Abstract
Background
The aim of this study is to report a case of cystoid macular oedema (CME) associated with Rosai–Dorfman Disease (RDD).
Case presentation
A 52-year-old male initially presented with a two-month history of a congested left eye. At presentation, visual acuity was 20/20 in the right eye and 20/80 in the left eye. Biomicroscopy showed conjunctival hyperaemia in the left eye with a slight elevation, suggesting a subconjunctival mass. Retinal fluorescein angiography and optical coherence tomography (OCT) revealed the presence of CME in the left eye. A clinical examination revealed nodular lesions in the ears and a lump in the subcutaneous tissue of the left arm. A biopsy of the subcutaneous lesion showed histological and immunohistochemical characteristics of RDD. The patient was treated with intravitreal triamcinolone (0.1 mL/4 mg). One month after treatment, there was complete regression of the oedema with a significant improvement in visual acuity to 20/20.
Conclusions
This is the first reported case of RDD associated with cystoid macular oedema. Macular oedema responded to intravitreal treatment with triamcinolone.
Similar content being viewed by others
Background
Rosai–Dorfman disease (RDD), or sinus histiocytosis with massive lymphadenopathy, was first described by Destombes [1] in 1965. Four years later, Rosai and Dorfman [2] characterized RDD as a distinct clinicopathological disorder based on four cases. Patients with this rare and nonmalignant disorder often present with painless cervical lymphadenopathy, fever, and leukocytosis. RDD often manifests in the lymph nodes of the head and neck but may also be present in extranodal sites, such as the skin, conjunctiva, upper respiratory tract, and bone. Ocular involvement is relatively rare (8.5%) and usually manifests as lymphoproliferation in the soft tissues of the orbit and eyelid [3].
In the following report, we describe the first case of cystoid macular oedema (CME) associated with RDD.
Case presentation
A 52-year-old male initially presented with a two-month history of congestion of the left eye.
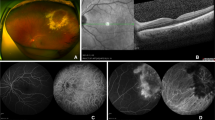
At presentation, he underwent a complete ophthalmic examination. Visual acuity was 20/20 in the right eye and 20/80 in the left eye. Biomicroscopy showed conjunctival hyperaemia in the left eye with a slight elevation, suggesting a subconjunctival mass (Fig. 1a), but no intraocular inflammatory reaction was noted. The bilateral intraocular pressures were both 10 mmHg. No signs of inflammatory cells were noted in the anterior chamber or the vitreous, and no signs of retinal vasculitis were identified on biomicroscopy and ophthalmoscopy examination with mydriasis. However, the presence of an abnormality in the foveal reflex in the left eye was observed. A clinical examination revealed nodular lesions in the ears (Fig. 1b) and a lump in the subcutaneous tissue of the left arm.
A biopsy of the subcutaneous lesion showed a cellular infiltrate in the superficial and deep dermis with histiocytes with phagocytized lymphocytes and plasma cells (Fig. 2a). A characteristic finding was the presence of lymphocytes engulfed within the histiocytic cytoplasm, a feature called emperipolesis (Fig. 2b) [1]. Immunohistochemically, the large histiocytes reacted strongly with antibodies to S-100 protein, CD68, and CD 20b. These three immunohistochemical markers are indicative of a mixed inflammatory or heterogeneous population of cells that are characteristic of RDD. Retinal fluorescein angiography in the left eye revealed petaloid leakage from the perifoveal retinal capillaries during the late phases without staining of the optic disc. Optical coherence tomography (OCT) revealed well-defined, intraretinal cystic areas of low reflectivity in the macula in the left eye, which are characteristic signs of cystoid macula oedema (CME). (Fig. 3b).
Due to the low visual acuity secondary to CME, the patient was treated intravitreally with triamcinolone (4 mg/0.1 mL). One month later, the patient showed significant improvement in visual acuity (20/20) and OCT showed complete regression of the oedema (Fig. 3c). The follow-up time was 6 months, and during this period, there was no recurrence of the oedema.
Discussion and Conclusions
RDD (sinus histiocytosis with massive lymphadenopathy) often presents as a painless bilateral cervical lymphadenopathy with systemic symptoms. Consists of a rare disease, non-hereditary, benign histiocytic proliferative disorder. The Extranodal impairment have been reported in 28–43% of cases with rare ocular involvement [4].
The characteristic findings of RDD include emperipolesis, positive histiocyte staining for S100 and CD68, and negative staining for CD1a. There is no standardized protocol available for treatment of ocular RDD because of its rarity and the possibility of its spontaneous regression [2, 5]. Excisional biopsy is often performed for diagnosis and treatment, and there is usually no recurrence after this procedure [6].
Extradonal impairment has been reported in 28–43% of cases, with locations including the skin, upper respiratory tract, salivary glands, epidural space, bone, and ocular adnexa. Ocular manifestation is rare. In the largest series of 243 cases as described by Foucar in 1990, the eye was involved in 36 cases (8.5%) and was highly associated with nasal sinus involvement. Infiltration of the soft tissues of the orbit and eyelids was the most common manifestation of ocular involvement [5, 7]. In addition, infiltration of the lacrimal system, conjunctiva, subconjunctiva, cornea, uveal tract, and optic nerve were also reported [8,9,10,11,12,13,14].
Uveitis was present in three isolated cases of anterior uveitis (5,7,8,12) involving one patient with coexistent corneal infiltration [13], one patient with coexistent papilledema [14], one patient with bilateral subconjunctival masses [15], one patient with bilateral serous retinal detachment [16], and one patient with uveitic glaucoma [17].
To the best of our knowledge, this is the first report of macular oedema associated with RDD. The patient also presented with a subconjunctival mass and dermatologic abnormalities in the arm and ear. There was a prompt clinical response to intravitreal treatment with triamcinolone, suggesting a probable inflammatory cause of the macular oedema as previously reported in other forms of ocular involvement, such as chronic uveitis and uveitic glaucoma [12, 17].
The short follow-up time of 6 months was a limitation of this study, particularly with regard to drawing conclusions regarding the efficacy of long-term therapy.
In summary, RDD can be associated with CME; therefore, RDD patients should undergo routine eye examinations.
Abbreviations
- CME:
-
Cystoid macular oedema
- OCT:
-
Optical coherence tomography
- RDD:
-
Rosai–Dorfman disease
References
Diebold J, Tixier P, Baufine-Ducrocq H, Tricot G, Verger JP, Wierzbicki N. Lymphadenopathy caused by hemophagocytic sinus histiocytosis (Destombes-Rosai-Dorfman syndrome). Immunologic and histopathologic study of a new case. Ann Anat Pathol (Paris). 1976 Jul-Sep;21(3):347–56.
Lam-My S, Weiller PJ, Dor AM, Lebreuil G, Michel-Bechet M, Mongin M Benign pseudo-tumoral lymphoid hyperplasia with massive Destombes-Rosai-Dorfman histiocytosis.Sem Hop. 1981 Mar 8–15;57(9–10):458-460.
Tran HM, Chinichian S, Storkersen K, Tokuhara K, Tran K, et al. An unusual case of extranodal Rosai-Dorfman disease manifesting as an epibulbar mass. Case Rep Ophthalmol. 2015;6:351–5.
Yilmaz S, Ture M, Maden A, Tunakan M. Extranodal Rosai-Dorfman disease with bilateral orbital involvement: Report of a case treated with systemic steroid alone. Clin Ophthalmol. 2008;2:479–81.
Foucar E, Rosai J, Dorfman RF. The ophthalmologic manifestations of sinus histiocytosis with massive lymphadenopathy. Am J Ophthalmol. 1979;87:354–67.
Fernandes BF, Brazuna A, Moura LR, et al. Extranodal Rosai-Dorfman disease presenting as an epibulbar tumor. Cornea. 2008;27:378–81.
Foucar E, Rosai J, Dorfman RF, Eyman JM. Immunologic abnormalities and their significance in sinus histiocytosis with massive lymphadenopathy. Am J Clin Pathol. 1984 Nov;82(5):515–25.
Berger C, Gakt J, Allansmith MR. Globe involvement in sinus histiocytosis. Am J Ophthalmol. 1983 Jan;95(1):124–5.
Karcioglu Z, Allam B, Sinsler M. Ocular involvement in sinus histiocytosis with mass lymphadenopathy. Br J Ophthalmol. 1988;72:793–5.
Stopak A, Dreizen N, Zimmerman L, O'Neill JF. Sinus histiocytosis presenting as an epibulbar mass. Arch Ophthalmol. 1988;106:1426–8.
Ireland KC, Hutchinson AK, Grossniklaus HE. Sinus histiocytosis presenting as bilateral epibulbar masses. Am J Ophthalmol. 1999;127:360–1.
Silvestre JF, Aliaga A. Cutaneous sinus histiocytosis and chronic uveitis. Pediatr Dermatol. 2000;17:377–80.
Rumelt S, Cohen I, Rehany U. Marginal corneal infiltrates: a possible new manifestation of sinus histiocytosis with massive lymphadenopathy. Cornea. 2000;19:857–8.
Shukla E, Nicholson A, Agrawal A, Rathod D. Extra Nodal Rosai-Dorfman Disease (Sinus Histiocytosis with Massive Lymphadenopathy) Presenting as Asymmetric Bilateral Optic Atrophy : An Atypical Ocular Presentation. Head Neck Pathol. 2016;10(3):414-7.
Cavuoto K, Galor A, Dubovy SR, Gregori N, McCarthy M. Subconjunctival masses associated with central nervous system rosai-dorfman disease. Cornea. 2011;30(2):237-40.
Meyer CH, Sel S, Hörle S, Burg J, Kroll P. Rosai-Dorfman disease with bilateral serous retinal detachment. Arch Ophthalmol. 2003;121:733–5.
MacLaren RE, Hundal KS, Trittibach P, Bloom PA. Uveitic glaucoma and Rosai-Dorfman disease (sinus histiocytosis). Ocul Immunol Inflamm. 2006;14:305–7.
Acknowledgements
We acknowledge the contribution of Prof. Dr. Fernando Chahud Augusto for the pathological analyses of this clinical case.
The data on the declarations can be obtained at the Department of Ophthalmology, Otorhinolaryngology and Head and Neck Surgery, Ribeirao Preto School of Medicine, University of Sao Paulo, Sao Paulo, Brazil through the link below:
Funding
No funding was obtained for this study.
Availability of data and materials
All of the data supporting our findings are contained within the manuscript.
Author information
Authors and Affiliations
Contributions
Literature screening, selection, and preparation and review of the manuscript were performed by RCS and AAVC. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Institutional Review Board/Ethics Committee of the Clinical Hospital of Ribeirao Preto-SP Brazil approved the intravitreal use of drugs for special cases that do not respond to clinical treatment. This study was performed in accordance with the tenets of the Declaration of Helsinki.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Siqueira, R.C., e Cruz, A.A.V. Cystoid macular oedema associated with Rosai–Dorfman disease: a case report. BMC Ophthalmol 17, 141 (2017). https://doi.org/10.1186/s12886-017-0538-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-017-0538-8