Abstract
Background
Chemoradiotherapy (CRT) with high cumulative doses (CDs) of cisplatin has been considered the standard of care for non-metastatic nasopharyngeal carcinoma (NPC). However, given most patients’ inability to tolerate high CDs due to cisplatin-related toxicities, the optimal CD of cisplatin during CRT remains undetermined.
Methods
Patients with non-metastatic NPC who received CRT with cisplatin between 2007 and 2017 were identified through the Thai head and neck cancer multicenter database and then categorized according to cisplatin CD (mg/m2) received. All complications and cisplatin-related toxicities during CRT were recorded.
Results
We identified 779 non-metastatic NPC patients receiving low (≤150; n = 97), intermediate (151–250; n = 411), and high (> 250; n = 271) CDs of cisplatin. Low CD patients had significantly lower mean actual radiation dose (p < 0.001) and more radiotherapy delay (p = 0.010), while intermediate CD patients had the least hospitalization (p < 0.001). Overall, 39.3% of the patients experienced cisplatin-related toxicity, which was associated with poor overall survival (OS) (p = 0.001). Acute kidney injury was observed in 7% in all patients, which was highest among low CD patients (15.5%; p = 0.002). Intermediate CD patients had significantly longer median OS than the low and high groups (64 vs. 49.8 vs. 53.2, respectively; p = 0.015). Univariate, but not multivariate, analysis showed that CD of cisplatin was significantly associated with OS.
Conclusion
CD of cisplatin during CRT was not an independent prognostic factor for OS. An intermediate CD induced minimal toxicity without compromising survival and should be considered the optimal CD. Nonetheless, a randomized phase 3 study evaluating the optimal CD of cisplatin is warranted.
Similar content being viewed by others
Background
Nasopharyngeal carcinoma (NPC) is highly endemic to Southern China, Maghreb region of North Africa, parts of the Middle East, and Southeast Asia, including Thailand [1, 2]. Epstein–Barr virus (EBV) plays a major role in carcinogenesis. Ninety-six percent of Thai patients with NPC are associated with EBV [3]. Concurrent chemoradiotherapy (CRT) with cisplatin is the standard of care for local advanced NPC treatment [4]. Several phase III clinical studies utilized high-dose cisplatin, either 100 mg/m2 every 3 weeks for three cycles [cumulative dose (CD), 300 mg/m2] or 40 mg/m2 weekly for seven cycles (CD, 280 mg/m2), for using concurrently with radiotherapy (RT) [5,6,7,8]. However, no study has evaluated the optimal cisplatin CD administration during CRT. A post-hoc analysis from a Chinese prospective phase III study of patients with non-metastatic NPC concurrently receiving weekly cisplatin and radiotherapy (RT) reported a median cisplatin CD of 240 mg/m2, despite protocols requiring a CD of 280 mg/m2 [9]. Several retrospective studies demonstrated real-world data that majority of patients received less than the standard recommendations for cisplatin CD (280–300 mg/m2) [8, 10,11,12]. However, patients receiving a lower cisplatin CD had comparable survival with patients receiving the recommended CD. Thus, the lowest efficacious cisplatin CD during CRT remains unidentified.
About 13.6% patients with cancer treated with cisplatin develop nephrotoxicity, i.e., acute kidney injury (AKI), which is significantly associated with administrated cisplatin dose [13]. Incidences of nephrotoxicity among head and neck cancer patients receiving cisplatin CRT were 30–34%, higher than in those with other cancer types [14, 15]. Therefore, we evaluated the optimal cisplatin CD for definitive CRT that would maintain efficacy and minimize toxicity among patients with non-metastatic NPC in a multicenter setting in Thailand.
Methods
Patient population
We identified patients with histologically confirmed non-metastatic NPC who received treatment at the three largest cancer centers in Thailand, Ramathibodi and Siriraj Hospitals, Mahidol University, and Songklanagarind Hospital, Prince of Songkla University, between 2007 and 2017. All medical records were retrospectively reviewed. Patient characteristics, treatments, toxicities, complications, and survival rates were abstracted and recorded in the common electronic case record form of the large multicenter multidisciplinary database for Thai head and neck cancer patients using the REDCap platform. This database was established in 2016 and was funded by the Thailand Grand Challenge Program for Research University Network (RUN) under the Precision Medicine for Cancer project. The present study was approved by the Institutional Ethic Committee.
Patients with non-metastatic NPC who received cisplatin for concurrent CRT were identified from the database. Those who received induction chemotherapy, had distant metastasis at diagnosis, or received non-cisplatin chemotherapy for CRT were excluded. For patients who cisplatin was initially started and subsequently terminated during CRT from any reasons, substitution of concurrent carboplatin CRT was allowed at their physician’s discretion. These patients were included in this analysis. All patients in this study must be treated with definitive CRT with the planned total dose of radiation of 7000 cGy. Radiation technique including 2D, 3D, and IMRT was selected for each patent based on their treating physicians according to standard of care, availability, and physician’s discretion at the time of treatment. Adjuvant platinum doublet chemotherapy was given after completion of CRT following local standard practice at treating physician’s discretion. Overall survival (OS), recurrence-free survival (RFS), distant recurrence-free survival (DRFS), and locoregional recurrence-free survival (LRFS) were determined. Death status was validated and confirmed through the Thai Social Security Death Index database.
Cisplatin dose for chemoradiotherapy and its complications
CD of cisplatin (mg/m2) used during CRT was calculated and classified into low, intermediate, and high. The dose cutoffs were identified using the area under the curve (AUC) associated with the gold standard for predicting death status. The upper cutoff of 250 mg/m2 was selected according to the AUC with significance. The CD of 150 mg/m2 was selected for the lower cutoff since the low CD of cisplatin during CRT was previously reported ranging between 100 and 160 mg/m2 in the literature [10, 16, 17]. Thus, CD of cisplatin during CRT in this study was categorized into low (≤150 mg/m2; n = 97), intermediate (151–250 mg/m2; n = 411), and high (> 250 mg/m2; n = 271; Supplement 1). The correlation between aforementioned dose levels and patient characteristics, RT treatment, treatment tolerability, complications, and survival was then determined.
Acute complications during CRT were defined as experience of any cisplatin or RT interruption, treatment delay (> 7 days), hospitalization (> 24 h), and/or discontinuation of cisplatin or RT. Cisplatin-related complications included creatinine clearance (CCr) decline after CRT (calculated using the Cockcroft–Gault formula), AKI [18], acute kidney disease (AKD), defined by (i) GFR < 60 ml/min/1.73 m2 for < 3 months, or (ii) decrease in GFR by ≥35%, or (iii) increase in serum creatinine by > 50% for < 3 months [19], electrolyte imbalance requiring hospitalization during CRT, and ototoxicity.
Statistical analysis
All analyses were performed using the STATA/MP 14.1. Descriptive statistics, including mean ± SD or median (range), were used for continuous variables. Differences between the three categories were compared using one-way analysis of variance (normal distribution) or Kruskal–Wallis test (non-normal distribution). Significant differences in proportions were determined using the Chi-square or Fisher’s exact test, as appropriate. Receiver operating characteristic analysis was conducted to determine the cutoff CD of cisplatin (mg/m2) using the gold standard for predicting death status. Associated risk factors were initially screened using univariate and multivariate Cox regression analyses for OS with significance set at p < 0.10. Identified variables were subsequently assessed using backward stepwise regression with significance set at p ≤ 0.05. The final model included cisplatin CD during CRT and other significant factors. The goodness-of-fit assumption was assessed using the Hosmer–Lemeshow method with significance set at p > 0.05. Cumulative hazard curves were modeled using the Kaplan–Meier method and compared using the Log-rank test. A p value of < 0.05 indicated statistical significance.
Results
Patient characteristics
Overall 779 eligible patients with non-metastatic NPC were identified from the database. Baseline patient and pathological characteristics according to CD of cisplatin are summarized in Table 1. Majority of the patients in this cohort (99%) had WHO grades II and III disease. Approximately 50% patients underwent prophylactic feeding tube placement prior to CRT. Among those with a prophylactic feeding tube, 88% underwent percutaneous endoscopic gastrostomy, whereas 12% underwent nasogastric tube insertion. Patients who received low CD of cisplatin were significantly older at diagnosis (p < 0.001) and had poorer smoking status (p = 0.003), lower LN stage (p = 0.016), higher incidences of comorbidities, including cardiac disease (p = 0.009), diabetes mellitus (p = 0.014), and hypertension (p = 0.043), and higher baseline CCr (p < 0.001) than other groups.
Treatments and acute complications during chemoradiotherapy
Chemotherapy
The mean CD of low-, intermediate-, and high-dose groups were 104, 207, and 287 mg/m2, respectively (Table 2). The intermediate CD group received more 3-weekly regimens than the low and high CD groups (p = 0.031). Most patients in the high CD group (98.5%) completed the planned cisplatin cycle. Only 60 patients in the low CD group (62%) received adjuvant chemotherapy, whereas 363 (88%) and 252 (93%) patients in the intermediate and high CD groups received the same, respectively (p < 0.001). However, the high CD group had a significantly lower mean CD of adjuvant cisplatin than the other groups (p = 0.002). Patients treated with low and intermediate CD were able to complete 3 cycles of adjuvant chemotherapy significantly more than high CD group (71.2% vs 74.3% vs 56.1%; p < 0.001).
Radiotherapy
Overall, 493 patients (63%) concurrently received intensity-modulated radiation therapy (IMRT) with cisplatin as the definitive treatment, whereas 122 (16%) and 149 (19%) patients underwent 3D and 2D techniques, respectively. More patients in the intermediate CD group (72.5%) received IMRT than the low (63%) and high CD (49%) groups (p < 0.001; Table 2). Patients treated with IMRT technique had significant better smoking status, ECOG performance status, higher baseline BMI, earlier stage at diagnosis, but more comorbidities including diabetes, hyperlipidemia, and hypertension. (Supplement 2) Moreover, IMRT patients had significantly higher baseline CCr, less prophylactic feeding tube, and less CD of cisplatin during CRT. Only12 patients in the 2D group (11.4%) did not receive adjuvant chemotherapy when compared with 7 (5.7%) and 76 (15.4%) patients in the 3D and IMRT groups, respectively (p = 0.002). However, those receiving a low CD of cisplatin had a significantly low mean actual RT dose (p < 0.001). Patients in the high CD group had longer duration of RT (p = 0.013), whereas RT delay was more common in low CD patients (p = 0.010).
Acute complication and cisplatin-related toxicity
Patients receiving a low CD of cisplatin experienced higher rates of cisplatin interruption, delay, and termination of cisplatin (p < 0.001) compared with the intermediate and high CD groups (Table 2). Intermediate CD patients had the lowest incidence (4%) of hospitalization during CRT (p < 0.001). Among those, in whom cisplatin was terminated, 31 (45.5%) and 8 (9.9%) in the low and intermediate CD groups subsequently received concurrent carboplatin and radiation, respectively. The low CD group had more patients with at least one acute complication (79.4%) than the other groups.
Overall, cisplatin-related toxicity occurred in 306 patients (39.3%), with the low CD group having the highest incidence (50.5%; Table 2). The most common cisplatin-related toxicities included nephrotoxicity (26.4%), grade 3–4 vomiting (4%), grade 3–4 electrolyte imbalance (3.6%), and grade 3–4 infection (including febrile neutropenia; 3.3%; Supplement 3). Mean percent drop in CCr was significantly associated with higher CD of cisplatin (p = 0.001). Overall, 7% patients developed AKI during CRT, with the low CD group having the highest number (15.5%; p = 0.002). Furthermore, the incidence of AKD was comparable between the high (38.2%) and low (39.1%) cisplatin groups but lower in the intermediate group (28.7%; p = 0.038).
Survival
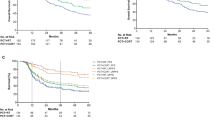
The median follow-up duration of the study was 59.4 months. Patients who received an intermediate CD of cisplatin had significantly longer median OS (64 months) than low and high (49.8 and 53.2 months, respectively) CD groups (p = 0.015; Fig. 1a). Moreover, 5-year OS among patients treated with low, intermediate, and high CD of cisplatin were 54, 72, and 60%, respectively (p = 0.004). The intermediate CD group (64%) had a significantly higher 7-year OS than the low (51%) and high (53%) CD groups (p < 0.001). Subset analysis of patients who underwent IMRT showed no significant differences in OS among the cisplatin CD groups (p = 0.584), whereas intermediate CD patients who underwent non-IMRT had significantly longer OS than the other groups (p = 0.016; Fig. 2). Those who experienced cisplatin-related toxicity during CRT had significantly shorter OS (p = 0.001; Supplement 4). In addition, the intermediate CD patients had significantly longer RFS, DRFS, and LRFS than the low- and high-dose groups (Fig. 1b–d).
Univariate and multivariate analyses of OS are summarized in Table 3. Univariate, but not multivariate, analysis showed that CD of cisplatin was significantly associated with OS. Multivariate analysis showed that age ≥ 65, stage IVab at diagnosis, 2D/3D radiation technique, actual radiation dose of < 6600 cGy, and hospitalization during CRT were associated with poor OS, whereas baseline BMI of ≥23 kg/m2 and adjuvant chemotherapy were associated with longer OS.
Discussion
Patients who received an intermediate CD of cisplatin (151–250 mg/m2; mean 207 mg/m2) achieved the highest survival and lowest overall complications and cisplatin-related toxicities. However, only univariate analysis showed that cisplatin CD during CRT associated with OS. This suggests that cisplatin CD was not an independent prognostic factor for OS in non-metastatic NPC. Therefore, the poorer survival in the low and high CD groups might have been affected by other related factors. Most of those who received a high CD of cisplatin (> 250 mg/m2; mean 287 mg/m2) were treated with the standard recommended CD of cisplatin based on several pivotal phase III studies [5,6,7]. However, the high CD patients included herein developed significant more complications and cisplatin-related toxicities during treatment than the other groups. Though incidences of AKI were comparable among these groups, the high CD group had significantly higher incidences of AKD, cisplatin-related hospitalization, all cisplatin-related toxicities, and CCr decline after completion of CRT (Table 2). In contrast, patients who received low cisplatin CD (≤150 mg/m2; mean 104 mg/m2) had poorer survival and more complications and cisplatin-related toxicities. Interestingly, none of the patients included herein satisfied the cisplatin ineligibility criteria for patients with head and neck cancer undergoing CRT in the Asia Pacific region [20]. However, some patients in this group could be considered high risk due to their age (> 70 years) and ECOG of 2. Moreover, majority of the patients in the low CD group could have been cisplatin ineligible in the real world given that half of them suffered from cisplatin-related toxicity, whereas two-third experienced interruptions during cisplatin treatment. In addition, the present study showed that patients who suffered from cisplatin-related toxicity had poor OS. Therefore, we hypothesized that low survival observed in high CD group could have been attributed to cisplatin-related complications, which interfered with other significant treatments factors, such as treatment interruption, hospitalization, RT dose, and delay. However, it remains inconclusive whether the low survival observed in the low CD group was indeed related to inadequate cisplatin CD during CRT or intolerability to cisplatin that might have affected the primary treatment, RT.
A post-hoc analysis of a Chinese prospective phase III study involving 298 locally advanced NPC patients who underwent CRT reported that a cisplatin CD of ≥240 mg/m2 was not an independent prognostic factor for OS [9]. A larger retrospective study on 549 patients with locally advanced NPC who underwent concurrent cisplatin and IMRT from the same group revealed similar results [12]. Another retrospective Chinese study including 491 patients with locally advanced NPC who received with cisplatin and IMRT [10] showed that those who received a low cisplatin CD (≤100 mg/m2) had poorer OS and DRFS than those who received intermediate (101 to ≤200 mg/m2) and high CDs (> 200 mg/m2). These results are similar to those presented herein given that our intermediate CD group received a mean cisplatin CD of 207 mg/m2. However, none of the previous studies included a high CD group that received close to the recommended cisplatin CD (280–300 mg/m2) to which we could compared [7, 9, 10, 12]. Moreover, none of these previous studies reported overall complications and cisplatin-related toxicities during CRT in each group.
Recently, induction chemotherapy with gemcitabine and cisplatin has prolonged OS and become the standard of care for treating locally advanced NPC [8]. Most patients (97%) completed three cycles of induction chemotherapy, wherein cisplatin CD was 240 mg/m2. During CRT, patients in the induction group received significantly less median dose intensity than the standard group (200 vs. 300 mg/m2; p < 0.001). A Chinese retrospective study showed no difference in OS among cisplatin CDs of more or less 160 mg/m2 during CRT for patients with locally advanced NPC receiving induction chemotherapy [16]. A larger study on 990 Chinese patients with NPC undergoing induction chemotherapy showed that a cisplatin CD of ≤100 mg/m2 was an independent prognostic factor for PFS and DRFS, but not for OS, among those who responded to induction chemotherapy [17]. Therefore, the optimal CD of cisplatin during CRT after completion of induction chemotherapy could perhaps be lower than that recommended [7, 8]. Most studies, including our study, have suggested that the lowest cisplatin CD during CRT (at least 150–200 mg/m2) might not affect survival [9, 10, 19, 20].
Interestingly, the effect of cisplatin CD on OS was not observed among patients who received IMRT but was pronounced among those who received non-IMRT. An important caveat to this study is its retrospective nature, which led to prognostically relevant baseline differences in radiation treatments received by patients. These often result from physicians’ selection bias and the availability of IMRT at the time of diagnosis. Notably, IMRT is considered a modern technique when compared to 2D or 3D radiotherapy, thus the majority of patients in this study were treated with non-IMRT techniques in the earlier years, in contrast to NPC patients from large cancer centers in Thailand, who are often treated with IMRT. Nonetheless, IMRT provides significantly better survival and lower serious toxicity compared to 2D and 3D techniques for the treatment of locally advanced NPC [21]. The effects of IMRT might override the benefit of adding it to concurrent chemotherapy for intermediate-risk (stage II and T3N0M0) NPC patients given that no improvement in OS had been observed [22, 23]. Thus, a similar phenomenon may be observed herein for the variation of cisplatin CD.
Our study contains several limitations, especially selection bias of the actual CD of cisplatin administration during CRT due to retrospective nature of the study. To our knowledge, no phase III study has evaluated the optimal cisplatin CD during CRT for locally advanced NPC. All retrospective studies, including the present study, contain limitations, particularly selection bias of treating physicians, due to their retrospective nature. Therefore, in clinical practice, patients with locally advanced NPC might be receiving CD of cisplatin as recommended by the standard guideline or pivotal phase III randomized studies [5,6,7,8]. This may lead to unnecessary complications and toxicities, especially from cisplatin [14, 15]. Moreover, these complications and toxicities may delay and/or affect radiation treatment, leading to poor survival. Thus, a randomized phase 3 study that would evaluate the optimal cisplatin CD during CRT for locally advanced NPC is warranted.
Conclusions
Though intermediate cisplatin CD (151–250 mg/m2) during CRT was not an independent prognostic factor for OS, it allowed for minimal overall complications and cisplatin-related toxicities without compromising survivals. Moreover, cisplatin-related toxicities during CRT were associated with poor OS. Thus, an intermediate dose should be considered as the optimal cisplatin CD concurrent with radiation for non-metastatic NPC. Nonetheless, a randomized phase III study that would evaluate the optimal cisplatin CD during CRT for locally advanced NPC is warranted.
Availability of data and materials
Not applicable.
Abbreviations
- AKD:
-
Acute kidney disease
- AKI:
-
Acute kidney injury
- CCr:
-
Creatinine clearance
- CD:
-
Cumulative dose
- CI:
-
Confidence intervals
- CRT:
-
Chemoradiotherapy
- CT:
-
Chemotherapy
- DRFS:
-
Distant recurrence-free survival
- EBV:
-
Epstein–Barr virus
- GFR:
-
Glomerular filtration rate
- HR:
-
Hazard ratios
- IMRT:
-
Intensity-modulated radiation therapy
- LRFS:
-
Locoregional recurrence-free survival
- NPC:
-
Nasopharyngeal carcinoma
- OS:
-
Overall survival
- RFS:
-
Recurrence-free survival
- RT:
-
Radiotherapy
- RUN:
-
Research University Network
References
Yu MC, Yuan JM. Epidemiology of nasopharyngeal carcinoma. Semin Cancer Biol. 2002;12:421–9.
Tangjaturonrasme N, Vatanasapt P, Bychkov A. Epidemiology of head and neck cancer in Thailand. Asia Pac J Clin Oncol. 2018;14:16–22.
Larbcharoensub N, Mahaprom K, Jiarpinitnun C, Trachu N, Tubthong N, Pattaranutaporn P, et al. Characterization of PD-L1 and PD-1 expression and CD8+ tumor-infiltrating lymphocyte in Epstein-Barr virus-associated nasopharyngeal carcinoma. Am J Clin Oncol. 2018;41:1204–10.
Chan AT, Gregoire V, Lefebvre JL, Licitra L, Hui EP, Leung SF, et al. Nasopharyngeal cancer: EHNS-ESMO-ESTRO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012;23:vii83–5.
Al-Sarraf M, LeBlanc M, Giri PG, Fu KK, Cooper J, Vuong T, et al. Chemoradiotherapy versus radiotherapy in patients with advanced nasopharyngeal cancer: phase III randomized intergroup study 0099. J Clin Oncol. 1998;16:1310–7.
Chen L, Hu CS, Chen XZ, Hu GQ, Cheng ZB, Sun Y, et al. Concurrent chemoradiotherapy plus adjuvant chemotherapy versus concurrent chemoradiotherapy alone in patients with locoregionally advanced nasopharyngeal carcinoma: a phase 3 multicentre randomised controlled trial. Lancet Oncol. 2012;13:163–71.
NCCN®. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Head and Neck Cancers V3.2019. In. https://www.nccn.org. Accessed 1 Nov 2019.
Zhang Y, Chen L, Hu GQ, Zhang N, Zhu XD, Yang KY, et al. Gemcitabine and cisplatin induction chemotherapy in nasopharyngeal carcinoma. N Engl J Med. 2019;381:1124–35.
Peng H, Chen L, Zhang Y, Li WF, Mao YP, Zhang F, et al. Prognostic value of the cumulative cisplatin dose during concurrent chemoradiotherapy in locoregionally advanced nasopharyngeal carcinoma: a secondary analysis of a prospective phase III clinical trial. Oncologist. 2016;21:1369–76.
Guo SS, Tang LQ, Zhang L, Chen QY, Liu LT, Guo L, et al. The impact of the cumulative dose of cisplatin during concurrent chemoradiotherapy on the clinical outcomes of patients with advanced-stage nasopharyngeal carcinoma in an era of intensity-modulated radiotherapy. BMC Cancer. 2015;15:977.
Danchaivijitr P, Ngamphaiboon N, Jiarpinitnun C, Sirachainan E, Pattaranutaporn P, Setakornnukul J. An optimal cumulative dose of cisplatin in chemoradiotherapy as a definitive treatment for non-metastatic nasopharyngeal carcinoma: a retrospective multicenter study. Ann Oncol. 2016;27:328–50.
Peng H, Chen L, Li WF, Guo R, Mao YP, Zhang Y, et al. The cumulative cisplatin dose affects the long-term survival outcomes of patients with nasopharyngeal carcinoma receiving concurrent chemoradiotherapy. Sci Rep. 2016;6:24332.
Motwani SS, McMahon GM, Humphreys BD, Partridge AH, Waikar SS, Curhan GC. Development and validation of a risk prediction model for acute kidney injury after the first course of cisplatin. J Clin Oncol. 2018;36:682–8.
Faig J, Haughton M, Taylor RC, D'Agostino RB Jr, Whelen MJ, Porosnicu Rodriguez KA, et al. Retrospective analysis of cisplatin nephrotoxicity in patients with head and neck cancer receiving outpatient treatment with concurrent high-dose cisplatin and radiotherapy. Am J Clin Oncol. 2018;41:432–40.
Patimarattananan T, Pattaranutaporn P, Unwanatham N, Jiarpinitnun C, Nongnuch A, Ngamphaiboon N. Risk and impact of renal impairment of locally advanced head and neck squamous cell carcinoma patients who received chemoradiotherapy with cisplatin. Ann Oncol. 2019;30:v449–74.
Lv JW, Qi ZY, Zhou GQ, He XJ, Chen YP, Mao YP, et al. Optimal cumulative cisplatin dose in nasopharyngeal carcinoma patients receiving additional induction chemotherapy. Cancer Sci. 2018;109:751–63.
Liu SL, Sun XS, Yan JJ, Chen QY, Lin HX, Wen YF, et al. Optimal cumulative cisplatin dose in nasopharyngeal carcinoma patients based on induction chemotherapy response. Radiother Oncol. 2019;137:83–94.
Ostermann M, Joannidis M. Acute kidney injury 2016: diagnosis and diagnostic workup. Crit Care. 2016;20:299.
Barry R, James MT. Guidelines for classification of acute kidney diseases and disorders. Nephron. 2015;131:221–6.
Ahn MJ, D'Cruz A, Vermorken JB, Chen JP, Chitapanarux I, Dang HQ, et al. Clinical recommendations for defining platinum unsuitable head and neck cancer patient populations on chemoradiotherapy: a literature review. Oral Oncol. 2016;53:10–6.
Lee AW, Ng WT, Chan LL, Hung WM, Chan CC, Sze HC, et al. Evolution of treatment for nasopharyngeal cancer--success and setback in the intensity-modulated radiotherapy era. Radiother Oncol. 2014;110:377–84.
Zhang F, Zhang Y, Li WF, Liu X, Guo R, Sun Y, et al. Efficacy of concurrent chemotherapy for intermediate risk NPC in the intensity-modulated radiotherapy era: a propensity-matched analysis. Sci Rep. 2015;5:17378.
Liu F, Jin T, Liu L, Xiang Z, Yan R, Yang H. The role of concurrent chemotherapy for stage II nasopharyngeal carcinoma in the intensity-modulated radiotherapy era: a systematic review and meta-analysis. PLoS One. 2018;13:e0194733.
Acknowledgements
The study was funded by the Thailand Grand Challenge Program for Research University Network (RUN) under the Precision Medicine for Cancer project by the National Research Council of Thailand (NRCT). The authors thank Chanaphat Pundorlha, and Sirichai Srigate for assisting with data collection and verification, and Ms. Dollapas Punpanich for statistical analysis.
Funding
The study was funded by the Thailand Grand Challenge Program for Research University Network (RUN) under the Precision Medicine for Cancer project by the National Research Council of Thailand (NRCT) to Nuttapong Ngamphaiboon. The funding source has no involvement in the design of the study; data collection, analysis, and interpretation of data; and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
All authors have read and approved the manuscript. Study concepts: NN, PD. Study design: NN, PD. Data acquisition: AD, JS, TD, RJ, CJ. Quality control of data and algorithms: BS, PP. Data analysis and interpretation: PD, BS, PP, NN. Statistical analysis: NN, BS. Manuscript preparation: NN. Manuscript editing: BS, CJ, PP, AD, PD. Manuscript review: All authors.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The ethics approval was granted by the ethics committee of Mahidol and Prince of Songkla Universities. Ethics approval was obtained through the ethics committee at the Ramathibodi (ID 07–59-48), and Siriraj (ECI 149/2562) hospitals, Mahidol university, and Songklanagarind hospital (REC.61–007–14-1), Prince of Songkla University, and all patient information was de-identified.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Supplement 1.
Cumulative dose of cisplatin (mg/m2) cutoff using the gold standard for death status. Supplement 2. Baseline characteristics of patients treated with different radiation technique. Supplement 3. Cisplatin-related toxicity during chemoradiotherapy in all patients. Supplement 4. Overall survival of patients who experienced cisplatin-related toxicities during chemoradiotherapy.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ngamphaiboon, N., Dechaphunkul, A., Setakornnukul, J. et al. Optimal cumulative dose of cisplatin for concurrent chemoradiotherapy among patients with non-metastatic nasopharyngeal carcinoma: a multicenter analysis in Thailand. BMC Cancer 20, 518 (2020). https://doi.org/10.1186/s12885-020-07024-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-020-07024-8