Abstract
Background
Bone metastasis (BM) is one of the common sites of hepatocellular carcinoma (HCC), and the prognosis of BM patients is worse than patients without it. Our study aimed to identify predictors and prognostic factors of BM in HCC patients and develop two nomograms to quantify the risk of BM and the prognosis of HCC patients with BM.
Methods
We retrospectively reviewed the data of patients who were diagnosed as HCC between 2010 and 2015 in the Surveillance, Epidemiology, and End Results (SEER) database. Independent predictors for BM from HCC patients were determined by the univariate and multivariate logistic regression analysis. Independent prognostic factors for HCC patients with BM were identified by univariate and multivariate Cox regression analysis. Two nomograms were established and evaluated by calibration curves, receiver operating characteristic (ROC) curve, and decision curve analysis (DCA).
Results
Nine thousand and forty-seven patients were included. The independent risk factors of BM in newly diagnosed HCC patients are sex, grade, T stage, and N stage. The independent prognostic factors for HCC patients with BM are radiotherapy, chemotherapy, and lung metastasis. The AUC of diagnostic nomogram were 0.726 in the training set and 0.629 in the testing set. For the prognostic nomogram, the AUCs of 6-, 9-, and 12-months were 0.753, 0.799, and 0.732 in the training set and 0.698, 0.770, and 0.823 in the validation set. The calibration curve and DCA indicated the good performance of the nomogram.
Conclusions
Two nomograms were established to predict the incidence of BM in HCC patients and the prognosis of HCC patients with BM, respectively. Both nomograms have satisfactory accuracy, and clinical utility may benefit for clinical decision-making.
Similar content being viewed by others
Background
Hepatocellular carcinoma (HCC) is one of the most common primary malignant tumors and the fourth leading cause of cancer-related death worldwide, with 841,000 new cases and at least 780,000 deaths in 2018 [1]. Nowadays, surgical excision, liver transplantation, local administration of radiation or chemical drugs, and combined therapy are the main treatments for HCC patients [2]. However, most patients are diagnosed in the advanced stage. Therefore, the prognosis remains poor, and the 5-year survival rate was less than 20% [3]. Moreover, 14.0–36.7% of patients have distant metastasis at initial diagnosis [4, 5], and the prognosis was poorer in HCC patients with extrahepatic metastasis than patients without it [6].
Bone metastasis (BM) is a typical metastatic pattern in HCC patients. It was reported that the incidence of BM in HCC patients ranged from 3 to 20%, and showed a rising trend [3, 7,8,9]. Although the management of HCC patients has improved in recent years, the prognosis of HCC with BM is abysmal, with a median survival of only 1–2 months [7]. Therefore, it is important to establish predictive models for predicting the BM in HCC patients and the prognosis in HCC patients with BM. In the previous studies, many risk factors and prognostic variables were identified, including SREs, AFP, Tomita scoring system, BMI, marriage status, and surgical treatment history of primary liver lesions [10,11,12,13,14]. However, no researches focused on the predictive model for predicting the BM in HCC and the prognosis of HCC with BM, which means that the probability of outcome cannot be quantified.
Nomogram is a simple, multivariate visualization tool in oncology to predict and quantify the rate of the outcome of an individual patient [15], which were used to aid clinical decisions and promote the development of precision medicine. Therefore, based on the data from the Surveillance, Epidemiology, and End Results (SEER) database, we aimed to develop two nomograms for predicting the BM in newly diagnosed HCC patients and the cancer-specific survival (CSS) of HCC patients with BM, respectively.
Methods
Study population selection
The data included in the present study were downloaded from the SEER*Stat software version 8.3.6. The analysis of the unidentified data from the SEER database was exempted from medical ethics review and didn’t require informed consent. The inclusion criteria were following: (1) Patients were histologically diagnosed as HCC from 2010 to 2015; (2) Demographic variables, including age, race, and sex were available; (3) Tumor characteristics, including histological grade, T stage, N stage, bone metastasis status were available. In addition, patients diagnosed with autopsies or death certificates were excluded from the present study. Finally, 9047 patients were used to form a cohort to study the risk factors of BM in HCC patients and establish a predictive nomogram. Afterward, HCC patients with BM with survival time ≥ one month, specific metastasis data, including liver metastasis, lung metastasis, and brain metastasis, and specific treatment information, including surgery, radiotherapy, and chemotherapy, were used to form a new cohort to explore the prognostic factors for HCC patients with BM and develop a prognostic nomogram. Ultimately, 190 patients were used to study the prognostic factors of HCC with BM. For each cohort, patients were randomly divided into the training set(70%) and testing set(30%). In the present study, patients in the training set were used to develop the nomogram, and patients in the testing set were used to validate it.
Data collection
In the present study, seven variables were used to identify the risk factors of BM from HCC, including age, sex, race, grade, T stage, and N stage. For the study about the prognostic factors for HCC patients with BM, three treatment variables, including surgery (Performed or not performed), chemotherapy (Performed or not performed), and radiotherapy (Performed or not performed), and metastasis data, including liver metastasis(Yes or no), lung metastasis, and brain metastasis, were also included. In this part, CSS was the primary outcome, which was defined as the time interval between the day of diagnosis and the day of death due to cancer.
Statistical analysis
All statistical analysis in our present study was conducted with SPSS 25.0 and R software (version 3.6.1). The chi-square test was used to compare the variables between the training set and the testing set. In the present study, a p-value < 0.05(two sides) was considered as statistical significance. Univariate logistic analysis was applied to identify BM-related factors. The variables with p value< 0.05 in the univariate logistic analysis were included in the multivariate binary logistic regression analysis to determine independent risk factors of BM in initially diagnosed HCC patients. For prognostic factors, the univariate Cox regression analysis was applied to identify prognostic variables. Then, significant variables in the univariate Cox regression analysis were incorporated into the multivariate Cox regression analysis, and the independent prognostic factors of HCC with BM were identified.
The predictive and prognostic nomograms were developed by the “rms” package in R software based on the independent predictive factors and prognostic factors, respectively [16]. Meanwhile, the receiver operating characteristic (ROC) curve for the predictive nomogram and the time-dependent ROC curve for the prognostic nomogram were generated [17]. The area under the curve (AUC) was used to evaluate the discrimination of nomograms. In addition, ROC curves or time-dependent ROC curve of all independent variables were also generated, AUCs of all independent variables were compared with the AUC of the nomogram. Moreover, the calibration curves and decision curve analysis (DCA) curves were established for the nomogram [18]. Finally, according to the median of risk score, all patients were divided into the high-risk and low-risk groups, and the survival curve with a log-rank test was used to verify the prognostic value of nomogram [19].
Results
The characteristics of the study population
According to the selection process, a total of 9047 patients were included in our research. Meanwhile, 6335 patients were incorporated into the training set, and the remaining 2712 patients were incorporated into the testing set. The baselines of 9047 patients were shown in Table 1.
Risk factors of bone metastasis in HCC patients
In 9047 patients, 232 cases (2.6%) with BM at initial diagnosis and 8815 cases (97.4%) without it. To identify BM-related variables in HCC patients, univariate logistic analysis was used to analyze seven predictors. The results revealed that five predictors were related to BM in HCC patients, including race, sex, histological grade, T stage, and N stage (Table 2). Then, the multivariate logistic regression analysis showed that male patients (P = 0.023), higher grade (P = 0.002), higher T stage patients (P < 0.001), and higher N stage patients (P < 0.001) were independent predictors of BM in newly diagnosed HCC patients (Table 2).
Development and validation of a diagnostic nomogram for BM in newly diagnosed HCC patients
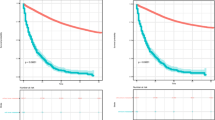
Based on the four independent BM-related variables, a diagnostic nomogram was established for the risk assessment of BM in newly diagnosed HCC patients (Fig. 1). Meanwhile, the ROC curves of both training set and testing set were established, and the AUC of nomogram were 0.726 in the training set and 0.629 in the testing set (Figs. 2a and 3a). More importantly, the ROC curves of each independent predictors were also generated (Fig. 4). The results showed that the AUC of all predictors alone were lower than the AUC of nomogram, no matter in the training set and testing set. Furthermore, both in the training set and testing set, the calibration curves showed a robust calibration of nomogram (Figs. 2b and 3b), and DCA indicated that this nomogram can serve as an excellent diagnostic tool for BM in newly diagnosed HCC patients(Figs. 2c and 3c).
Prognostic factors for HCC patients with BM
As shown in Table 3, 190 eligible HCC patients with BM were used to study the prognostic factors. Among 190 patients, the male patients (85.2%) were more than female patients (14.8%). And the race of 120 (63.2%) patients were White, 46 (24.2%) patients were Africa American, and 24 (12.6%) patients were other. Meanwhile, 133 patients were randomly divided into the training set, and the remaining 57 patients were incorporated into the testing set. The chi-square test showed that there were no significant differences between the training set and the testing set (Table 3).
As shown in Table 4, the univariate and multivariate Cox proportional hazard regression were performed to screen prognostic factors, which revealed that age, radiotherapy, chemotherapy, and lung metastasis were CSS-related factors, while the radiotherapy(P = 0.001), chemotherapy (P < 0.001), and lung metastasis (P < 0.001) were independently prognostic factors for HCC patients with BM.
Prognostic nomogram for HCC patients with BM
A prognostic nomogram was established based on three independent prognostic factors (Fig. 5). The AUCs of 6-, 9-, and 12-months were 0.753, 0.799, and 0.732, respectively (Fig. 6a). Afterward, we further compared the discrimination between nomogram and independent prognostic factors, and the results indicated the AUC of nomogram was higher than AUCs of all independent factors in 6-, 9-, and 12-months (Fig. 7a). In the testing set, the AUCs of 6-, 9-, and 12-months were 0.698, 0.770, and 0.823, respectively (Fig. 6c). Moreover, in the testing set, we can find that the discrimination of nomogram was also better than all independent prognostic factors in 6-, 9-, and 12-months. In addition, the Kaplan-Meier survival curve suggested that patients in the high-risk group have a worse prognosis than patients in the low-risk group (Fig. 6b and d). The calibration curves for the probability of 6-, 9-, and 12-month CSS also indicated a good consistency between nomogram-predicted CSS and the actual outcome (Fig.8a and c). In addition, the DCA curves showed that the nomogram had a good predictive efficiency for CSS of HCC patients with BM (Fig. 8b and d).
Discussion
HCC is an aggressive tumor and prone to extrahepatic metastasis, occurring in 14.0–36.7% of patients [20]. Meanwhile, the detection of extrahepatic metastasis from HCC increased because of the development of survival and diagnostic modalities [21]. Bone is a common site of extrahepatic metastasis, and the incidence ranges from 2 to 25% in HCC patients [12]. In our study, we established a diagnostic nomogram for predicting the BM in newly diagnosed HCC patients and a prognostic nomogram for HCC patients with BM. By obtaining the data of several easily accessible variables on the nomogram of each HCC patient, the total score can be calculated. Then, the risk of BM can be easily identified on the nomogram, which can provide guidance for further clinical management. Similarly, the prognosis of HCC patients with BM can be identified by prognostic nomogram. In our research, both nomograms demonstrated excellent performance in the risk assessment of BM and the survival prediction of HCC patients with BM, which will make the individualized clinical decision and surveillance more accurate.
Although the prognosis is extremely poor in HCC patients with BM, the early detection of BM could be crucial for HCC patients to receive appropriate therapy [22]. Therefore, it appears to be important for clinical decision-making to explore the risk factors for BM from HCC patients. In the molecular level, the expression of Chemokine receptor CXCR4 [23], MicroRNA-34a, [24] and LncRNA34a [25] were identified to be associated with BM in HCC patients. Nevertheless, these biomarkers were difficult and unpractical to apply immediately to clinical decisions. In addition, as for some practical clinical features, it was reported that marital status, T stage, N stage were risk factors for BM from HCC [12]. However, to date, no predictive model has been established, which means that the individual risk of BM cannot be identified by combining all independent BM-related predictors. In our study, the results showed that sex, grade, T stage, and N stage were the significant predictors for BM from HCC. The association between these factors and BM in HCC patients has been reported in previous researches. The association between tumor differentiation and TNM stage and BM in HCC patients has been confirmed in the previous study [26]. Another improvement of the nomogram was that the discrimination of nomogram was confirmed higher than any single predictors, which also showed the importance of a comprehensive predictive model.
In addition, our research showed that HCC patients with BM with lung metastasis, absence of chemotherapy, and absence of radiotherapy had unfavorable prognosis. Based on three independent prognostic factors, a nomogram was established. The results indicated that the nomogram can serve as an effective tool to identify high-risk patients. Similarly, the relationship between lung metastasis, chemotherapy, and radiotherapy and the prognosis in HCC patients have been widely reported in previous researches. In 2017, Yang et al. reported that multiple tumors and extrahepatic invasion were the independent adverse prognostic factors for HCC patients [27]. Therefore, as a common extrahepatic invasion site, patients with pulmonary metastasis were worse prognosis than patients without it. HCC with extrahepatic spread is considered to be in the advanced stage, and the therapeutic recommendation for this stage is oral sorafenib treatment [3]. Sorafenib had a positive effect on the survival of patients with advanced HCC [28]. Meanwhile, systemic chemotherapy with doxorubicin, gemcitabine or combined regimens for palliative care also improved HCC patients survival [3]. It was consistent with those reports that the absence of chemotherapy could lead to poor prognosis for HCC patients with BM and be an independent prognostic factor in our study. Generally, radiotherapy is a kind of treatment for uncomplicated symptomatic bone metastasis from HCC, aimed at palliation of symptoms [22, 29]. In the previous reports, radiotherapy was shown to provide effective palliation for patients with painful BM from HCC [9, 30]. In our research, radiotherapy showed favorable CSS in multivariate Cox regression analysis. Therefore, we recommend paying attention to the possibility of lung metastasis in patients with BM of HCC. For the sake of good prognosis, clinical treatment in HCC patients with BM could tend to be radiotherapy and chemotherapy. And further studies of significant prognostic factors for CSS in HCC with BM are necessary.
However, several limitations to our study should be noted. First, limited patients (N = 190) may result the possible error. Second, the information collected in the SEER database was about the disease at the first diagnosis, which meant that the bone metastasis occur in the latter stage cannot be recorded. Third, this was a retrospective study in which selection bias existed inevitably, and the information about detailed treatment was not available in the SEER database.
Conclusions
Our study showed that sex, grade, T stage, and N stage were the risk factors of BM from HCC. As for HCC patients with BM, lung metastasis, chemotherapy, and radiotherapy were independent prognostic factors for CSS. Two nomograms we created may be individual, convenient, and more intuitive visual tools for risk assessment and prognostic prediction for BM from HCC.
Availability of data and materials
The dataset from SEER database generated and/or analyzed during the current study are available in the SEER dataset repository (https://seer.cancer.gov/).
Abbreviations
- BM:
-
Bone metastasis
- HCC:
-
Hepatocellular carcinoma
- SEER:
-
Surveillance, Epidemiology, and End Results
- ROC:
-
Receiver operating characteristic
- DCA:
-
Decision curve analysis
- CSS:
-
Cancer-specific survival
- AUC:
-
Area under the curve
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391(10127):1301–14.
Lin S, Hoffmann K, Schemmer P. Treatment of hepatocellular carcinoma: a systematic review. Liver Cancer. 2012;1(3–4):144–58.
Katyal S, Oliver JH 3rd, Peterson MS, Ferris JV, Carr BS, Baron RL. Extrahepatic metastases of hepatocellular carcinoma. Radiology. 2000;216(3):698–703.
Shuto T, Hirohashi K, Kubo S, Tanaka H, Yamamoto T, Higaki I, Takemura S, Kinoshita H. Treatment of adrenal metastases after hepatic resection of a hepatocellular carcinoma. Dig Surg. 2001;18(4):294–7.
Elmoghazy W, Ahmed K, Vijay A, Kamel Y, Elaffandi A, El-Ansari W, Kakil R, Khalaf H. Hepatocellular carcinoma in a rapidly growing community: epidemiology, clinico-pathology and predictors of extrahepatic metastasis. Arab J Gastroenterol. 2019;20(1):38–43.
Attili VS, Babu KG, Lokanatha D, Bapsy PP, Ramachandra C, Rajshekar H. Bone metastasis in hepatocellular carcinoma: need for reappraisal of treatment. J Cancer Res Ther. 2008;4(2):93–4.
Okazaki N, Yoshino M, Yoshida T, Hirohashi S, Kishi K, Shimosato Y. Bone metastasis in hepatocellular carcinoma. Cancer. 1985;55(9):1991–4.
Fukutomi M, Yokota M, Chuman H, Harada H, Zaitsu Y, Funakoshi A, Wakasugi H, Iguchi H. Increased incidence of bone metastases in hepatocellular carcinoma. Eur J Gastroenterol Hepatol. 2001;13(9):1083–8.
Lee MH, Lee SH, Kim ES, Eoh W, Chung SS, Lee CS. Survival-related factors of spinal metastasis with hepatocellular carcinoma in current surgical treatment modalities : a single institute experience. J Korean Neurosurg Soc. 2015;58(5):448–53.
Chang YS, Huang JS, Yen CL, Chien RN, Wang CH, Lai CH, Wu TH, Lan YJ, Yeh KY. Body mass index above 24 is beneficial for the 6-month survival rate in hepatocellular carcinoma patients with extrahepatic metastases. Asia Pac J Clin Nutr. 2017;26(4):637–41.
Guo X, Xu Y, Wang X, Lin F, Wu H, Duan J, Xiong Y, Han X, Baklaushev VP, Xiong S. Advanced Hepatocellular Carcinoma with Bone Metastases: Prevalence, Associated Factors, and Survival Estimation. Med Sci Monit. 2019;25:1105-12.
Seo HJ, Kim GM, Kim JH, Kang WJ, Choi HJ. 18F-FDG PET/CT in hepatocellular carcinoma: detection of bone metastasis and prediction of prognosis. Nucl Med Commun. 2015;36(3):226–33.
Harding JJ, Abu-Zeinah G, Chou JF, Owen DH, Ly M, Lowery MA, Capanu M, Do R, Kemeny NE, O'Reilly EM, et al. Frequency, morbidity, and mortality of bone metastases in advanced hepatocellular carcinoma. J Natl Compr Cancer Netw. 2018;16(1):50–8.
Balachandran VP, Gonen M, Smith JJ, DeMatteo RP. Nomograms in oncology: more than meets the eye. Lancet Oncol. 2015;16(4):e173–80.
Harrell FE Jr. rms: Regression Modeling Strategies: R package version 5.1-4. https://CRAN.R-project.org/package=rms. Accessed 22 Jan 2020.
Heagerty PJ, Lumley T, Pepe MS. Time-dependent ROC curves for censored survival data and a diagnostic marker. Biometrics. 2000;56(2):337–44.
Vickers AJ, Elkin EB. Decision curve analysis: a novel method for evaluating prediction models. Med Decis Mak. 2006;26(6):565–74.
Ranstam J, Cook J. Kaplan-Meier curve. Br J Surg. 2017;104(4):442.
Natsuizaka M, Omura T, Akaike T, Kuwata Y, Yamazaki K, Sato T, Karino Y, Toyota J, Suga T, Asaka M. Clinical features of hepatocellular carcinoma with extrahepatic metastases. J Gastroenterol Hepatol. 2005;20(11):1781–7.
Uka K, Aikata H, Takaki S, Shirakawa H, Jeong SC, Yamashina K, Hiramatsu A, Kodama H, Takahashi S, Chayama K. Clinical features and prognosis of patients with extrahepatic metastases from hepatocellular carcinoma. World J Gastroenterol. 2007;13(3):414–20.
Bhatia R, Ravulapati S, Befeler A, Dombrowski J, Gadani S, Poddar N. Hepatocellular carcinoma with bone metastases: incidence, prognostic significance, and management-single-center experience. J Gastrointest Cancer. 2017;48(4):321–5.
Xiang ZL, Zeng ZC, Tang ZY, Fan J, Zhuang PY, Liang Y, Tan YS, He J. Chemokine receptor CXCR4 expression in hepatocellular carcinoma patients increases the risk of bone metastases and poor survival. BMC Cancer. 2009;9:176.
Xiang ZL, Zhao XM, Zhang L, Yang P, Fan J, Tang ZY, Zeng ZC. MicroRNA-34a expression levels in serum and intratumoral tissue can predict bone metastasis in patients with hepatocellular carcinoma. Oncotarget. 2016;7(52):87246–56.
Zhang L, Niu H, Ma J, Yuan BY, Chen YH, Zhuang Y, Chen GW, Zeng ZC, Xiang ZL. The molecular mechanism of LncRNA34a-mediated regulation of bone metastasis in hepatocellular carcinoma. Mol Cancer. 2019;18(1):120.
Xiang ZL, Zeng ZC, Fan J, Wu WZ, He J, Zeng HY, Tang ZY. A clinicopathological model to predict bone metastasis in hepatocellular carcinoma. J Cancer Res Clin Oncol. 2011;137(12):1791–7.
Wang YK, Bi XY, Li ZY, Zhao H, Zhao JJ, Zhou JG, Huang Z, Zhang YF, Li MX, Chen X, et al. A new prognostic score system of hepatocellular carcinoma following hepatectomy. Zhonghua Zhong Liu Za Zhi. 2017;39(12):903–9.
Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S, Kim JS, Luo R, Feng J, Ye S, Yang TS, et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009;10(1):25–34.
Jung IH, Yoon SM, Kwak J, Park JH, Song SY, Lee SW, Ahn SD, Choi EK, Kim JH. High-dose radiotherapy is associated with better local control of bone metastasis from hepatocellular carcinoma. Oncotarget. 2017;8(9):15182–92.
Seong J, Koom WS, Park HC. Radiotherapy for painful bone metastases from hepatocellular carcinoma. Liver Int. 2005;25(2):261–5.
Acknowledgements
None.
Funding
We received no external funding for this study.
Author information
Authors and Affiliations
Contributions
C H, JX Y, and CL Z conceived of and designed the study. C H, ZH H and C L performed literature search. CL W, ZY F, YJ L and B C generated the figures and tables. YX T and B C analyzed the data. C H wrote the manuscript and CL Z critically reviewed the manuscript. CL Z supervised the research. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
We received permission to access the research data file in the SEER program from the National Cancer Institute, US (reference number 15260-Nov2018). Approval was waived by the local ethics committee, as SEER data is publicly available and de-identified.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hu, C., Yang, J., Huang, Z. et al. Diagnostic and prognostic nomograms for bone metastasis in hepatocellular carcinoma. BMC Cancer 20, 494 (2020). https://doi.org/10.1186/s12885-020-06995-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-020-06995-y