Abstract
Background
Increasing studies have demonstrated that activated platelets play an essential role in tumour progression. However, the level and prognostic role of platelet indices in chordoma patients remain unclear. The aim of the current study was to characterize the prognostic performance of platelet count (PLT), mean platelet volume (MPV) and platelet distribution width (PDW) in skull base chordoma patients.
Methods
187 primary skull base chordoma patients between January 2008 and September 2014 were enrolled in this retrospective study. The optimal cut-off values were determined by X-tile software, and the correlations between PLT, MPV, PDW and clinicopathological features were further analysed. Kaplan-Meier curve and Cox regression analysis were used for survival analysis.
Results
The values of preoperative PTL, MPV and PDW ranged from 104 to 501 × 109/L, 6.7 to 14.2 fl, and 7.8 to 26.2%, respectively. Elevated PLT was associated with larger tumour volume (p = 0.002). Kaplan-Meier survival analysis revealed that increased MPV and PDW were associated with shorter overall survival (p = 0.022 and 0.008, respectively). Importantly, multivariate Cox analysis demonstrated that elevated PDW was an independent unfavourable predictive factor for overall survival (hazard ratio (HR), 2.154, 95% confidence interval (CI), 1.258–3.688, p = 0.005).
Conclusions
Our data show that elevated MPV and PDW are associated with poor outcomes in skull base chordoma and that PDW may be helpful to identify patients with high risk.
Similar content being viewed by others
Background
Skull base chordoma is a slow-growing cancer of the bone system originating from notochord remnants, with a morbidity of less than 1 per million and a slight preference of male patients [1, 2]. The current first choice of treatment for skull base chordoma patients remains complete surgical resection with recommended postoperative proton-beam therapy [3, 4]. However, the therapy of skull base chordoma patients is still challenging owing to the difficulty of radical resection, subsequent local recurrence, resistance to classical chemoradiotherapy and limited value of targeted therapy [1, 5]. The identification of effective prognostic markers for potential risk stratification and to better select individual treatment strategies are urgently needed to prolong the life span and reduce the financial burden of skull base chordoma patients.
Increasing evidence indicates that platelets derived from megakaryocytes play an essential role in the tumour initiation, development and metastasis through several aspects such as tumour cell growth and invasion, abnormal angiogenesis, and inflammatory process [6, 7]. Moreover, activated platelets are closely correlated with cancer-associated thrombosis via interactions with tumour cells, neutrophils and monocytes. Recent studies revealed that increased platelet count (PLT) was observed in various cancers and it was closely associated with poor outcomes in colorectal cancer [8], non-small cell lung cancer [9], glioblastoma [10] and epithelial ovarian carcinoma [11], indicating the potential role of anti-platelet therapy in comprehensive cancer therapy.
Mean platelet volume (MPV), an index characterizing the size of platelets, is a valuable indicator of platelet activation and changes in platelet production [12, 13]. In addition, preoperative MPV was found to be elevated in various cancer patients compared to that in healthy people, and it has been recognized as a useful diagnostic marker in various diseases, including malignancies, cardiovascular disease and stroke [12]. Moreover, further studies indicate that MPV can act as an effective prognostic indicator for outcome in patients with cancers such as esophageal squamous cell cancer and colorectal cancer [14]. Platelet distribution width (PDW), another platelet associated indicator evaluating the coefficient of variation in platelet dimension, is considered a hallmark of platelet morphology and is widely used for the differential diagnosis of thrombocytopenia [15]. Besides, an increasing numbers of studies have revealed that PDW is elevated in cancer patients and can independently predict patient survival in various malignancies [16, 17].
However, to our knowledge, few studies have evaluated the preoperative levels and prognostic roles of these platelet-associated indexes in skull base chordoma until now. Thus, the current study aimed to characterize the preoperative levels of PLT, MPV and PDW and explore their correlations in primary skull base chordoma patients. We also assessed the relationships of PLT, MPV, and PDW with clinical factors and patient outcome in skull base chordoma.
Methods
Study population and data collection
This retrospective study analysed skull base chordoma patients who received operations at Beijing Tiantan Hospital from January 2008 to September 2014. Patients with histopathologically confirmed skull base chordoma and no history of preoperative radiotherapy or chemotherapy were included. Patients with any of the following conditions were excluded: (1) fuzzy pathological diagnosis; (2) incomplete clinical data and/or preoperative laboratory tests; (3) history of preoperative treatment (operation, chemoradiotherapy); (4) evidence of other malignancies, infection, inflammation or autoimmune disease, haematological disease or blood transfusion; and (5) unavailable follow up information. Accordingly, 187 primary skull base chordoma patients were included in the study. The ethical committee of Beijing Tiantan Hospital approved the current study and informed consent was received from the enrolled patients.
The clinicopathological data of each patient including age at diagnosis, patient sex, symptoms, pathological type, tumour size, tumour texture and blood supply, brainstem involvement, posterior cranial nerve involvement and preoperative laboratory tests containing PLT (109/L), MPV (fl), and PDW (%) were acquired from medical records. The extent of resection was assessed as total resection or non-total resection according to the pre- and postoperative image examinations [18].
Patients’ treatment and follow up
All patients were treated with surgical resection (endoscopic endonasal approach for 73 patients, endoscopic transoral approach for 6 patients, transcranial approach for 108 patients), and no patients received exclusive radiotherapy alone. For patients with a non-total resection, postoperative adjuvant radiotherapy was recommended.
Survival data were acquired from each patient via regular follow up, and the last time of follow up was October 2019. Patients were periodically followed up at the interval of 3 to 6 months for the first 2 years after the operation, and then annually. Clinical examinations and contrast-enhanced MRI were routinely used at each follow-up time. Overall survival (OS), calculated as the time between the date of tumour resection to the date of death or the last follow-up, was used for survival analysis. The mean follow up time was 72.41 months (range, 3–141 months; median, 74 months).
Definition of cutoff values for PLT, MPV and PDW
X-tile 3.6.1 software (Yale University, New Haven, CT, USA) was used to find the optimal cutoff values of each index for OS analysis [19]. In brief, the patients were divided into two groups according to certain values, and a subsequent log-rank test comparing the two groups was performed. The value with the minimum p value was defined as the best cutoff value.
Statistical analysis
All statistical analyses were conducted by SPSS 19.0 software (IBM, Armonk, NY, USA) and GraphPad Prism (Version 7.0, GraphPad, La Jolla, CA, USA) was used for graph construction. Continuous variables were listed as the median or mean ± standard deviation, and categorical variables were expressed as the frequency. The chi-square test was used for comparisons between categorical variables. Correlations between PLT MPV and PDW were analysed using Pearson correlation. The Kaplan-Meier method and subsequent log-rank test were used for OS analysis between groups. Variables with a p value < 0.05 in univariate Cox analysis were enrolled in multivariate Cox analysis to evaluate independence. Statistical significance was considered if the p value was less than 0.05 in 2-sided tests.
Results
Summary of patients
Patient descriptive characteristics are reported in Table 1. A total of 187 skull base chordoma patients meeting the inclusion criteria were enrolled in this retrospective study, including 98 males and 89 females with a mean (± SD) age at diagnosis of 40.1 (± 15.3) years old. Tumour volumes varied from 1740.5 to 258,024.6 mm3 (mean ± SD, 31729.8 ± 33,238.5). The most common symptoms of skull base chordoma patients were headache (88 patients), diplopia (68 patients), and blurred vision (61 patients). Fifty-seven patients had soft tumours and the other 130 patients had hard/moderate tumor. A total of 109 patients had a rich tumor blood supply, and 78 patients with poor/moderate tumour blood supply. The numbers of patients with classical, chondroid and dedifferentiated chordoma were 126, 61, and 0, respectively. A total of 118 patients had brainstem involvement, and 69 patients had posterior cranial nerve involvement. Regarding surgical outcome, 41 patients received total resection and the remaining 146 patients received non-total resection (Fig. 1). 72 patients received postoperative radiotherapy. Among them, 42 (58.3%) patients received the gamma knife; 8 (11%) patients received proton beam therapy; 6 (8.3%) patients received other forms of radiotherapy (1 carbon ion therapy, 1 cyberknife, and 4 intensity modulated radiotherapy); and the detailed forms of radiotherapy were unknown in 16 (22.2%) patients (Table 1).
Representative preoperative and postoperative MR images showing the definition of total and non-total resection, as well as the value of combined treatment. a-d preoperative and postoperative images of one case who received total resection and the patient got no recurrence during the follow up. e-h preoperative and postoperative images of another case who received non-total resection and following adjuvant radiotherapy. i-j After surgery and postoperative adjuvant radiotherapy, the case shown in e-h had no sign of recurrence on the 70 months follow up images
PLT, MPV, and PDW levels in skull base chordoma patients
The median (range) levels of PTL, MPV and PDW were 234 (104–501) × 109/L, 10.2 (6.7–14.2) fl, and 11.8 (7.8–26.2) %, respectively (Table 1). We then used X-tile software to find the optimal cutoff value of each index, and the cutoff values of PLT, MPV and PDW were 266, 11.9 and 14.5, respectively (see Additional file 1). Accordingly, the patients were divided into two groups for further analysis: 142 (75.9%) patients with PLT ≥266 and 45 (24.1%) patients with PLT < 266; 165 (88.2%) patients in the MPV ≥11.9 group and 22 (11.8%) patients in the MPV < 11.9 group; and 156 (83.4%) patients with PDW ≥14.5 and 31 (16.6%) patients with PDW < 14.5.
Relationships between PLT, MPV, and PDW and clinical variables
We also analysed the correlations between PLT, MPV, and PDW and clinical parameters. As shown in Table 2, only higher PLT (PLT ≥266) was associated with larger tumour volume (p = 0.002). No significant differences were found between PLT, MPV, and PDW and clinicopathological features including patient sex, age at diagnosis, pathological types, tumour texture, tumour blood supply, brainstem involvement and posterior cranial nerve involvement. Of note, patients with high PLT tended to have tumours with rich blood supply (p = 0.098). Additionally, a larger tumour volume seemed to be more common in patients with PDW ≥14.5 (p = 0.108).
We then analysed the potential correlation among PLT, MPV and PDW. Our results indicated that PDW was negatively correlated with PLT (r = − 0.344, p < 0.001), however, a strong positive correlation was observed between PDW and MPV (r = 0.844, p < 0.001).
Analysis of the association of PLT, MPV and PDW with patient outcomes
A total of 72 (38.5%) patients died during the follow-up, and the 5-year OS rate was 68.4% in the current study. Kaplan-Meier analysis demonstrated a shorter OS time (mean OS time, 82.3 months, 5-year OS rate, 62.1%) in the PLT ≥266 group than that in the PLT < 266 group (mean OS time, 102.7 months; 5-year OS rate, 75.8%), though the p value was 0.115 (Fig. 2a). For MPV, patients with MPV ≥11.9 had a worse OS (mean OS time, 77.7 months; 5-year OS rate, 59.1%) than patients with MPV < 11.9 (mean OS time, 103.0 months; 5-year OS rate, 74.36%) (p = 0.022, Fig. 2b). Moreover, the OS time of patients with PDW ≥14.5 (mean OS time, 78.2 months; 5-year OS rate 58.1%) was significantly shorter than that of patients with PDW < 14.5 (mean OS time, 104.2 months; 5-year OS rate 75.6%) (p = 0.008, Fig. 2c).
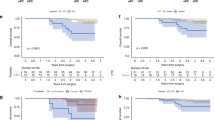
Further subgroup analysis of different tumour pathologies showed that higher PLT (p = 0.671, Fig. 3a) showed no prognostic value in classical chordoma patients, while higher MPV (p = 0.003, Fig. 3b) and PDW (p = 0.009, Fig. 3c) were associated with poor OS in the classical chordoma subgroup. Conversely, for chondroid chordoma patients, higher PLT (p = 0.011, Fig. 3d) rather than higher MPV (p = 0.524, Fig. 3e) or PDW (p = 0.941, Fig. 3f) was associated with a shorter OS time. In addition, for patients with different tumour volumes, the differences between the different PLT, MPV and PDW groups were not significant in tumour volume ≤ 20,000 mm3 patients (p = 0.489, p = 0.696, p = 0.496, respectively). The OS between the different PLT groups showed no significance (p = 0.376); however, MPV (p = 0.006) and PDW (p = 0.007) still showed prognostic value in patients with tumour volume > 20,000 mm3 (Fig. 4).
Kaplan-Meier curves of PLT, MPV and PDW in different pathological types of skull base chordoma. a OS analysis of PLT in classical chordoma patients. b OS analysis of MPV in classical chordoma patients. c OS analysis of PDW in classical chordoma patients. d OS analysis of PLT in chondroid chordoma patients. e OS analysis of MPV in chondroid chordoma patients. f OS analysis of PDW in chondroid chordoma patients. PLT, platelet count; MPV, mean platelet volume; PDW, platelet distribution width; OS, overall survival
Kaplan-Meier curves of PLT, MPV and PDW in skull base chordoma with different tumor volumes. a OS analysis of PLT in tumor volume ≤ 20,000 mm3 patients. b OS analysis of MPV in tumor volume ≤ 20,000 mm3 patients. c OS analysis of PDW in tumor volume ≤ 20,000 mm3 patients. d OS analysis of PLT in tumor volume > 20,000 mm3 patients. e OS analysis of MPV in tumor volume > 20,000 mm3 patients. f OS analysis of PDW in tumor volume > 20,000 mm3 patients. PLT, platelet count; MPV, mean platelet volume; PDW, platelet distribution width; OS, overall survival
Univariate Cox analysis revealed that age at diagnosis (hazard ratio (HR), 1.852; 95% confidence interval (CI), 1.072–3.198; p = 0.027), tumour volume (HR, 1.697; 95% CI, 1.056–2.728; p = 0.029), tumour blood supply (HR, 0.523; 95% CI, 0.314–0.870; p = 0.013), tumour pathology type (HR, 0.493; 95% CI, 0.283–0.861; p = 0.013), degree of resection (HR, 3.390; 95% CI, 1.552–7.405; p = 0.002), tumour recurrence (HR, 9.549; 95% CI, 3.482–26.183; p < 0.001), MPV (HR, 1.957; 95% CI, 1.090–3.514; p = 0.025) and PDW (HR, 2.013; 95% CI, 1.191–3.405; p = 0.009) were associated with poor OS, while PLT showed no significance (p = 0.119). To identify potential independent factors, further multivariate Cox analysis including these 8 variables was carried out, and the results showed that PDW (HR, 2.154; 95% CI, 1.258–3.688; p = 0.005), age at diagnosis (HR, 1.791; 95% CI, 1.023–3.315; p = 0.042), degree of resection (HR, 2.585; 95% CI, 1.172–5.704; p = 0.019) and tumour recurrence (HR, 7.460; 95% CI, 2.701–20.599; p < 0.001) were independent indicators of OS (Table 3).
Discussion
To our knowledge, this study was first to evaluate the prognostic role of preoperative platelet associated indexes (PLT, MPV and PDW) in skull base chordoma. Our data demonstrated that preoperative MPV and PDW rather than PLT were associated with patient OS. Multivariate Cox analysis indicated that high PDW (PDW ≥14.5) was an independent prognostic indicator of survival in skull base chordoma patients. In addition, our data confirmed that tumour recurrence and degree of resection were associated with OS [1, 20,21,22]. Our data revealed that MPV and PDW may be practical clinical biomarkers for prognosis in skull base chordoma due to the easy availability and relative affordability in daily clinical practice.
Platelets were identified to be involved in the process of tumour progression by numerous researches, however, the prognostic value of PLT remains disputable in different cancers, even in patients with the same kind of tumours [6, 23]. Increasing studies have indicated that an elevated preoperative PLT was associated with unfavourable prognosis in lung cancer, hepatocellular carcinoma and colorectal cancer [9, 24], however, some studies found that a lower PLT rather than a higher PLT predicted poor survival in hepatocellular carcinoma [25, 26]. This inconsistency may be explained by different cutoff values of PLT, differences in the follow-up time, potential selection bias of the study population, and tumour heterogeneity [27]. In the current study, similar to previous studies identifying PLT as a risk factor for survival, our data revealed that patients with preoperative PLT ≥266 tended to have a shorter OS time than patients with PLT < 266 (mean OS time, 82.3 months versus 102.7 months), indicating the potential relation between high PLT and poor outcome in skull base chordoma, though the p value between groups was > 0.05. Additional studies assessing the prognostic performance of PLT in skull base chordoma, and research exploring whether PLT is increased in skull base chordoma patients compared to healthy controls are highly warranted.
Interestingly, changes in MPV and PDW in patients with dissimilar tumours seemed controversial as well. Preoperative MPV and PDW were found to be increased and serve as risk factors for survival in various malignancies, including colorectal cancers and stomach cancers [12]. However, several researches showed that MPV was decreased in non-small-cell lung cancer patients, and subsequent survival results showed that MPV could act as a protective factor for patient outcomes [28]. In addition, a study indicated that PDW was decreased in breast cancer patients compared to controls, though patients with relatively high PDW were still associated with inferior outcomes [29]. In this study, our data indicated that preoperative MPV ≥11.9 and PDW ≥14.5 were associated with unfavourable OS in skull base chordoma patients, and PDW ≥14.5 was further identified as an effective independent prognostic indicator for OS, although MPV failed to be statistically significant in the multivariable Cox model. Further exploration of this conflict may deepen our understanding of the clinical implications and mechanisms of platelet-associated indicators in cancer patients.
The underlying mechanisms of elevated PLT, MPV and PDW levels in tumour progression remain to be elucidated. Increased PLT and platelet activation induced by the secretion of cytokines from tumour cells is associated with hypercoagulable state and thrombosis in patients, which are tightly associated with shorter survival [30]. In addition, tumour cells can escape the tumour immunity with the help of the hypercoagulable microenvironment and physical barrier by thrombosis [6]. Increased PLT can promote CD40 ligand production and contribute to the inflammatory response [31], and the inflammatory response participates in tumourigenesis and tumour development through several aspects, such as the induction of reactive oxygen species and subsequent DNA damage, promotion of tumour cell growth and angiogenesis via the secretion of various cytokines and enhanced tumour cell adhesion, and the induction of potential tumour micrometastasis [32]. In addition, platelet-derived growth factor (PDGF) family secreted by platelets plays a vital role in cell proliferation and invasion via binding to its respective receptors [33], and recent studies have revealed that PDGF receptor B is significantly expressed and associated with unfavourable outcome in skull base chordoma [34, 35]. Moreover, vascular endothelial growth factor (VEGF), which is secreted by platelet, contributes to tumour angiogenesis and serves as a predictor of tumor progression in chordoma patients receiving sorafenib [36]. MPV and PDW were considered as indicators of platelet activation [17, 37], and previous studies reported that the aberrance of MPV and PDW levels may be correlated with megakaryocyte dysfunction, heterogeneous demarcation and abnormal bone marrow haematopoietic system [38], and the release of inflammatory cytokines, including interleukin-6 and several colony stimulating factors such as granulocyte colony stimulating factors, by tumour cells can regulate megakaryocytic maturation and subsequent platelet synthesis and size [39]. As an essential proinflammatory mediator, interleukin-6 has been identified to promote oncogenesis by regulation of tumour cells survival, metabolism and angiogenesis [40]. We thus hypothesized that skull base patients with high MPV or PDW may have aberrant levels of cytokines such as interleukin-6 and abnormal inflammatory responses, leading to tumour progression and poor outcomes [32]. Interesting, several cytokines including interleukin-6 and tumor necrosis factor-alpha were reported to be elevated in chordoma patients [41, 42], suggesting the potential role of cytokines in chordoma progression. We will explore the levels and prognostic values of these cytokines in skull base chordoma, and their association with platelet associated indexes in the future study.
Some limitations exist in the current study. Considering the character of a single-centre retrospective study, additional large-scale, multicentre prospective studies are needed to verify our results and whether platelet is a potential therapeutic target for chordoma. In addition, the current study lacks mechanism studies explaining how these indexes affect the clinical outcomes of chordoma patients. Finally, the prognostic roles of other platelet indices and postoperative platelet-associated indictors, such as P-selectin [43] and postoperative PDW [44] in skull base chordoma were not analysed.
Conclusions
Our data reveal that high levels of MPV and PDW are associated with poor OS in skull base chordoma patients. Importantly, PDW could independently predict patient outcomes, suggesting that PDW may act as a useful prognostic biomarker. In addition, our findings reveal the potential value of platelet-associated therapy in skull base chordoma.
Availability of data and materials
All data used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PLT:
-
Platelet count
- MPV:
-
Mean platelet volume
- PDW:
-
Platelet distribution width
- OS:
-
Overall survival
- PDGF:
-
Platelet-derived growth factor
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
References
Walcott BP, Nahed BV, Mohyeldin A, Coumans J-V, Kahle KT, Ferreira MJ. Chordoma: current concepts, management, and future directions. Lancet Oncol. 2012;13(2):e69–76.
Chambers KJ, Lin DT, Meier J, Remenschneider A, Herr M, Gray ST. Incidence and survival patterns of cranial chordoma in the United States. Laryngoscope. 2014;124(5):1097–102.
Williams BJ, Raper DM, Godbout E, Bourne TD, Prevedello DM, Kassam AB, et al. Diagnosis and treatment of chordoma. J Natl Compr Cancer Netw. 2013;11(6):726–31.
Stacchiotti S, Sommer J. Building a global consensus approach to chordoma: a position paper from the medical and patient community. Lancet Oncol. 2015;16(2):e71–83.
Stacchiotti S, Longhi A, Ferraresi V, Grignani G, Comandone A, Stupp R, et al. Phase II study of imatinib in advanced chordoma. J Clin Oncol. 2012;30(9):914–20.
Mezouar S, Frère C, Darbousset R, Mege D, Crescence L, Dignat-George F, et al. Role of platelets in cancer and cancer-associated thrombosis: experimental and clinical evidences. Thromb Res. 2016;139:65–76.
Buergy D, Wenz F, Groden C, Brockmann MA. Tumor–platelet interaction in solid tumors. Int J Cancer. 2012;130(12):2747–60.
Long Y, Wang T, Gao Q, Zhou C. Prognostic significance of pretreatment elevated platelet count in patients with colorectal cancer: a meta-analysis. Oncotarget. 2016;7(49):81849.
Dangfan Y, Bingjiang L, Lizhen Z, Kaiqi D. Platelet count predicts prognosis in operable non-small cell lung cancer. Exp Ther Med. 2013;5(5):1351–4.
Brockmann MA, Giese A, Mueller K, Kaba FJ, Lohr F, Weiss C, et al. Preoperative thrombocytosis predicts poor survival in patients with glioblastoma. Neuro-oncology. 2007;9(3):335–42.
Li AJ, Madden AC, Cass I, Leuchter RS, Lagasse LD, Karlan BY. The prognostic significance of thrombocytosis in epithelial ovarian carcinoma. Gynecol Oncol. 2004;92(1):211–4.
Pyo J-S, Sohn JH, Kang G. Diagnostic and prognostic roles of the mean platelet volume in malignant tumors: a systematic review and meta-analysis. Platelets. 2016;27(8):722–8.
Yuri Gasparyan A, Ayvazyan L, Mikhailidis DP, Kitas GD. Mean platelet volume: a link between thrombosis and inflammation? Curr Pharm Des. 2011;17(1):47–58.
Li N, Yu Z, Zhang X, Liu T, Sun Y-X, Wang R-T, et al. Elevated mean platelet volume predicts poor prognosis in colorectal cancer. Sci Rep. 2017;7(1):1–6.
Kaito K, Otsubo H, Usui N, Yoshida M, Tanno J, Kurihara E, et al. Platelet size deviation width, platelet large cell ratio, and mean platelet volume have sufficient sensitivity and specificity in the diagnosis of immune thrombocytopenia. Br J Haematol. 2005;128(5):698–702.
Zhang X, Cui M-M, Fu S, Li L-L, Liu Y-S, Liu Z-P, et al. Platelet distribution width correlates with prognosis of gastric cancer. Oncotarget. 2017;8(12):20213.
Li N, Diao Z, Huang X, Niu Y, Liu T, Liu Z-P, et al. Increased platelet distribution width predicts poor prognosis in melanoma patients. Sci Rep. 2017;7(1):1–6.
Gui S, Zong X, Wang X, Li C, Zhao P, Cao L, et al. Classification and surgical approaches for transnasal endoscopic skull base chordoma resection: a 6-year experience with 161 cases. Neurosurg Rev. 2016;39(2):321–32 discussion 32-3.
Hu B, Yang XR, Xu Y, Sun YF, Sun C, Guo W, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. 2014;20(23):6212–22.
Samii A, Gerganov VM, Herold C, Hayashi N, Naka T, Mirzayan MJ, et al. Chordomas of the skull base: surgical management and outcome. J Neurosurg. 2007;107(2):319–24.
Li M, Zhai Y, Bai J, Wang S, Gao H, Li C, et al. SNF5 as a prognostic factor in skull base chordoma. J Neuro-Oncol. 2018;137(1):139–46.
Di Maio S, Temkin N, Ramanathan D, Sekhar LN. Current comprehensive management of cranial base chordomas: 10-year meta-analysis of observational studies. J Neurosurg. 2011;115(6):1094–105.
Pang Q, Zhang J-Y, Xu X-S, Song S-D, Qu K, Chen W, et al. Significance of platelet count and platelet-based models for hepatocellular carcinoma recurrence. World J Gastroenterol. 2015;21(18):5607.
Nouso K, Ito Y, Kuwaki K, Kobayashi Y, Nakamura S, Ohashi Y, et al. Prognostic factors and treatment effects for hepatocellular carcinoma in child C cirrhosis. Br J Cancer. 2008;98(7):1161–5.
Amano H, Tashiro H, Oshita A, Kobayashi T, Tanimoto Y, Kuroda S, et al. Significance of platelet count in the outcomes of hepatectomized patients with hepatocellular carcinoma exceeding the Milan criteria. J Gastrointest Surg. 2011;15(7):1173–81.
Wu W-C, Chiou Y-Y, Hung H-H, Kao W-Y, Chou Y-H, Su C-W, et al. Prognostic significance of computed tomography scan-derived splenic volume in hepatocellular carcinoma treated with radiofrequency ablation. J Clin Gastroenterol. 2012;46(9):789–95.
Marusyk A, Polyak K. Tumor heterogeneity: causes and consequences. Biochimica et Biophysica Acta (BBA)-reviews on. Cancer. 2010;1805(1):105–17.
Kumagai S, Tokuno J, Ueda Y, Marumo S, Shoji T, Nishimura T, et al. Prognostic significance of preoperative mean platelet volume in resected non-small-cell lung cancer. Mol Clin Oncol. 2015;3(1):197–201.
Takeuchi H, Abe M, Takumi Y, Hashimoto T, Kobayashi R, Osoegawa A, et al. The prognostic impact of the platelet distribution width-to-platelet count ratio in patients with breast cancer. PloS one. 2017;12(12):e0189166.
Bick RL. Cancer-associated thrombosis. N Engl J Med. 2003;349(2):109–11.
Refaai MA, Phipps RP, Spinelli SL, Blumberg N. Platelet transfusions: impact on hemostasis, thrombosis, inflammation and clinical outcomes. Thromb Res. 2011;127(4):287–91.
Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140(6):883–99.
Heldin C-H, Westermark B. Mechanism of action and in vivo role of platelet-derived growth factor. Physiol Rev. 1999;79(4):1283–316.
Tamborini E, Miselli F, Negri T, Lagonigro MS, Staurengo S, Dagrada GP, et al. Molecular and biochemical analyses of platelet-derived growth factor receptor (PDGFR) B, PDGFRA, and KIT receptors in chordomas. Clin Cancer Res. 2006;12(23):6920–8.
Zhai Y, Bai J, Wang S, Gao H, Li M, Li C, et al. Analysis of clinical factors and PDGFR-beta in predicting prognosis of patients with clival chordoma. J Neurosurg. 2018;129(6):1429-37.
Lebellec L, Bertucci F, Tresch-Bruneel E, Bompas E, Toiron Y, Camoin L, et al. Circulating vascular endothelial growth factor (VEGF) as predictive factor of progression-free survival in patients with advanced chordoma receiving sorafenib: an analysis from a phase II trial of the french sarcoma group (GSF/GETO). Oncotarget. 2016;7(45):73984–94.
Schoene NW. Design criteria: tests used to assess platelet function. Am J Clin Nutr. 1997;65(5 Suppl):1665s–8s.
Bessman JD, Williams LJ, Gilmer PR Jr. Platelet size in health and hematologic disease. Am J Clin Pathol. 1982;78(2):150–3.
Kaushansky K. Growth factors and hematopoietic cell fate. A new feature: controversies in hematology. Blood. 1998;92(2):345.
Guo Y, Xu F, Lu T, Duan Z, Zhang Z. Interleukin-6 signaling pathway in targeted therapy for cancer. Cancer Treat Rev. 2012;38(7):904–10.
Kushlinskii NE, Timofeev YS, Solov'ev YN, Gerstein ES, Lyubimova NV, Bulycheva IV. Components of the RANK/RANKL/OPG system, IL-6, IL-8, IL-16, MMP-2, and calcitonin in the sera of patients with bone tumors. Bull Exp Biol Med. 2014;157(4):520–3.
Gulluoglu S, Tuysuz EC, Sahin M, Yaltirik CK, Kuskucu A, Ozkan F, et al. The role of TNF-α in chordoma progression and inflammatory pathways. Cell Oncol (Dordrecht). 2019;42(5):663–77.
Yang H, Lang S, Zhai Z, Li L, Kahr WH, Chen P, et al. Fibrinogen is required for maintenance of platelet intracellular and cell-surface P-selectin expression. Blood. 2009;114(2):425–36.
Matsunaga T, Saito H, Fukumoto Y, Shimizu S, Kono Y, Murakami Y, et al. The postoperative platelet distribution width is useful for predicting the prognosis in patients with esophageal squamous cell carcinoma. Surg Today. 2020;50(2):123–33.
Acknowledgements
We are grateful for the supporting of all patients.
Funding
This study was supported by the National Natural Science Foundation of China (81771489); Supported by Beijing Municipal Science & Technology Commission (Z171100000117002). The funding bodies had no role in the design of the study, collection, analysis, interpretation of data, and writing of the manuscript.
Author information
Authors and Affiliations
Contributions
MXL, JWB and YZZ contributed to the conception and design of the study. SW, YXZ, SHZ, CZL and JD contributed to data collection, analysis and interpretation of data. MXL wrote the manuscript. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The current study was approved by the Ethics Committee of Beijing Tiantan Hospital and carried out in keeping with the 1964 Declaration of Helsinki. In addition, informed consent was obtained from all participants, and we further analyzed the data anonymously.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
X-tile software was used to identify the optimal cut-off values of PLT, MPV and PDW for OS analysis in skull base chordoma. (a) The optimal cut-off value of PLT was 266. (b) The optimal cut-off value of MPV was 11.9. (c) The optimal cut-off value of PDW was 14.5. PLT, platelet count; MPV, mean platelet volume; PDW, platelet distribution width; OS, overall survival.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, M., Bai, J., Wang, S. et al. Mean platelet volume and platelet distribution width serve as prognostic biomarkers in skull base chordoma: a retrospective study. BMC Cancer 20, 988 (2020). https://doi.org/10.1186/s12885-020-07497-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-020-07497-7