Abstract
Background
Ubiquitous fungi of the Scedosporium apiospermum species complex (SASC) cause various opportunistic infections. Posterior subtenon triamcinolone acetonide (STTA) injection is a standard therapy for intraocular inflammation and macular edema. We report a case of Scedosporium apiospermum infectious scleritis after a posterior STTA injection.
Case presentation
A 75-year-old man received a posterior STTA injection to treat macular edema in his left eye. After 3 months, he complained of ocular pain and hyperemia in his left eye. Examination showed a subtenon abscess in the site corresponding with the STTA injection. After incising the abscess, the smear revealed numerous conidia-like structures. Although we suspected fungal infection and started topical voriconazole (VRCZ) and levofloxacin, the inflammation of the eye worsened. Fungal culture revealed filamentous fungus growth. Subsequently, we added systemic VRCZ and performed surgical debridement of the infected sclera and Tenon’s capsule. Pathology of the sclera showed fungal hyphae. The antifungal susceptibility test revealed low minimum inhibitory concentrations for micafungin, VRCZ and miconazole (0.06, 0.25 and 0.5 μg/mL, respectively). After 2 months, the ciliary injection subsided and VRCZ therapy was stopped. However, subtenon abscess recurred 1 month after discontinuation of topical VRCZ. Surgical debridement and topical VRCZ were resumed, with the eye finally improving after 5 months of management. The fungal species was identified as Scedosporium apiospermum sensu stricto morphologically and by DNA sequencing.
Conclusions
This case was successfully treated by topical and systemic VRCZ and repeated surgical debridement. Infectious scleritis caused by SASC rarely develops after posterior STTA. SASC can produce conidia in the enclosed subtenon space. Late-onset infectious scleritis after a posterior STTA injection suggests the presence of a fungal infection, including SASC, thereby requiring extensive and prolonged medical and surgical treatment.
Similar content being viewed by others
Background
Infectious scleritis is a rare condition that can develop after ocular trauma, ocular surgeries that include pterygium excision with β-radiation or mitomycin C, posterior subtenon triamcinolone acetonide (STTA) injection, or it can be due to extensions from an adjacent ocular infection [1]. Triamcinolone acetonide belongs to the class of drugs referred to as long-acting corticosteroids. Posterior STTA injections are used as a standard therapy for treating intraocular inflammation and macular edema following various ocular diseases including uveitis, diabetic retinopathy and branch retinal vein occlusion [2,3,4]. The outside of the sclera is covered with the Tenon’s capsule, which consists of loose connective tissue and is located beneath the bulbar conjunctiva [5]. Posterior STTA injection is a technique used to directly introduce drug into the subtenon space. Adverse effects of STTA include scleral perforation, cataract formation, glaucoma, endophthalmitis, infectious scleritis (also called periocular infection) and blepharoptosis [6, 7]. Infectious scleritis following posterior STTA is a rare complication that is caused by bacteria or fungi [8,9,10,11,12,13,14,15]. Here, we describe a case of infectious scleritis caused by Scedosporium apiospermum sensu stricto, which was successfully treated by topical and systemic voriconazole and surgical debridement of the infected sclera.
Case presentation
After a 75-year-old male, who pursued gardening as a hobby, noticed decreased vision in his left eye, he visited an ophthalmologist in September of 2015. He had a history of hypertension, colon cancer and metastatic hepatic tumor. As an ophthalmologic examination revealed macular edema in his left retina resulting from branch retinal vein occlusion (BRVO), he underwent a posterior STTA injection in his left eye to treat the macular edema. After routine disinfection of the lid margins and conjunctival sac with 10% and 0.625% (16-fold dilution) povidone iodine, respectively, the procedure was performed uneventfully. The patient once again visited his ophthalmologist in November due to complaints of ocular pain and hyperemia in his left eye. The symptoms did not improve even though he received oral and topical antibiotic treatment for 3 days. Computed tomography of the orbit was performed and revealed a peribulbar high density lesion of the left eyeball. Due to a suspected peribulbar infection, he was subsequently referred to our hospital in the middle of November.
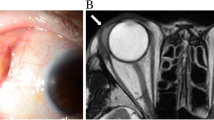
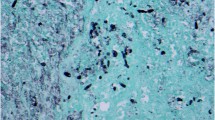
At his first visit, best corrected visual acuity (BCVA) (decimal) was 1.2 in the right eye and 0.15 in the left eye. Intraocular pressures were normal. Although the upper and lower eyelids of his left eye were swollen, we observed no restrictions of his eye movement. Slit lamp examination of the left eye showed ciliary injection, cells in the anterior chamber and a subtenon abscess in the superotemporal quadrant, which corresponded to the site of the posterior STTA (Fig. 1a). While our fundus examination did not reveal any intravitreal involvement, it did find macular edema and BRVO, which had been reported by his previous doctor. The right eye exhibited no abnormal findings, including both the anterior and posterior segments. The patient had no fever. The orbital magnetic resonance imaging (MRI) revealed the presence of a peribulbar high intensity lesion that corresponded to the subtenon abscess (Fig. 2). The MRI did not detect any paranasal sinus or intracranial invasion. The serologic test, which included white blood cells, C-reactive protein and beta-D-glucan, only revealed a slight elevation of C-reactive protein (1.11 mg/dL). To determine the causative pathogen, incision and drainage of the subtenon abscess were performed, with the obtained purulent fluid submitted for bacterial and fungal cultures. While the smears revealed polymorphonuclear leukocytes and a large number of round or oval conidia-like structures, a fungal filamentous appearance was not observed (Fig. 1b). Based on these results, we suspected fungal infectious scleritis induced by STTA. Therefore, the patient was initially started on 1% voriconazole (VRCZ) and 1.5% levofloxacin (LVFX) eye drops that were each administered six times per day in an outpatient department. Inflammation of the anterior chamber of the left eye worsened after 4 days, with choroidal detachment observed in the temporal region of the fundus. The fungal culture found an early colony of a filamentous fungus. Based on the definitive diagnosis of infectious scleritis by filamentous fungi, we then performed debridement of the infected sclera and Tenon’s capsule. The resected scleral tissue was submitted for further pathological examination. The conjunctival sac of the left eye was irrigated with 0.625% povidone iodine, followed by hospitalization for treatments with 1% natamycin ointment, 1% atropine eye drops and intravenous VRCZ. Ten days after the initial visit, we noted improvement in both his ocular pain and inflammation of the anterior chamber. As a result, we switched the voriconazole from an intravenous to an oral administration. Histopathological examination using Grocott staining revealed infiltration of branching hyphae into the sclera (Fig. 1c). Due to a novel subtenon abscess of the adjacent upper region of the left eyeball that developed at 18 days after the initial visit, we once again performed scleral debridement. The fungal species, Scedosporium apiospermum, was identified by DNA sequencing of the internal transcribed spacer (ITS) region of ribosomal DNA amplified by polymerase chain reaction (PCR) with ITS1F and ITS1R primers [16]. The strain was sent to Teikyo University for complete species identification. The susceptibility testing of the antifungal agents was performed using the broth microdilution method based on CLSI M38-A2 [17]. Results indicated low minimum inhibitory concentrations against micafungin, VRCZ and miconazole (Table 1). Based on the antifungal susceptibility test findings, the natamycin ointment was discontinued. Topical and systemic voriconazole administrations were continued for 2 and 1 months, respectively, and then stopped once the ciliary injection subsided. However, 1 month after the discontinuation of topical VRCZ, the subtenon abscess recurred at the same place (superotemporal quadrant). Incision and drainage of the abscess was performed three times. Light microscopic examination of the smears of the subtenon abscess revealed that septate hyphae were still present. As a result, we resumed the 1% VRCZ and 1.5% LVFX eye drops for 2 weeks and then stopped the administration. No recurrence was observed after the final treatment. Due to the prolonged macular edema, however, the final BCVA (decimal) of the left eye was 0.2 as of April 2016 (Fig. 1d).
Slit lamp microscopy of the left eye with right down gazing at the first examination (a) shows ciliary injection and a subtenon abscess in the superotemporal quadrant where the posterior STTA injection had been previously performed. The content of the subtenon abscess smear was Gram-stained and observed by light microscopy (b). A large amount of round or oval conidia-like structures and polymorphonuclear leukocytes were observed. A scleral specimen obtained by surgical debridement was histologically examined using Grocott staining (c). Branching hyphae stained with black were observed. A slit lamp microscope of the same view at the final examination shows that the subtenon abscess and ciliary injection were absent (d)
Characteristics of the colonies found on the potato dextrose agar incubated at 28 °C for 21 days included a grayish white and cottony appearance with an umbonate center on the surface, and a reverse side showing a brownish dark wrinkle appearance in the center and a yellow-white appearance on the margin (Fig. 3). Microscopic features observed when using the slide culture technique on potato dextrose agar at 10 days included septate hyphae that were 2 μm in diameter and branching irregularly, along with the production of lateral and terminal conidia, which were round or oval (3 to 5 by 5 to 10 μm) (Fig. 4a). We also observed a Graphium synanamorph that produced a brush of cylindrical conidia (3 by 12 μm) (Fig. 4b).
Microscopy of the slide culture on potato dextrose agar at 10 days revealed the presence of septate hyphae that were 2 μm in diameter. There was irregular branching of the hyphae with the production of round or oval (3 to 5 by 5 to 10 μm) lateral and terminal conidia (a). A Graphium synanamorph that produced a brush of cylindrical conidia (3 by 12 μm) was also observed (b)
In order to confirm the species identification using a molecular approach, the BUT locus of the β tubulin gene was also amplified by PCR using Bt1a/Bt1b primers [18, 19] and then applied to DNA sequencing [20, 21]. The obtained DNA sequencing was compared by using the Basic Local Alignment Search Tool. Both the ITS and the BUT exhibited 100% homology with that reported by Zouhair et al. for Scedosporium apiospermum (GenBank accession no. JQ690950 and JQ691056) [22]. Based on the current and previous results, we were finally able to identify the causative fungal strain as Scedosporium apiospermum sensu stricto.
Discussion
Here, we report a rare case of Scedosporium apiospermum infectious scleritis that developed after a posterior STTA injection. The treatment of infectious scleritis caused by filamentous fungi is challenging due to the difficulty of species identification and performing an antifungal drug susceptibility test, the small number of available antifungal agents, the poor drug delivery to the deep sclera, and the persistence of filamentous fungi. Additionally, scleral infections can cause the development of endophthalmitis due to direct invasion into the eyeball, thereby requiring enucleation [23, 24]. The early detection of the causative pathogen, Scedosporium apiospermum during the early stages in the current case made it possible to successfully treat the patient and save his vision. After the antifungal susceptibility test revealed the low MIC of VRCZ, repeated scleral debridement was able to effectively remove large amounts of the fungi, thereby improving drug delivery to the deep scleral lesion. It should be noted that the polyenes, such as amphotericin B, have exhibited limited in vitro activity against most strains of Scedosporium apiospermum [25]. Though initial treatment by only topical VRCZ was ineffective, the inflammation improved after addition of intravenous VRCZ. Therefore, not only topical but both topical and systemic VRCZ proved to be effective in this case, which was consistent with the in vitro susceptibility results.
Posterior STTA injection is one of the standard options for treating uveitis and macular edema [2,3,4]. Infectious scleritis (periocular infection) is a rare complication that occurs after posterior STTA injection, with a reported incidence of 0.04% [6]. Table 2 lists the previous reports of infectious scleritis after posterior STTA injections. The causative pathogens of the scleritis include bacteria and filamentous fungi. Generally, bacterial scleritis develops within 1 month, while fungal scleritis develops after 2 to 3 months (Table 2). Since 4 out of the 9 reported cases exhibited recurrences after a transient improvement, this suggests that these types of infections require not only extensive but also prolonged systemic and topical medical treatment especially for fungal scleritis [26]. All of the gram-positive cocci cases recovered after antibiotic treatment and exhibited good visual outcome. However, all of the fungal cases required surgical treatment including debridement for persistent scleral infection and pars plana vitrectomy for endophthalmitis secondary to infectious scleritis. When encountering late-onset infectious scleritis that is suspected to be fungal, surgical debridement should be considered in order to make a definitive diagnosis. Interestingly, 3 out of the 4 reported fungal cases were caused by either Scedosporium apiospermum or Pseudoallescheria boydii, although unlike in our current case, the processes used for species identification were not detailed in the other reports. Thus, these results suggest that Scedosporium apiospermum species complex is the dominant fungi that cause infectious scleritis after posterior STTA injection.
Scedosporium apiospermum is one of hyaline filamentous fungi that are ubiquitously present in soil, sewage and polluted water [25]. While it was previously considered to be the asexual state of Pseudallescheria boydii, it has now been shown to be two distinct species [27,28,29]. Presently, Scedosporium apiospermum is considered to be a species complex that is comprised of Scedosporium apiospermum sensu stricto, Scedosporium boydii, Scedosporium dehoogii, Scedosporium aurantiacum and Scedosporium minutisporum [27]. The fungal isolate in the current study was definitively identified as Scedosporium apiospermum sensu stricto through the use of DNA sequencing of the β-tubulin gene, which is currently the most reliable identification method for this genus [29, 30]. Scedosporium apiospermum species complex (SASC) are important opportunistic pathogens [25], as they can grow at 40 °C in most species [29, 31]. These pathogens can cause mycetoma, traumatic arthritis, prosthetic joint infection, catheter-related infection, near-drowning syndrome, osteomyelitis, otitis externa, pneumonia particular to cystic fibrosis patients, and ocular infections including keratitis, scleritis and endophthalmitis [31,32,33,34,35].
The most remarkable point in our current case was the unique microscopic finding of the smear of the subtenon abscess. This subtenon abscess smear showed numerous conidia, with the pathology of the resected sclera revealing branching hyphae (Fig. 1b, c). These findings imply that this fungus was introduced into the subtenon space by a previous posterior STTA injection, with hyphae then growing into the patient’s sclera and producing conidia asexually in the enclosed subtenon space. This is the first report on the characteristics of the cytology and the pathology of a subtenon abscess associated with the SASC.
Conclusions
We report a case of infectious scleritis that developed 3 months after a posterior STTA injection, with the isolates definitively identified as Scedosporium apiospermum sensu stricto. Surgical debridement combined with topical and systemic VRCZ administration effectively improved the infection and successfully saved the patient’s vision. This case report and the review of the literature imply that late-onset infectious scleritis after a posterior STTA injection strongly suggests the presence of a fungal infection, including SASC, thereby requiring extensive and prolonged medical and surgical treatment.
Abbreviations
- BCVA:
-
Best corrected visual acuity
- BRVO:
-
Branch retinal vein occlusion
- ITS:
-
Internal transcribed spacer
- LVFX:
-
Levofloxacin
- MIC:
-
Minimum inhibitory concentration
- MRI:
-
Magnetic resonance imaging
- PCR:
-
Polymerase chain reaction
- SASC:
-
Scedosporium apiospermum species complex
- STTA:
-
Subtenon triamcinolone acetonide
- VRCZ:
-
Voriconazole
References
Sainz de la Maza M, Biber JM, Schwam BL, Raizman MB. Scleritis. In: Mannis MJ, Holland EJ, editors. Cornea. Vol 1. Amsterdam, Elsevier; 2017. p. 1181–1194.
Bakri SJ, Kaiser PK. Posterior subtenon triamcinolone acetonide for refractory diabetic macular edema. Am J Ophthalmol. 2005;139:290–4.
Tanner V, Kanski JJ, Posterior FPA. Sub-Tenon’s triamcinolone injections in the treatment of uveitis. Eye (Lond). 1998;12(Pt 4):679–85.
Helm CJ, Holland GN. The effects of posterior subtenon injection of triamcinolone acetonide in patients with intermediate uveitis. Am J Ophthalmol. 1995;120:55–64.
Nishida T, Saika S, Morishige N. Cornea and sclera: anatomy and physiology. In: Mannis MJ, Holland EJ, editors. Cornea, vol. 1. Amsterdam: Elsevier; 2017. p. 1–22.
Sakamoto T, Hida T, Tano Y, Negi A, Takeuchi S, Ishibashi T, et al. Survey of triamcinolone acetonide for ocular diseases in Japan. Nippon Ganka Gakkai Zasshi. 2007;111:936–45.
Leder HA, Jabs DA, Galor A, Dunn JP, Thorne JE. Periocular triamcinolone acetonide injections for cystoid macular edema complicating noninfectious uveitis. Am J Ophthalmol. 2011;152:441–8.
Gharaee H, Khalife M, Poor SS, Abrishami M. Infectious scleritis after subtenon triamcinolone acetonide injection. Ocul Immunol Inflamm. 2011;19:284–5.
Ikewaki J, Imaizumi M, Nakamuro T, Motomura Y, Ohkusu K, Shinoda K, et al. Peribulbar fungal abscess and endophthalmitis following posterior subtenon injection of triamcinolone acetonide. Acta Ophthalmol. 2009;87:102–4.
Seth RK, Gaudio PA. Nocardia Asteroides necrotizing scleritis associated with subtenon triamcinolone acetonide injection. Ocul Immunol Inflamm. 2008;16:139–40.
Oh IK, Baek S, Huh K, Oh J. Periocular abscess caused by Pseudallescheria boydii after a posterior subtenon injection of triamcinolone acetonide. Graefes Arch Clin Exp Ophthalmol. 2007;245:164–6.
Kusaka S, Ikuno Y, Ohguro N, Hori Y, Tano Y. Orbital infection following posterior subtenon triamcinolone injection. Acta Ophthalmol Scand. 2007;85:692–3.
Isshiki Y, Kimura T, Yokoyama M, Kimura W, Syoge K, Ryu M, et al. Case of fungal endophthalmitis developed after subtenon injections of triamcinolone acetonide. Nippon Ganka Gakkai Zasshi. 2007;111:741–4.
Azarbod P, Mohammed Q, Akram I, Moorman C. Localised abscess following an injection of subtenon triamcinolone acitonide. Eye (Lond). 2007;21:672–4.
Engelman CJ, Palmer JD, Egbert P. Orbital abscess following subtenon triamcinolone injection. Arch Ophthalmol. 2004;122:654–5.
Todokoro D, Yamada N, Fukuchi M, Kishi S. Topical voriconazole therapy of Purpureocillium lilacinum keratitis that occurred in disposable soft contact lens wearers. Int Ophthalmol. 2014;34:1159–63.
CLSI. M38-A2 reference method for broth dilution antifungal susceptibility testing of filamentous fungi; approved standard. 2nd ed. Wayne: Clinical and Laboratory Standards Institute; 2008.
Makimura K. Molecular detection and identification for mycosis-fungal DNA extraction method. Med Mycol J. 2013;54:329–32.
Glass NL, Donaldson GC. Development of primer sets designed for use with the PCR to amplify conserved genes from filamentous ascomycetes. Appl Environ Microbiol. 1995;61:1323–30.
Chen M, Zeng J, De Hoog GS, Stielow B, Gerrits Van Den Ende AH, Liao W, et al. The ‘species complex’ issue in clinically relevant fungi: a case study in Scedosporium apiospermum. Fungal Biol. 2016;120:137–46.
Lackner M, Klaassen CH, Meis JF, van den Ende AH, de Hoog GS. Molecular identification tools for sibling species of Scedosporium and Pseudallescheria. Med Mycol. 2012;50:497–508.
Zouhair R, Rougeron A, Razafimandimby B, Kobi A, Bouchara JP, Giraud S. Distribution of the different species of the Pseudallescheria boydii/Scedosporium apiospermum complex in French patients with cystic fibrosis. Med Mycol. 2013;51:603–13.
Belenitsky MP, Liu C, Tsui I. Scedosporium apiospermum endopthalmitis treated early with intravitreous voriconazole results in recovery of vision. J Ophthalmic Inflamm Infect. 2012;2:157–60.
McGuire TW, Bullock JD, Bullock JD Jr, Elder BL, Fungal FJW. Endophthalmitis. An experimental study with a review of 17 human ocular cases. Arch Ophthalmol. 1991;109:1289–96.
Cortez KJ, Roilides E, Quiroz-Telles F, Meletiadis J, Antachopoulos C, Knudsew T, et al. Infections caused by Scedosporium spp. Clin Microbiol Rev. 2008;21:157–97.
Reddy JC, Murthy SI, Reddy AK, Garg P. Risk factors and clinical outcomes of bacterial and fungal scleritis at a tertiary eye care hospital. Middle East Afr J Ophthalmol. 2015;22:203–11.
Huguenin A, Noel V, Rogez A, Chemla C, Villena I, Toubas D. Scedosporium apiospermum otitis complicated by a temporomandibular arthritis: a case report and mini-review. Mycopathologia. 2015;180:257–64.
Lackner M, de Hoog GS, Yang L, Moreno LF, Ahmed SA, Andreas F, et al. Proposed nomenclature for Pseudallescheria, Scedosporium and related genera. Fungal Divers. 2014;67:1–10.
Gilgado F, Cano J, Gene J, Sutton DA, Guarro J. Molecular and phenotypic data supporting distinct species statuses for Scedosporium apiospermum and Pseudallescheria boydii and the proposed new species Scedosporium dehoogii. J Clin Microbiol. 2008;46:766–71.
Gilgado F, Cano J, Gene J, Guarro J. Molecular phylogeny of the Pseudallescheria boydii species complex: proposal of two new species. J Clin Microbiol. 2005;43:4930–42.
Atlas of Clinical Fungi, Version 4.1.4 [database on the Internet]. Centraalbureau voor Schimmelcultures. Available from: http://atlas.clinicalfungi.org/. Accessed: 11/21/2017.
Jutley G, Koukkoulli A, Forbes J, Sharma V. Unusual case of Scedosporium apiospermum keratitis following phacoemulsification in a systemically well patient. J Cataract Refract Surg. 2015;41:230–3.
Hayashi Y, Eguchi H, Toibana T, Mitamura Y, Yaguchi T. Polymicrobial sclerokeratitis caused by Scedosporium apiospermum and Aspergillus cibarius. Cornea. 2014;33:875–7.
Jhanji V, Yohendran J, Constantinou M, Sheorey H, Vajpayee RB. Scedosporium scleritis or keratitis or both: case series. Eye Contact Lens. 2009;35:312–5.
Chen FK, Chen SD, Tay-Kearney ML. Intravitreal voriconazole for the treatment of endogenous endophthalmitis caused by Scedosporium apiospermum. Clin Exp Ophthalmol. 2007;35:382–5.
Acknowledgements
Not applicable.
Funding
Not applicable.
Availability of the data and materials
All data have been presented within the manuscript and in the form of images.
Author information
Authors and Affiliations
Contributions
DT is responsible for acquisition of the clinical information and writing up of the manuscript. JH is responsible for contributing to and reviewing the manuscript. AY and KM are responsible for identification of the fungal isolate. JH is responsible for pathological diagnosis of the patient. HA is responsible for reviewing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
This study followed the tenets of the Declarations of Helsinki. Written informed consent was obtained from the participants.
Consent for publication
Written informed consent for the publication of the case details was obtained from the patient in this case report. A copy of written consent is available for review by the Executive Editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Todokoro, D., Hoshino, J., Yo, A. et al. Scedosporium apiospermum infectious scleritis following posterior subtenon triamcinolone acetonide injection: a case report and literature review. BMC Ophthalmol 18, 40 (2018). https://doi.org/10.1186/s12886-018-0707-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-018-0707-4