Abstract
Background
To report a case of Suprachoroidal Hemorrhage followed by Swept-Source Optical Coherence Tomography.
Case presentation
A 66-year-old woman with a rhegmatogenous retinal detachment in her left eye underwent pars plana vitrectomy. During the intraocular photocoagulation for a retinal tear after fluid-air exchange, a vitreous hemorrhage and suprachoroidal hemorrhage (SCH) developed. The surgical incisions were closed after filling the vitreous cavity with silicone oil. Two weeks later, the hemolyzed hemorrhage was removed, and new silicone oil was injected. After the surgery, a low reflective region was detected near the macula in the swept-source optical coherence tomographic (SS-OCT) images. The low reflective region was caused by the residual hemorrhage. The size of the reflective region gradually decreased and was not present at 3 months. We conclude that SS-OCT can be used to follow the resolution of a suprachoroidal hemorrhage.
Conclusion
SS-OCT can be used to detect and follow the natural course of a suprachoroidal hemorrhage including the absorptive processes.
Similar content being viewed by others
Background
A suprachoroidal hemorrhage is a severe complication that can develop during intraocular surgery [1]. It is generally believed that a suprachoroidal hemorrhage develops after a disruption of the posterior ciliary arteries. Ocular hypertension, high myopia, glaucoma, age, high intraocular pressure, arterial sclerosis, diabetes, and aphakia have been reported as preoperative risk factors for developing a suprachoroidal hemorrhage [1]. The intraoperative risk factors are increasing venous return, high intraocular pressure, and vitreous prolapse [2].
The choroidal vessels can be weakened by these risk factors, and when high pressure or stress is applied to increase the transmural venous pressure, the choroidal vessels can be disrupted. These changes are considered to be the cause of a suprachoroidal hemorrhage. In severe cases, the size of the hemorrhage is rapidly increased accompanied by a prolapse of the vitreous and retina. If this happens, the prognosis for the visual acuity is poor. The incidence of a suprachoroidal hemorrhage is 1.9% after vitrectomy [3] and 0.2% after cataract surgery [1, 4].
A search of Medline did not extract any publications showing the course of a suprachoroidal hemorrhage documented by optical coherence tomography (OCT). We report our swept-source OCT (SS-OCT) findings obtained just after the development of a suprachoroidal hemorrhage to its resolution.
Case presentation
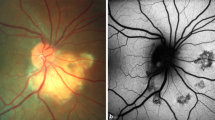
A 66-year-old woman with reduced vision in her left eye was examined in the Tokyo Medical and Dental University Hospital on June 27, 2015. Her best-corrected visual acuity (BCVA) in her left eye was 20/50, and both eyes were pseudophakic. The refractive error of the left eye was − 1.75 diopters, and the axial length was 25.89 mm. A rhegmatogenous retinal detachment (RRD) was detected by ophthalmoscopy and SS-OCT which extended over the inferotemporal quadrant including macula in her left eye (Fig. 1).
She underwent pars plana vitrectomy on the same day, and during the intraocular photocoagulation for a retinal tear, a sudden choroidal elevation and vitreous hemorrhage occurred. A suprachoroidal hemorrhage was also observed at the site of the trocar insertion. Although we intended to inject silicone oil into the vitreous cavity, a sufficient amount could not be injected because of an obstruction at the trocar insertion site. The surgery was terminated with a closure of the surgical incision.
On postoperative day 1, an elevated lesion was detected in the B-scan ultrasound images that was considered to be the suprachoroidal hemorrhage (Fig. 2).
The hemolyzed hemorrhage was removed by scleral fenestration on postoperative day 13. During the surgery, a reduction of choroidal elevation was observed. New silicone oil was injected after removing the original silicone oil.
Postoperatively, the resolution of the suprachoroidal hemorrhage was followed in the SS-OCT images (Fig. 3). However, the RRD on the inferior quadrant remained, and a scleral encircling procedure was performed on day 63, and silicone oil was reinjected to tamponade the retina. On day 73 after the RRD surgery, the retina was reattached, and the suprachoroidal hemorrhage was not present in the SS-OCT images.
SS-OCT images showing the resolution of a suprachoroidal hemorrhage. On postoperative day 26, a low reflective region can be seen in the suprachoroidal space (between arrowheads) in the SS-OCT image a day 26. This was considered to be a suprachoroidal hemorrhage. An elevation of the retina and choroid can be seen at the same region. The low reflective region (yellow arrows) and moderate reflective region (green arrows) are gradually absorbed and not present on postoperative day 73 b day 38, c day 56, d day 73. During the follow-up period, the RRD (white arrows) was still present, and an encircling procedure with silicone oil tamponade was performed on postoperative day 63. The hemorrhage was slowly absorbed and was not detected on postoperative day 73
At 3 months after the most recent surgery, the patient’s BCVA is 20/200, and the silicone oil was still present. A future surgery is planned to remove the silicone oil.
Discussion
This case report shows the process of a gradual absorption of a fresh hemorrhage in the suprachoroidal space by SS-OCT. A suprachoroidal hemorrhage is observed as low to moderate reflective regions in SS-OCT images. Generally, a subretinal hemorrhage is observed as high reflective region especially next to the retina in the OCT images [5]. We suggest that the low reflective region in our case was due to the hemolyzed liquid hemorrhage component and the moderate reflective region was the non-liquid component of the hemorrhage. It might be possible that the phase when the low reflective region is observed might be the appropriate timing for removing the suprachoroidal hemorrhage.
There are some diseases which shows the similar OCT findings to suprachoroidal hemorrhage, such as choroidal hemangioma, choroidal malignant melanoma, and choroidal nevus. The choroidal hemangioma exhibits a mottled high reflection image on the tumor surface due to the reflection of the blood vessel wall. The choroidal malignant melanoma/choroidal nevus exhibit an internal homogeneous low-reflection image similarly to suprachoroidal hemorrhage, but it is easy to distinguish the suprachoroidal hemorrhage from these diseases because of the specific course of the onset. In addition, the suprachoroidal location of the lesions is useful for making differential diagnosis from choroidal lesions.
Because of the deep penetration into tissues, SS-OCT is considered a powerful tool for the management of postoperative suprachoroidal hemorrhage. In spite of the limitation of a single case report, we believe it would be beneficial for clinicians to know the change of OCT findings in the course of the resolution of a suprachoroidal hemorrhage. Further studies including a larger number of patients are considered necessary to confirm the value of SS-OCT for a tool to visualize the course of this serious complication. In spite of the limitation of single case report, we believe it would be beneficial for clinicians to know the change of OCT findings in the course of the resolution of a suprachoroidal hemorrhage.
Conclusion
We conclude that SS-OCT can be used to detect and follow the natural course of a suprachoroidal hemorrhage including the absorptive processes.
Abbreviations
- BCVA:
-
Bbest-corrected visual acuity
- OCT:
-
Optical coherence tomography
- RRD:
-
Rhegmatogenous retinal detachment
- SS-OCT:
-
Swept-source OCT
References
Taylor DM. Expulsive hemorrhage: some observations and comments. Trans Am Ophthalmol Soc. 1974;72:157–69.
Tabandeh H, Sullivan PM, Smahliuk P, Flynn HW Jr, Schiffman J. Suprachoroidal hemorrhage during pars plana vitrectomy. Curr Opin Ophthalmol. 2001;12(3):179–85.
Piper JG, Han DP, Abrams GW, Mieler WF. Perioperative choroidal hemorrhage at pars plana vitrectomy. A case-control study. Ophthalmology. 1993;100(5):699–704.
Sekine Y, Takei K, Nakano H, Saotome T, Hommura S. Survey of risk factors for expulsive choroidal hemorrhage: case reports. Substantiation of the risk factors and their incidence. Ophthalmologica. 1996;210(6):344–7.
Zhao L, Ma W, Fariss RN, Wong WT. Minocycline attenuates photoreceptor degeneration in a mouse model of subretinal hemorrhage. Am J Pathol. 2011;179(3):1265–77.
Availability of data and materials
All the data supporting the conclusions of this article is included in the present article.
Author information
Authors and Affiliations
Contributions
HM and HT did the surgery, KU and NS and KS and KOM drafted the article and analyze the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Uramoto, K., Shimada, N., Takahashi, H. et al. Suprachoroidal hemorrhage followed by swept-source optical coherence tomography: a case report. BMC Ophthalmol 18, 203 (2018). https://doi.org/10.1186/s12886-018-0881-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-018-0881-4