Abstract
Background
The risk of positive lymph nodes in patients with muscle-invasive bladder urothelial carcinoma (MIBC) can be used to guide treatment recommendations. However, little is known about the effect of age on lymph node positivity (LN+). This study aimed to evaluate the effect of age on LN+ in MIBC.
Methods
We analyzed patients with stage T2–T4 bladder urothelial carcinoma who had not received preoperative radiotherapy, had at least one lymph node examined, and underwent cystectomy between 1998 and 2015. The Cochran–Armitage trend test and logistic univariate and multivariate analyses were used to evaluate the effect of age on LN+ in all T stages.
Results
In total, 15,624 patients with MIBC were identified, including 747 patients aged ≤50 years (4.78%), 2614 patients aged 50–59 years (16.73%), 4914 patients aged 60–69 years (31.45%), 5225 patients aged 70–79 years old (33.44%), and 2124 patients aged > 80 years (13.59%). In T2–T4 staging, LN+ was negatively correlated with age. After adjustment for several covariates, multivariate logistic regression analysis revealed that age was an independent risk factor for LN+.
Conclusions
In this large SEER analysis, Young patients with MIBC have a higher risk of lymph node metastasis. This finding is worthy of further study and may eventually affect the treatment decisions of young patients.
Similar content being viewed by others
Background
Bladder cancer is the most common malignant tumor of the urinary system, with high morbidity and mortality. It is estimated that there will be approximately 81,400 new bladder cancer patients and 17,980 deaths due to this disease in the USA in 2020 [1]. Urothelial carcinoma accounts for approximately 90% of bladder cancers, 25% of which can develop into muscle-invasive bladder cancer [2] and approximately half of which are potentially fatal [3]. Radical cystectomy plus pelvic lymph node dissection (PLND) is considered the gold standard treatment for bladder urothelial carcinoma with invasion of the detrusor muscle [4], and up to 25% of patients turn out to have lymph node metastasis during radical cystectomy [5]. Lymph node positivity (LN+) has been shown to be an independent predictor of disease recurrence and cancer-specific death in urothelial carcinoma of the bladder [6].
In patients with muscle-invasive bladder urothelial carcinoma (MIBC), the evaluation of LN+ is very important for staging and decisions on treatment. Age is an independent predictor of LN+ in various cancers [7,8,9]. In an analysis of 46,077 patients with thyroid cancer, it was found that young patients were more likely to have LN+, regardless of the T stage [7]. Similarly, in patients with colon cancer, the risk of LN+ is associated with age at the time of diagnosis [8], and age is related with LN+ in non-small cell lung cancer [9].
However, the correlation between LN+ and age at the time of diagnosis in patients with MIBC is still uncertain. Therefore, in this study, we used data from the Surveillance, Epidemiology, and End Results (SEER) database and descriptive statistics to investigate the predictive effect of age on LN+ in patients with MIBC based on a large population dataset.
Methods
Patients
The SEER database records data on the morbidity, mortality, and illness of millions of patients with malignant tumors in certain states and counties of the USA. In this study, we analyzed the records of all patients diagnosed with MIBC between 1988 and 2015 in the SEER database. The inclusion criteria were as follows: 1. patients clinically and pathologically diagnosed as MIBC; 2. patients who underwent surgery and for whom exact pathological details were available; 3. patients who had at least one lymph node examined. The exclusion criteria were as follows: 1. MIBC patients aged < 18 years; 2. patients with distant metastasis; 3. patients who received radiotherapy and neoadjuvant chemotherapy and chemotherapy (to eliminate the effect of preoperative radiotherapy on lymph node collection and LN+); 4. patients who underwent local resection or local destruction surgery (as this type of surgery is associated with low expectation of obtaining lymph nodes).
Data analysis
The primary outcome was LN+. Age was considered a categorical variable, and patients were classified by 10-year age groups. Considering the relatively small number of patients under the age of 50 years, we classified them all into one group. Chi-square analysis was used to compare the proportions of all classified data. The number of lymph nodes examined (LNE) was compared between the age groups by rank sum test. We used Cochran–Armitage trend tests to evaluate changes in LN+ with age. Using LN+ as the result, logistic regression univariate and multivariate analyses were performed for T2–T4 stages. Age, sex, race, tumor grade, year of operation and the number of lymph node examinations were covariates. Age ≥ 80 years was used as the reference group. Odds ratios (ORs) and 95% confidence intervals (CIs) are reported. SPSS v.25 and R v.3.6.1 were used for analyses. All statistical tests were two-sided, and P < 0.05 was considered significant.
Results
Demographic and clinicopathological characteristics
We identified 15,624 patients who met our research eligibility criteria. Table 1 summarizes the demographic and tumor characteristics. Most of the patients were aged 70–79 years (33.44%, n = 5225). Only 747 patients (4.78%) were aged < 50 years; 2614 (16.73%), 50–59 years; 4914 (31.45%), 60–69 years; and 2124 (13.59%), > 80 years. Grade IV (58.76%) and stage T3 (41.477%) accounted for the largest proportion in tumor grading and staging, respectively. Caucasian and afroamericans accounted for 89.15 and 5.88%, respectively. The median number of patients with stage T2 receiving LN examination was the highest (n = 13), and the average number of patients with stage T3 and T4 receiving LN examination was 11 and 12, respectively (Table 2).
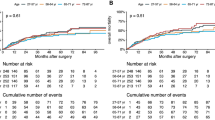
Impact of age at diagnosis on LN+
To explore the effect of age on LN+, we grouped patients according to T stage. In total, 4321 patients (27.66%) had lymph node metastasis. The rate of LN+ was 12.37% in T2, 34.68% in T3, and 46.13% in T4. In all stages, age was significantly negatively correlated with LN+ (P < 0.05; Table 3).
Multivariable analysis of LN+
We used multivariate logistic regression to evaluate whether the association between age and LN+ at the time of diagnosis was independent of other known risk factors. Sex, race, year of operation, tumor grade, and LNE were used as covariates of the adjusted model. Age remained a significant predictor of LN+ in all T stages (Table 4, P < 0.05), and young MIBC patients were more likely to have LN+. Compared with the reference group (aged > 80 years), patients with T2 and T4 stages, aged < 50 years, were more likely to have LN+, and the adjusted OR was 1.805 (95% CI, 1.217–2.676) and 1.492 (95% CI, 1.002–2.220), respectively. The probability of LN+ was the highest in the 50–59-year age group with T3, and the adjusted OR was 1.407 (95% CI, 1.173–1.688).
Discussion
Tumor stage and grade are associated with the risk of lymph node metastasis in MIBC [10, 11]. However, it is not ideal to use staging and grading alone to predict lymph node metastasis. The addition of other important prediction factors, such as age, may improve the risk stratification of patients, and more active, multi-modal treatment may be selected for high-risk patients, thus improving the prognosis. No study has explored the predictive effect of age on LN+ in patients with MIBC. In the current study, we analyzed data from 15,624 MIBC patients extracted from the SEER database. We found that young patients had a higher tendency for LN+ at any T stage. This finding was validated in multivariate analysis including sex, race, grade, LNE, and year of operation. This is consistent with the results reported by Hellenthal et al. that per 10-year age increase, the odds of LN+ in patients with bladder cancer decreased by approximately 20% [12].
The effect of age on LN+ may be related to biological differences between young and old patients. Migaldi et al. pointed out that low p27Kip1 expression was not related to the risk of recurrence in young patients, whereas decreased p27Kip1 expression was related to an increased risk of recurrence in older patients [13]. More significantly, high Ki67 expression and low cyclinD1 expression were associated with an increased risk of recurrence in young patients, but not in older patients. Thus, compared with older patients, urothelial carcinoma of the bladder in young patients may involve different molecular pathways. In addition, with increasing age, various changes occur in the body, including those in the lymph nodes [14]. Aging leads to a decrease in the cortex and medulla of the lymph nodes and an increase in degeneration into inactive lymph nodes without lymph node tissue, resulting in reduced lymph flow to and retraction of the lymph nodes [15, 16]. This may be one of the important reasons for the effect of age on LN+.
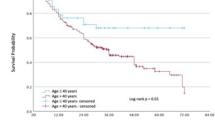
Lymph node dissection is an indispensable part of radical resection of bladder cancer. The reasonable PLND has been proved to be helpful in determing the pathological stage, guide follow-up treatment [5]. However, it is still controversial whether PLND can improve the prognosis of patients. In a retrospective study, young patients with radical cystectomy and PLND had better all cause and cancer specific survival than radical cystectomy alone [17]. Another retrospective study have suggested that the survival prognosis of extended lymphadenectomy group is better than that of standard lymphadenectomy group [18]. But it’s worth noting that, there is a great risk of Will Rogers Phenomena and Stage migration, so the whole concept is blurred on a scientific level when examining retrospective materials [19]. Choi et al. found that compared with standard lymphadenectomy, super-extended or extended lymphadenectomy may have no significant effect on local recurrence, distant metastasis, disease-specific survival and overall survival [20]. To date, the only randomized phase 3 trial showed no improvement in PLND in either recurrence-free survival, cancer-specific survival or overall survival [21]. Therefore, more randomized prospective trials are needed to establish whether PLND can benefit patients with radical resection of bladder cancer. Moreover, extended lymphadenectomy can increase the time of operation and cause potential bleeding, lymphatic leakage, lymphoceles, autonomic nerve and ureteral injury, and serious nutritional and immune problems after operation, which significantly prolong the risk of postoperative rehabilitation and hospitalization [21,22,23,24,25]. This refutes the hypothesis that the benefits associated with PLND are consistent across ages and comorbidities. Considering the lack of a final conclusion on the scope and benefits of lymph node dissection, based on current research results, in elderly patients, because the probability of LN+ is low and their physique is generally weaker, lymph node involvement should be actively evaluated before operation. In line with our results, Koppie et al. found that for elderly patients with bladder cancer or with more underlying diseases, LN+ was lower with PLND, and thus, they recommended that PLND or regional lymph node dissection should not be performed [26]. Another study also pointed out that in older and seriously ill patients, radical cystectomy combined with PLND had no significant clinical benefit compared with radical cystectomy alone [17]. When choosing the specific way of lymph node dissection for the elderly, we should try our best to consider the time of operation and anesthesia, and the possible impact of cardiopulmonary complications on the elderly.
Clinical treatment strategies for patients with MIBC vary according to the status of lymph nodes. Accurate prediction of lymph node metastasis is essential to help doctors make reasonable decisions, especially for patients who need to be evaluated for lymph node status before surgery or do not need PLND. Trimodality therapy (TMT) is an alternative for patients who do not undergo or refuse radical resection of bladder cancer [27]. While preserving bladder function, TMT improves the long-term survival rate and the quality of life similar to radical resection of bladder cancer [28,29,30]. However, TMT is not recommended when patients show high-risk features, such as LN+ [27, 31]. Therefore, for patients who opt for TMT, it is important to carefully evaluate lymph node involvement before operation. Because the survival time of young patients with bladder cancer is longer [32], and according to our results, young patients are more prone to LN+, a comprehensive and professional evaluation of the lymph node area should be done before deciding on TMT, so as to avoid missed diagnosis of lymph node involvement and wrong treatment.
Several limitations of our study should be noted. First, this study is limited by its long term and retrospective nature. The way patients receive surgery is affected by the year of diagnosis and clinical factors. These factors were taken into account in the multivariate analysis. However, the clinical treatment of young patients may be more aggressive than that of older patients, which leads to systematic bias. Second, the SEER database collects data from a large number of patients from the population-based cancer registry, but some data may be miscoded or omitted during the registration process. However, this error coding is random and does not introduce any system bias. Finally, the data are representative only for the population in the SEER area and do not apply to other geographic locations.
Conclusions
Our analysis of data in the SEER database showed that after considering other predictive factors, there is an increased risk of LN+ in young MIBC patients. Considering the different lymph node invasiveness in patients of different ages, our results can guide clinicians to choose the best treatment. Our findings are worthy of further study and may influence the assessment of lymph node invasiveness in patients with MIBC.
Availability of data and materials
In this retrospective study, our data were downloaded from the SEER database.
Abbreviations
- LN+:
-
Lymph node positivity
- LNE:
-
Lymph nodes examined
- MIBC:
-
Muscle-invasive bladder urothelial carcinoma
- NAC:
-
Neoadjuvant chemotherapy
- PLND:
-
Pelvic lymph node dissection
- SE:
-
Standard error
- SEER:
-
Surveillance Epidemiology and End Results
- TMT:
-
Trimodality therapy
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7–30.
Kamat AM, Hahn NM, Efstathiou JA, Lerner SP, Malmstrom PU, Choi W, et al. Bladder cancer. Lancet. 2016;388:2796–810.
Babjuk M, Bohle A, Burger M, Capoun O, Cohen D, Comperat EM, et al. EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder: update 2016. Eur Urol. 2017;71:447–61.
Bruins HM, Arends TJ, Pelkman M, Hulsbergen-van de Kaa CA, van der Heijden AG, Witjes JA. Radical cystectomy in a Dutch University hospital: long-term outcomes and prognostic factors in a homogeneous surgery-only series. Clin Genitourin Cancer. 2014;12:190–5.
Bruins HM, Veskimae E, Hernandez V, Imamura M, Neuberger MM, Dahm P, et al. The impact of the extent of lymphadenectomy on oncologic outcomes in patients undergoing radical cystectomy for bladder cancer: a systematic review. Eur Urol. 2014;66:1065–77.
Spradling K, Lotan Y, Shokeir A, Abol-Enein H, Mosbah A, Morgan JB, et al. Lymphovascular invasion is associated with oncologic outcomes following radical cystectomy for squamous cell carcinoma of the urinary bladder. Urol Oncol. 2016;34(417):e1–8.
Wang J, Liu J, Pan H, Jiang C, Liu S, Zhu Z, et al. Young age increases the risk of lymph node positivity in papillary thyroid cancer patients: a SEER data-based study. Cancer Manag Res. 2018;10:3867–73.
Wang H, Lu H, Yang H, Zhang X, Thompson EW, Roberts MS, et al. Impact of age on risk of lymph node positivity in patients with colon cancer. J Cancer. 2019;10:2102–8.
Xia W, Wang A, Jin M, Mao Q, Xia W, Dong G, et al. Young age increases risk for lymph node positivity but decreases risk for non-small cell lung cancer death. Cancer Manag Res. 2018;10:41–8.
Kim HS, Moon KC, Jeong CW, Kwak C, Kim HH, Ku JH. Histological variant as the significant predictor of survival in patients with lymph node positive urothelial carcinoma of the bladder. Sci Rep. 2015;5:9626.
Abdel-Latif M, Abol-Enein H, El-Baz M, Ghoneim MA. Nodal involvement in bladder cancer cases treated with radical cystectomy: incidence and prognosis. J Urol. 2004;172:85–9.
Hellenthal NJ, Ramirez ML, Evans CP. deVere white RW, Koppie TM. Trends in pelvic lymphadenectomy at the time of radical cystectomy: 1988 to 2004. J Urol. 2009;181:2490–5.
Migaldi M, Rossi G, Maiorana A, Sartori G, Ferrari P, De Gaetani C, et al. Superficial papillary urothelial carcinomas in young and elderly patients: a comparative study. BJU Int. 2004;94:311–6.
Thompson HL, Smithey MJ, Surh CD, Nikolich-Zugich J. Functional and homeostatic impact of age-related changes in lymph node stroma. Front Immunol. 2017;8:706.
Pan WR, Suami H, Taylor GI. Senile changes in human lymph nodes. Lymphat Res Biol. 2008;6:77–83.
Hadamitzky C, Spohr H, Debertin AS, Guddat S, Tsokos M, Pabst R. Age-dependent histoarchitectural changes in human lymph nodes: an underestimated process with clinical relevance? J Anat. 2010;216:556–62.
Larcher A, Sun M, Schiffmann J, Tian Z, Shariat SF, McCormack M, et al. Differential effect on survival of pelvic lymph node dissection at radical cystectomy for muscle invasive bladder cancer. Eur J Surg Oncol. 2015;41:353–60.
Abol-Enein H, Tilki D, Mosbah A, El-Baz M, Shokeir A, Nabeeh A, et al. Does the extent of lymphadenectomy in radical cystectomy for bladder cancer influence disease-free survival? A prospective single-center study. Eur Urol. 2011;60(3):572–7.
Suttmann H, Kamradt J, Lehmann J, Stockle M. Improving the prognosis of patients after radical cystectomy. Part I: the role of lymph node dissection. BJU Int. 2007;100(6):1221–4.
Choi SY, You D, Hong B, Hong JH, Ahn H, Kim CS. Impact of lymph node dissection in radical cystectomy for bladder cancer: how many vs how far? Surg Oncol. 2019;30:109–16.
Gschwend JE, Heck MM, Lehmann J, Rubben H, Albers P, Wolff JM, et al. Extended versus limited lymph node dissection in bladder Cancer patients undergoing radical cystectomy: survival results from a prospective, Randomized Trial. Eur Urol. 2019;75(4):604–11.
Han LP, Zhang HM, Abha HD, Liu T, Zhang XP. Management and prevention of chylous leakage after laparoscopic lymphadenectomy. Eur Rev Med Pharmacol Sci. 2014;18(17):2518–22.
Leibovitch I, Mor Y, Golomb J, Ramon J. The diagnosis and management of postoperative chylous ascites. J Urol. 2002;167(2 Pt 1):449–57.
Loeb S, Partin AW, Schaeffer EM. Complications of pelvic lymphadenectomy: do the risks outweigh the benefits? Rev Urol. 2010;12(1):20–4.
Stamatakis L, Godoy G, Lerner SP. Innovations in radical cystectomy and pelvic lymph node dissection. Semin Oncol. 2012;39(5):573–82.
Koppie TM, Serio AM, Vickers AJ, Vora K, Dalbagni G, Donat SM, et al. Age-adjusted Charlson comorbidity score is associated with treatment decisions and clinical outcomes for patients undergoing radical cystectomy for bladder cancer. Cancer. 2008;112(11):2384–92.
Spiess PE, Agarwal N, Bangs R, Boorjian SA, Buyyounouski MK, Clark PE, et al. Bladder Cancer, version 5.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2017;15(10):1240–67.
Giacalone NJ, Shipley WU, Clayman RH, Niemierko A, Drumm M, Heney NM, et al. Long-term outcomes after bladder-preserving tri-modality therapy for patients with muscle-invasive bladder Cancer: an updated analysis of the Massachusetts General Hospital experience. Eur Urol. 2017;71(6):952–60.
Mak KS, Smith AB, Eidelman A, Clayman R, Niemierko A, Cheng JS, et al. Quality of life in long-term survivors of muscle-invasive bladder Cancer. Int J Radiat Oncol Biol Phys. 2016;96(5):1028–36.
Alfred Witjes J, Lebret T, Comperat EM, Cowan NC, De Santis M, Bruins HM, et al. Updated 2016 EAU guidelines on muscle-invasive and metastatic bladder Cancer. Eur Urol. 2017;71(3):462–75.
Cahn DB, Ristau BT, Ghiraldi EM, Churilla TM, Geynisman DM, Horwitz EM, et al. Bladder preservation therapy: a review of the literature and future directions. Urology. 2016;96:54–61.
Liberman D, Lughezzani G, Sun M, Alasker A, Thuret R, Abdollah F, et al. Perioperative mortality is significantly greater in septuagenarian and octogenarian patients treated with radical cystectomy for urothelial carcinoma of the bladder. Urology. 2011;77(3):660–6.
Acknowledgments
We would like to thank Editage (www.editage.cn) for English language editing.
Funding
This study was financially supported by the Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (grant number: 2018-I2M-1-002) and the Beijing Hospital Clinical Research 121 Project (BJ-2018-090). The funders had no roles in study design, data collection, data analysis and interpretation, or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
Study concept and design: ZJ. T and JY. W; data acquisition or data analysis/interpretation: LF. M and M. L; manuscript drafting or manuscript revision for important intellectual content: ZJ. T, LF. M, and M. W; approval of final version of submitted manuscript: all authors; literature study: X. W, TX. D, and ML. H.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable (In this retrospective study, we provided a signed SEER research data agreement form to the SEER project, and we were granted access to and analysis of SEER data. There is no need to analyze SEER data to obtain informed consent.)
Consent for publication
Not applicable.
Competing interests
The authors have declared that no competing interest exists.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tian, Z., Meng, L., Wang, X. et al. Young age increases the risk of lymph-node metastasis in patients with muscle-invasive bladder urothelial carcinoma. BMC Cancer 20, 851 (2020). https://doi.org/10.1186/s12885-020-07354-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-020-07354-7