Abstract
Background
FOLFOXIRI plus bevacizumab is used as a first-line therapy for patients with unresectable or metastatic colorectal cancer. However, there are no clear recommendations for second-line therapy after FOLFOXIRI plus bevacizumab combination. Here, we describe our planning for the EFFORT study to investigate whether FOLFIRI plus aflibercept has efficacy following FOLFOXIRI plus bevacizumab for mCRC.
Methods
EFFORT is an open-label, multicenter, single arm phase II study to evaluate whether a FOLFIRI plus aflibercept has efficacy following FOLFOXIRI plus bevacizumab for mCRC. Patients with unresectable or metastatic colorectal cancer who received FOLFOXIRI plus bevacizumab as a first-line therapy will receive aflibercept and FOLFIRI (aflibercept 4 mg/kg, irinotecan 150 mg/m2 IV over 90 min, with levofolinate 200 mg/m2 IV over 2 h, followed by fluorouracil 400 mg/m2 bolus and fluorouracil 2400 mg/m2 continuous infusion over 46 h) every 2 weeks on day 1 of each cycle. The primary endpoint is progression-free survival (PFS). To achieve 80% power to show a significant response benefit with a one-sided alpha level of 0.10, assuming a threshold progression-free survival of 3 months and an expected value of at least 5.4 months, we estimated that 32 patients are necessary. Secondary endpoints include overall survival, overall response rate, safety, and exploratory biomarker analysis for differentiating anti-VEGF drug in 2nd-line chemotherapy for unresectable or metastatic colorectal cancer.
Discussion
This is the first study to investigate whether FOLFIRI plus aflibercept has efficacy following FOLFOXIRI plus bevacizumab for unresectable or metastatic colorectal cancer. Switching to a different type of anti-VEGF drug in second-line therapy after FOLFOXIRI plus bevacizumab appears to be an attractive treatment strategy when considering survival benefit. It is expected that this phase II study will prove the efficacy of this strategy and that a biomarker for drug selection will be discovered.
Trial registration
Japan Registry of Clinical Trials jRCTs071190003. Registered April 18, 2019.
Similar content being viewed by others
Background
One of the goals in chemotherapy for unresectable/metastatic colorectal cancer (mCRC) is to prolong survival and maintain quality of life by controlling the disease through exposure to all active agents in an appropriate sequence of administration. Nine different classes of drugs have shown antitumor activity in mCRC: fluoropyrimidines, irinotecan, oxaliplatin, anti-epidermal growth factor receptor (EGFR) antibodies, anti-vascular endothelial growth factor (VEGF) drugs, regorafenib, trifluridine/tipiracil (FTD/TPI, TAS-102), encorafenib for BRAF V600E mutant mCRC, and immunotherapy for microsatellite instability-high/deficient mismatch repair (MSI-H/dMMR) mCRC. Chemotherapy is usually performed with a combination of cytotoxic drugs and a molecular target drug such as anti-VEGF drug or anti-EGFR antibody. A cytotoxic DOUBLET combination of fluorouracil (5-FU) plus levofolinate (l-LV) and either oxaliplatin (FOLFOX) or irinotecan (FOLFIRI) with a molecular target drug is generally proposed as initial systemic chemotherapy; recently, however, a TRIPLET combination of fluorouracil plus levofolinate, oxaliplatin and irinotecan (FOLFOXIRI) showed superior efficacy in terms of tumor shrinkage and survival benefit compared with the DOUBLET combination.
The TRIBE study showed that FOLFOXIRI plus bevacizumab (BEV) is a promising regimen in first–line therapy for patients with mCRC [1], and this regimen is now regarded as a recommended first-line therapy for patients whose treatment goal is tumor shrinkage and in patients with BRAF mutant tumors. However, a second-line therapy after FOLFOXIRI plus BEV treatment has not been well established. The TRIBE2 study showed that after maintenance treatment with 5-FU/ l-LV plus BEV, re-introduction of FOLFOXIRI plus BEV offered the most favorable survival benefit [2]. However, most patients who receive an oxaliplatin-based regimen experience peripheral sensory neuropathy. Therefore, FOLFIRI plus BEV appears to be the most commonly used regimen for second-line therapy after FOLFOXIRI plus BEV [1]. Although FOLFIRI plus BEV may be suitable as a standard regimen for second-line therapy, all of the drugs in this regimen are included in first-line FOLFOXIRI plus BEV; accordingly, a response to FOLFIRI plus BEV would not be expected following the failure of first-line FOLFOXIRI plus BEV. Recently, two new anti-VEGF drugs - aflibercept [3] and ramucirumab [4] - showed promising anti-tumor effects as second-line treatment when combined with a FOLFIRI-based regimen for patients with mCRC. FOLFOXIRI plus BEV, or its maintenance phase - 5-FU/ l-LV plus BEV, does not include aflibercept, and thus this drug might provide additional benefit to patients who have progressed after FOLFOXIRI plus BEV.
To investigate this possibility, we planned a phase II EFFORT study to investigate whether FOLFIRI plus aflibercept has efficacy following FOLFOXIRI plus BEV treatment. Here, we describe the protocol for the phase II EFFORT study.
Methods/design
Study design and treatment
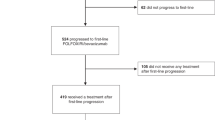
The EFFORT study is an open-label, multicenter, single arm phase II study to evaluate whether FOLFIRI plus aflibercept has efficacy following FOLFOXIRI plus BEV for mCRC in patients with unresectable or metastatic colorectal cancer. The study has been approved by a central review board and is currently ongoing at 47 medical facilities in Japan. The main inclusion criteria are histologically confirmed advanced mCRC, known RAS mutation status (known BRAF mutation status also, if possible), mCRC treated with FOLFOXIRI plus BEV as first-line therapy for at least two courses, adjuvant chemotherapy and FOLFOXIRI plus BEV treatment for recurrence, age ≥ 20 years, ECOG PS 0 or 1, measurable lesions based on the Response Evaluation Criteria in Solid Tumors (RECIST) guidelines version 1.1, adequate organ function, and sufficient oral ingestion function. Complete inclusion and exclusion criteria are shown in Table 1. RAS and BRAF testing are performed locally.
Patients receive aflibercept and FOLFIRI (aflibercept 4 mg/kg, irinotecan 150 mg/m2 IV over 90 min, with l-LV 200 mg/m2 IV over 2 h, followed by 5-FU 400 mg/m2 bolus and 5-FU 2400 mg/m2 continuous infusion over 46 h) every 2 weeks on day 1 of each cycle. Patients receive premedication with antiemetic agents according to institutional guidelines. Treatment continues until disease progression, unacceptable toxicity, death, patient refusal, or investigator decision. When irinotecan is stopped due to severe diarrhea or other adverse events, irinotecan can be skipped, in which case 5-FU/l-LV plus aflibercept or aflibercept alone can be administered. When aflibercept is missed due to an adverse event, FOLFIRI, irinotecan alone, or 5-FU/l-LV can be administered, and such treatments are also within the protocol treatment. There is no prescribed treatment following completion or discontinuation of protocol treatment. Planned enrollment period is 2019 April to 2021 March, and the observation period will include a 2-year follow-up period from the time the last patient is enrolled. No interim analysis of this study will be performed.
Endpoints and assessments
The primary objective of this trial is to determine whether the FOLFIRI plus aflibercept regimen has efficacy following FOLFOXIRI plus BEV in patients with mCRC in terms of progression-free survival (PFS). Secondary endpoints are overall response rate (ORR), overall survival (OS) and safety.
Disease assessment is performed every 6 weeks by computed tomography (CT). Response is determined by CT scanning based on Response Evaluation Criteria in Solid Tumors version 1.1. PFS is defined as the time from study enrollment to first disease progression or death, whichever occurs first; OS is defined as the time from study enrollment to the date of death due to any cause; and ORR is defined as the percentage of patients relative to the total of enrolled subjects who achieve a complete response (CR) or partial response (PR) based on CT scan images.
All adverse events (AEs) observed during the study treatment period are appropriately registered in the subjects’ medical records and in electronic case reports forms. All serious adverse events (SAEs), namely fatal or life-threatening adverse events or those requiring hospitalization or resulting in persistence or significant disability/incapacity, are required to be disclosed by the investigator to the KSCC (Kyushu Study group of Clinical Cancer) Study Office/Enrollment and Data Analysis Center within 24 h. AEs will be assessed according to the Common Terminology Criteria for Adverse Events version 5.0.
Plasma levels of placental growth factor (PlGF), vascular endothelial growth factor-A (VEGF-A), vascular endothelial growth factor-B (VEGF-B), vascular endothelial growth factor-C (VEGF-C), vascular endothelial growth factor-D (VEGF-D), and interleukin-8 (IL-8) are assessed in blood samples collected from each patient before the protocol treatment, prior to first imaging evaluation, and within 30 days after treatment discontinuation to identify biomarkers that predict the efficacy of aflibercept. This analysis aims to identify a potential predictive biomarker for the efficacy of FOLFIRI plus aflibercept treatment.
Target sample size and statistical analyses
The primary endpoint of this study is PFS. Second-line PFS with a FOLFIRI-based regimen after FOLFOXIRI/BEV is considered to be shorter than second-line PFS after FOLFOX/BEV due to treatment resistance to irinotecan. According to the TRIBE-2 trial, the second-line PFS of FOLFIRI/BEV after FOLFOX/BEV was 5.6 months [2]. Furthermore, a phase 2 trial of FOLFIRI plus aflibercept conducted in Japan showed its PFS as 5.4 months (95% CI, 4.14–6.70) [5]. Based on these results, the expected PFS value in this study was set at 5.4 months. To achieve 80% power to show a significant response benefit with a one-sided alpha level of 0.10, and assuming a threshold PFS of 3 months, we estimated that 32 patients would be necessary. Considering dropouts, a total of 35 patients would need to be enrolled.
The following hypothesis will be tested using the confidence intervals for median survival time as defined by Brookmeyer and Crowley. Sample size calculation was performed using SAS ver.9.4 (Cary, NC, USA).
Discussion
A survival benefit for anti-EGFR antibody in 2nd-line chemotherapy has not been shown even in the case of RAS wild-type mCRC [6,7,8,9]. In contrast, the combination of an anti-VEGF drug and doublet combination has shown a survival effect [3, 4, 10, 11], and an anti-VEGF drug is therefore usually selected in combination with second-line chemotherapy for mCRC. While bevacizumab, aflibercept and ramucirumab are currently used as anti-VEGF drugs [3, 4, 12], no biomarker or definite criteria for selection of these drugs is available, and no data for second-line therapy after FOLFOXIRI plus BEV as pretreatment have been reported.
Attempts to discover a molecular predictive biomarker for anti-VEGF drugs have not led to clinically useful findings, although several studies are currently underway. The acquisition of resistance to BEV in patients with mCRC may involve BEV-induced cytokine changes and high VEGF-A, −D and placental growth factor (PlGF) serum levels [13,14,15,16]. Following biomarker analysis of the RAISE trial (NCT01183780), ramucirumab is likely to be added to second-line FOLFIRI for patients with high VEGF-D levels. However, ramucirumab has been reported to show negative effects when administered to patients with low VEGF-D levels equivalent to the one-third of normal levels seen after first-line treatment with a bevacizumab-containing oxaliplatin-based regimen for mCRC [17]. In contrast, a biomarker post hoc analysis of the VELOUR trial (NCT00561470) reported that aflibercept retains its activity regardless of baseline VEGF-A and PlGF levels [18]. The GI-SCREEN CRC-Ukit study, a prospective longitudinal study to investigate an association between plasma angiogenesis-related mediators and clinical outcomes in mCRC, suggested that changes in VEGF-D and PlGF occurred independently, and it may be possible to select drugs by assessing these alterations [19].
Furthermore, regarding the effects of these anti-VEGF drugs, the usefulness of second-line treatment after administration of FOLFOXIRI plus BEV as pretreatment has not been reported. Moreover, the desirability of switching to a different type of anti-VEGF drug in subsequent treatment following BEV as pretreatment remains unclear.
FOLFOXIRI plus BEV showed significant superiority to DOUBLET plus BEV as initial systemic chemotherapy for patients with mCRC in terms of survival benefit and tumor shrinkage [1, 2, 20]. Subgroup analyses also indicated that FOLFOXIRI plus BEV is remarkably effective in patients with poor prognosis, such as those with BRAF mutations, extrahepatic metastases or a right-sided primary [1, 20]. Patients with mCRC who receive FOLFOXRI plus BEV as initial systemic chemotherapy may therefore expect an aggressive therapeutic combination as a subsequent regimen. Aflibercept uniquely targets both VEGF-A and PlGF, with higher affinity for both than other anti-angiogenic therapies, and VEGF-A and PlGF bind aflibercept with higher affinity than their native receptor [21]. These findings suggest that tumors progressing under blockade of a single anti-angiogenic therapy, such as BEV, most likely use numerous non-VEGF-A mechanisms to sustain their growth. Switching to a different therapy to target these alternative mechanisms, such as aflibercept, may be beneficial. Although differences in study design and patient characteristics hamper decision-making from cross-trial comparisons, aflibercept plus FOLFIRI combination showed an attractive ORR and survival benefit for patients with mCRC compared to BEV and ramucirumab as second-line therapy (Table 2). This study uses comparison with historical controls to investigate biomarkers able to predict the effects of aflibercept, and to determine the desirability of switching to a different type of anti-VEGF drug for second-line therapy following FOLFOXIRI therapy as pretreatment.
Availability of data and materials
Not applicable.
Abbreviations
- 5-FU:
-
5-Fluorouracil
- AE:
-
Adverse event
- BEV:
-
Bevacizumab
- CRC:
-
Colorectal cancer
- CT:
-
Computed tomography
- ECOG:
-
Eastern Cooperative Oncology Group
- EGFR:
-
Epidermal growth factor receptor
- FOLFIRI:
-
5-fluorouracil+levofolinate calcium+irinotecan
- FOLFOX:
-
5-fluorouracil+levofolinate calcium+oxaliplatin
- FOLFOXIRI:
-
5-fluorouracil+levofolinate calcium+oxaliplatin+irinotecan
- IRI:
-
irinotecan
- l-LV:
-
Levofolinate calcium
- mCRC:
-
Unresectable/metastatic colorectal cancer
- NCCN:
-
National Comprehensive Cancer Network
- ORR:
-
Overall response rate
- OS:
-
Overall survival
- OX:
-
Oxaliplatin
- PD:
-
Progressive disease
- PFS:
-
Progression-free survival
- PS:
-
Performance status
- VEGF:
-
Vascular endothelial growth factor
References
Loupakis F, Cremolini C, Masi G, Lonardi S, Zagonel V, Salvatore L, Cortesi E, Tomasello G, Ronzoni M, Spadi R, et al. Initial therapy with FOLFOXIRI and bevacizumab for metastatic colorectal cancer. N Engl J Med. 2014;371(17):1609–18.
Cremolini C, Antoniotti C, Rossini D, Lonardi S, Loupakis F, Pietrantonio F, Bordonaro R, Latiano TP, Tamburini E, Santini D, et al. Upfront FOLFOXIRI plus bevacizumab and reintroduction after progression versus mFOLFOX6 plus bevacizumab followed by FOLFIRI plus bevacizumab in the treatment of patients with metastatic colorectal cancer (TRIBE2): a multicentre, open-label, phase 3, randomised, controlled trial. Lancet Oncol. 2020;21(4):497–507.
Van Cutsem E, Tabernero J, Lakomy R, Prenen H, Prausova J, Macarulla T, Ruff P, van Hazel GA, Moiseyenko V, Ferry D, et al. Addition of aflibercept to fluorouracil, leucovorin, and irinotecan improves survival in a phase III randomized trial in patients with metastatic colorectal cancer previously treated with an oxaliplatin-based regimen. J Clin Oncol. 2012;30(28):3499–506.
Tabernero J, Yoshino T, Cohn AL, Obermannova R, Bodoky G, Garcia-Carbonero R, Ciuleanu TE, Portnoy DC, Van Cutsem E, Grothey A, et al. Ramucirumab versus placebo in combination with second-line FOLFIRI in patients with metastatic colorectal carcinoma that progressed during or after first-line therapy with bevacizumab, oxaliplatin, and a fluoropyrimidine (RAISE): a randomised, double-blind, multicentre, phase 3 study. Lancet Oncol. 2015;16(5):499–508.
Denda T, Sakai D, Hamaguchi T, Sugimoto N, Ura T, Yamazaki K, Fujii H, Kajiwara T, Nakajima TE, Takahashi S, et al. Phase II trial of aflibercept with FOLFIRI as a second-line treatment for Japanese patients with metastatic colorectal cancer. Cancer Sci. 2019;110(3):1032–43.
Cunningham D, Humblet Y, Siena S, Khayat D, Bleiberg H, Santoro A, Bets D, Mueser M, Harstrick A, Verslype C, et al. Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal cancer. N Engl J Med. 2004;351(4):337–45.
Hecht JR, Cohn A, Dakhil S, Saleh M, Piperdi B, Cline-Burkhardt M, Tian Y, Go WY. SPIRITT: a randomized, multicenter, phase II study of Panitumumab with FOLFIRI and Bevacizumab with FOLFIRI as second-line treatment in patients with Unresectable wild type KRAS metastatic colorectal Cancer. Clin Colorectal Cancer. 2015;14(2):72–80.
Peeters M, Price TJ, Cervantes A, Sobrero AF, Ducreux M, Hotko Y, Andre T, Chan E, Lordick F, Punt CJ, et al. Randomized phase III study of panitumumab with fluorouracil, leucovorin, and irinotecan (FOLFIRI) compared with FOLFIRI alone as second-line treatment in patients with metastatic colorectal cancer. J Clin Oncol. 2010;28(31):4706–13.
Sobrero AF, Maurel J, Fehrenbacher L, Scheithauer W, Abubakr YA, Lutz MP, Vega-Villegas ME, Eng C, Steinhauer EU, Prausova J, et al. EPIC: phase III trial of cetuximab plus irinotecan after fluoropyrimidine and oxaliplatin failure in patients with metastatic colorectal cancer. J Clin Oncol. 2008;26(14):2311–9.
Giantonio BJ, Catalano PJ, Meropol NJ, O'Dwyer PJ, Mitchell EP, Alberts SR, Schwartz MA, Benson AB 3rd. Eastern cooperative oncology group study E: Bevacizumab in combination with oxaliplatin, fluorouracil, and leucovorin (FOLFOX4) for previously treated metastatic colorectal cancer: results from the eastern cooperative oncology group study E3200. J Clin Oncol. 2007;25(12):1539–44.
Kubicka S, Greil R, Andre T, Bennouna J, Sastre J, Van Cutsem E, von Moos R, Osterlund P, Reyes-Rivera I, Muller T, et al. Bevacizumab plus chemotherapy continued beyond first progression in patients with metastatic colorectal cancer previously treated with bevacizumab plus chemotherapy: ML18147 study KRAS subgroup findings. Ann Oncol. 2013;24(9):2342–9.
Bennouna J, Sastre J, Arnold D, Osterlund P, Greil R, Van Cutsem E, von Moos R, Vieitez JM, Bouche O, Borg C, et al. Continuation of bevacizumab after first progression in metastatic colorectal cancer (ML18147): a randomised phase 3 trial. Lancet Oncol. 2013;14(1):29–37.
Alidzanovic L, Starlinger P, Schauer D, Maier T, Feldman A, Buchberger E, Stift J, Koeck U, Pop L, Gruenberger B, et al. The VEGF rise in blood of bevacizumab patients is not based on tumor escape but a host-blockade of VEGF clearance. Oncotarget. 2016;7(35):57197–212.
Kopetz S, Hoff PM, Morris JS, Wolff RA, Eng C, Glover KY, Adinin R, Overman MJ, Valero V, Wen S, et al. Phase II trial of infusional fluorouracil, irinotecan, and bevacizumab for metastatic colorectal cancer: efficacy and circulating angiogenic biomarkers associated with therapeutic resistance. J Clin Oncol. 2010;28(3):453–9.
Loupakis F, Cremolini C, Fioravanti A, Orlandi P, Salvatore L, Masi G, Di Desidero T, Canu B, Schirripa M, Frumento P, et al. Pharmacodynamic and pharmacogenetic angiogenesis-related markers of first-line FOLFOXIRI plus bevacizumab schedule in metastatic colorectal cancer. Br J Cancer. 2011;104(8):1262–9.
Willett CG, Duda DG, di Tomaso E, Boucher Y, Ancukiewicz M, Sahani DV, Lahdenranta J, Chung DC, Fischman AJ, Lauwers GY, et al. Efficacy, safety, and biomarkers of neoadjuvant bevacizumab, radiation therapy, and fluorouracil in rectal cancer: a multidisciplinary phase II study. J Clin Oncol. 2009;27(18):3020–6.
Tabernero J, Hozak RR, Yoshino T, Cohn AL, Obermannova R, Bodoky G, Garcia-Carbonero R, Ciuleanu TE, Portnoy DC, Prausova J, et al. Analysis of angiogenesis biomarkers for ramucirumab efficacy in patients with metastatic colorectal cancer from RAISE, a global, randomized, double-blind, phase III study. Ann Oncol. 2018;29(3):602–9.
Van Cutsem E, Paccard C, Chiron M, Tabernero J. Impact of prior Bevacizumab treatment on VEGF-A and PlGF levels and outcome following second-line Aflibercept treatment: biomarker post hoc analysis of the VELOUR trial. Clin Cancer Res. 2020;26(3):717–25.
Taniguchi H, Yuki S, Shiozawa M, Masuishi T, Nishina T, Kagawa Y, Takahashi N, Yasui H, Denda T, Sunakawa Y, et al. Plasma VEGF-D and PlGF levels according to prior use of biologics among metastatic colorectal cancer: preliminary results from GI-SCREEN CRC-Ukit study. J Clin Oncol. 2020;38(no. 4_suppl):178.
Cremolini C, Loupakis F, Antoniotti C, Lupi C, Sensi E, Lonardi S, Mezi S, Tomasello G, Ronzoni M, Zaniboni A, et al. FOLFOXIRI plus bevacizumab versus FOLFIRI plus bevacizumab as first-line treatment of patients with metastatic colorectal cancer: updated overall survival and molecular subgroup analyses of the open-label, phase 3 TRIBE study. Lancet Oncol. 2015;16(13):1306–15.
Papadopoulos N, Martin J, Ruan Q, Rafique A, Rosconi MP, Shi E, Pyles EA, Yancopoulos GD, Stahl N, Wiegand SJ. Binding and neutralization of vascular endothelial growth factor (VEGF) and related ligands by VEGF trap, ranibizumab and bevacizumab. Angiogenesis. 2012;15(2):171–85.
Acknowledgements
This trial is supported by KSCC Study Office/Enrollment and Data Analysis Center.
Editorial assistance/English editing was provided by Guy Harris of DMC Corp.
Funding
The EFFORT study is being funded by Sanofi Pharmaceutical Co., Ltd. The sponsor had no control over the interpretation, writing, or publication of this paper.
Author information
Authors and Affiliations
Contributions
EO and KA are the principal investigators, and are responsible for the trial design and study procedures. HS, KA EO AM and HS form the Protocol Committee. HS is responsible for recruitment and patient information. MS is responsible for statistical analysis. HS, EO KA, MS, AT and MM drafted and revised the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study is being conducted in accordance with the Good Clinical Practice guidelines and the guiding principles detailed in the Declaration of Helsinki, and in keeping with applicable local law(s) and regulation(s).
Written informed consent to study procedures must be provided by all candidate patients before enrolment. We have registered this study in the Japan Registry of Clinical Trials with registration number jRCTs071190003. Before initiation, the principal investigator was required to consult the Certified Review Board (Kyushu University Certified Institutional Review Board for Clinical Trials: Certification No. CRB718005) and receive approval from the study site’s manager, and to submit a trial plan to the Minister of Health, Labor and Welfare.
Consent for publication
Not applicable.
Competing interests
The EFFORT study is being funded by Sanofi Pharmaceutical Co., Ltd.
Hironaga Satake receives honoraria from Sanofi Co., Ltd. and Yakult Honsha Co., Ltd.
Eiji Oki receives honoraria from Yakult Honsha Co., Ltd.
All remaining authors have declared no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Satake, H., Ando, K., Oki, E. et al. Protocol of the EFFORT study: a prospective study of FOLFIRI plus aflibercept as second-line treatment after progression on FOLFOXIRI plus bevacizumab or during maintenance treatment in patients with unresectable/metastatic colorectal cancer. BMC Cancer 20, 1116 (2020). https://doi.org/10.1186/s12885-020-07576-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-020-07576-9