Abstract
Background
Somatic PTEN mutation occurs in a proportion of ovarian endometrioid carcinomas. However, these cancers have seldom been reported in diseases associated with germline PTEN variants, such as Cowden syndrome (CS).
Case presentation
The present case was a 39-year-old woman with a left ovarian carcinoma who demonstrated a germline splice variant of PTEN (c.1026 + 1G > T) following genome-wide whole exome sequencing of her germline DNA. Histology of her resected tumor revealed endometrioid carcinoma of the same type as a right ovarian cancer resected eight years previously. These tumors showed null immunostaining for PTEN. She was genetically diagnosed with CS. Despite her clinical examinations had demonstrated several characteristic findings of CS, including mammary fibroma, esophageal and skin papilloma, colonic hamartoma, uterine myoma, and lipoma, the clinicians could not approach this diagnosis.
Conclusion
Ovarian endometrioid carcinoma is generally thought to develop from endometrial tissue menstruated from the uterus and implanted on the ovary. To date, ovarian cancers have not been listed as CS-related cancers; however, ovarian endometrioid cancer can have a potential association with CS in endometriosis cases.
Similar content being viewed by others
Background
Pathogenic variants of germline PTEN result in autosomal dominant hereditary disease or PTEN hamartoma tumor syndromes (PHTS), including Proteus syndrome (PS), Proteus-like syndrome (PLS), Bannayan-Riley-Ruvalcaba syndrome (BRRS), and Cowden syndrome (CS). CS is clinically diagnosed based on the major criteria associated with three types of cancer (breast, thyroid, and endometrium) and macrocephaly, as well as by minor criteria that include other benign thyroid lesions; intellectual disability (IQ ≤75); intestinal hamartomatous polyps; mammary fibrocystic disease; lipomas; fibromas; genitourinary tumors and malformation; and uterine fibroids [1].
Ovarian cancer is not included in the above criteria, but uterine endometrial carcinoma is included. Ovarian endometrioid carcinoma is thought to develop from endometrial tissue menstruated from the uterus and implanted on the ovary [2]. We report a unique case of CS who had a germline PTEN splice variant and subsequently developed metachronous bilateral ovarian endometrioid carcinomas without expressing the PTEN protein.
Case presentation
The patient was a Japanese woman with a past history of left ovarian endometrioid carcinoma (grade 2, FIGO stage IC1) that had been resected by salpingo-oophorectomy, omentectomy and retroperitoneal lymph node biopsy (fertility sparing surgery) when she was 31 years old. She had a history of multiple thyroid goiters (maximum 2 cm), bilateral breast fibroma treated by surgical resection at age 15, endometriosis (at age 28) and myoma, and salpingitis treated by peroral medications (at age 28). She was intellectual enough to evaluate her IQ over 75. While in her 30s, she sometimes complained of lower abdominal pain and melena. A colonoscopy revealed colorectal polypoid lesions that were histologically diagnosed by forceps biopsy as hamartoma polyps and ectopic endometrial implants (Fig. 1a, b). An upper gastrointestinal endoscopy screening demonstrated multiple esophageal papillomas and glycogenic acanthosis (Fig. 1c). A gluteal subcutaneous lipoma, 55 mm in size, was detected by screening magnetic resonance imaging (MRI). The patient’s mother died of breast cancer in her 40s, and her father had a pathology-confirmed cutaneous papilloma on his head and neck. The patient had no smoking or drinking habits.
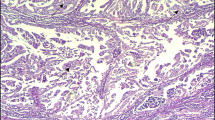
The patient had been undergoing surveillance for the endometriosis by yearly pelvic image examinations, and a right ovarian tumor was detected at age 39. Computed tomography (CT) demonstrated a heterogeneously enhanced mass, 9 cm in size, while 18F-fluorodeoxyglucose-positron emission tomography (FDG-PET) showed abnormal uptake by the ovarian tumor (SUVmax: 8.33). She underwent abdominal total hysterectomy, right salpingo-oophorectomy, pelvic lymphadenectomy and para-aortic lymphadenectomy. Endometrioid carcinoma (grade 1, FIGO stage: IC2), partially accompanied with components of squamous metaplasia and low-grade adenofibroma, was detected in the resected ovary. Immunostainings of the right-ovarian endometrial carcinoma revealed high expression of estrogen receptor, PI3K, and Ki-67 (labeling index approximately 40%), but TP53 showed no overexpression, and PTEN, WT1, Napsin A, and HNF-1β were not expressed (Fig. 2). Immunostainings of PI3K showed diffuse expression, but PTEN was not expressed, as also determined in the left ovarian tumor.
Pathology of the right-ovarian tumor. a Hematoxylin and eosin (H&E) staining showing endometrioid carcinoma, grade 1 (× 40). Immunostaining of the tumor showing diffuse expression of estrogen receptor (× 100)(b) and PI3K (× 100)(c). d Null expression of PTEN in the tumor, contrasting with the positive expression in the interstitial cells and inflammatory cells (× 100)
All resected lymph nodes were negative for cancer (0/120). Her uterus specimen confirmed myomas and endometriosis.
Upon full informed consent, the patient participated in genetic research at the time of surgery. Peripheral blood and a 4–5 mm3 area of fresh right-ovarian cancer tissue were taken at surgery for whole exome sequencing (WES) to compare germline DNA and cancer DNA using a next-generation sequencer [3, 4]. An exome library, including 723 cancer-associated genes and 49 genes [3] responsible for hereditary cancer syndromes, was prepared using the Ion AmpliSeq Exome RDY kit (Thermo Fisher Scientific, Massachusetts, USA). Exome sequencing of the right endometrioid carcinoma revealed a pathogenic mutation of hexose-6-phosphate dehydrogenase/glucose 1-dehydrogenase (H6PD), TFAP2D, MYO7A, TGM1, SEMA6B, ZNF99, and SIGLEC1. Loss of heterozygosity (LOH) in the 10q.23.3 (PTEN) locus was not recognized by copy number variation analysis in this tumor DNA. Her blood DNA demonstrated a splice-donor site variant of PTEN (c.1026 + 1G > T) [5], that had been reported to be causative of intellectual disability. This sequence was confirmed by the Sanger sequencing (Fig. 3). No other germline mutation or incidental pathogenic finding was recognized.
Despite a number of characteristic findings in her demographics, images and pathologies, the clinicians did not approach the diagnosis of Cowden syndrome (CS) until the detection of germline PTEN variant. At the counseling, multiple (> 6) palmar small papules, buccal papillomas, and macrocephaly (head circumference: 60 cm, > 97th percentile) were further recognized by the physical examinations, fully meeting the clinical criteria of CS. She received clinical surveillance of the organs associated with PHTS [1]. Her father also underwent genetic test, but the variant of PTEN was not recognized. Three years have passed since the last surgery. No recurrence has been detected.
Discussion and conclusions
An elevated risk of ovarian carcinoma has not been reported in cases with germline PTEN variants, although an association of PTEN with uterine endometrial carcinoma is well known (standardized incidence rate: 42.9, lifetime risk: 28.2%) [6]. However, ovarian endometrioid carcinoma is thought to develop from endometrial tissue menstruated in retrograde and implanted on the ovary [2]. Somatic mutation of PTEN is recognized in 53% of endometriosis cases [7], and LOH in the 10q.23.3 locus occurs in a range from 25% [8] to 84% [7]. Moreover, PTEN mutation is recognized in 20% [9, 10] of ovarian endometrioid carcinomas and the LOH is 60 [10] to 64% [8]; however, these values are much lower in other types of ovarian carcinomas (2% mutation rate; 28% LOH) [10]. These data suggest a specific association of PTEN alterations and endometrioid-type ovarian cancer.
Ovarian endometrioid carcinoma has seldom been reported in cases of Cowden syndrome (CS). The current case demonstrated metachronous bilateral ovarian endometrioid carcinoma with an 8-year interval. Endometriosis, but not endometrioid carcinoma, was recognized in the patient’s resected uterus; therefore, we speculated that an independent carcinogenesis had occurred in the bilateral ovaries or that carcinoma cells had exfoliated from the unilateral ovary and implanted to the other side. The expression patterns of PI3K and PTEN were the same; however, metastasis (from the left to the right ovary) had not been anticipated since both tumors contained low-grade components, which rarely metastasize. Our case suggested a risk for non-uterine endometrioid carcinoma in cases of CS, indicating that all ectopic endometrioses are at risk and require careful follow up or endoscopic resection of rectal endometriosis. Most recently, a case of CS was reported from France, that carried a pathogenic PTEN variant (c.388C > T) and developed an ovarian clear cell carcinoma showing loss of PTEN expression [11], like our case. Ovarian clear cell carcinoma has several biological characteristics similar to those of endometrioid carcinoma, such as a pathogenesis through the ovarian endometriosis and common somatic mutations [PIK3CA (15–60%), ARID1A (30–57%), CTNNB1 (3–53%) and DNA mismatch repair genes (4–13%)] [9, 12]. In addition to these endometriosis-associated ovarian cancers, several cases of embryonic tumors [13] and dysgerminoma [14] have also reported in cases of CS with germline PTEN variants, however their pathological and genetic rationale is unclear. These data give us a warning for the ovarian findings including endometriosis in cases of CS [15].
The patient had several characteristic CS findings that satisfied one major criteria (macrocephaly) and five minor criteria (multiple thyroid goiters, bilateral mammary fibromas, intestinal hamartomas, an uterine myoma, and a gluteal lipoma), so she could be clinically diagnosed with CS [1]. Based on the retrospective assessment using Cleveland Clinic PTEN Risk Calculator (http://www.lerner.ccf.org/gmi/ccscore/), probability of PTEN variant in this patient was estimated between 99.4 and 100%, even not including her histories of ovarian endometrioid cancers. However, she had not been diagnosed until after the genetic test for several reasons: the lack of a sense of inherited diseases in the doctor’s mind, multi-department associations beyond each doctor’s expertise field, diagnostic criteria that were characteristic but not really specific to CS, and an atypical CS cancer type. The patient did not have any children, so familial information was limited to her mother who had died of breast cancer at her 40s. In this sense, clinical cancer sequencing using next generation sequencing would potentially increase the possibility of incidentally detecting inherited cancer syndromes with atypical findings or relatively weak phenotypes.
Clinical sequencing sometimes reveals a novel variant that needs determination of its pathogenicity. The current splice donor site variant (c.1026 + 1G > T) is located at the intron 8 or C-terminal site of PTEN, and its pathogenicity has been reported previously for characteristic PTEN intellectual disability [5]. To the best of our knowledge, the current report is the first cancer case associated with this PTEN variant (c.1026 + 1G > T), and the cancer was negative for PTEN expression, as confirmed by the immunostaining antibody, clone 6H2.1, that recognizes an epitope located at the C-terminal region. PHTS has a genotype–phenotype correlation and includes a cancer-associated (CS and BRRS) and a non-cancer associated (PS and PLS) [1] group. Some PTEN variants only cause cancers but show no other criteria of CS [4]. In this sense, the current pathogenic variant of PTEN (c.1026 + 1G > T) appears to associate with a variety of characteristic CS findings.
We reported an incidentally detected case of CS in a patient who had carried a pathogenic variant of PTEN (c.1026 + 1G > T) and developed bilateral ovarian endometrioid cancers without PTEN expression. Ovarian endometrioid carcinoma can be considered a CS-associated cancer, and caution is needed for ovarian findings including endometriosis in cases of CS.
Availability of data and materials
The datasets used and/or analyzed in the current are available from the corresponding author on reasonable request.
Availability of data and materials
All data generated or analyzed during this study are included in this article.
Abbreviations
- BRRS:
-
Bannayan-Riley-Ruvalcaba syndrome
- CS:
-
Cowden syndrome
- CT:
-
Computed tomography
- FDG-PET:
-
18F-fluorodeoxyglucose-positron emission tomography
- LOH:
-
Loss of heterozygosity
- MRI:
-
Magnetic resonance imaging
- PHTS:
-
PTEN hamartoma tumor syndromes
- PLS:
-
Proteus-like syndrome
- PS:
-
Proteus syndrome
- WES:
-
Whole exome sequencing
References
Eng C. PTEN Hamartoma Tumor Syndrome (PHTS): GeneReviews [Internet] http://www.ncbi.nlm.nih.gov/books/NBK1488/, updated in 2016.
Kurman RJ, Shih IM. The origin and pathogenesis of epithelial ovarian cancer: a proposed unifying theory. Am J Surg Pathol. 2010;34:433–43.
Urakami K, Shimoda Y, Ohshima K, et al. Next generation sequencing approach for detecting 491 fusion genes from human cancer. Biomed Res. 2016;37:51–62.
Uemura S, Matsubayashi H, Kiyozumi Y, et al. Pancreatic adenocarcinoma with a germline PTEN p.Arg234Gln mutation. Familial Cancer. 2018;17:255–9.
Tatton-Brown K, Loveday C, Yost S, et al. Mutations in epigenetic regulation genes are a major cause of overgrowth with intellectual disability. Am J Hum Genet. 2017;100:725–36.
Tan MH, Mester JL, Ngeow J, et al. Lifetime cancer risks in individuals with germline PTEN mutations. Clin Cancer Res. 2012;18:400–7.
Govatati S, Kodati VL, Deenadayal M, et al. Mutations in the PTEN tumor gene and risk of endometriosis: a case-control study. Hum Reprod. 2014;29:324–36.
Xu B, Hamada S, Kusuki I, et al. Possible involvement of loss of heterozygosity in malignant transformation of ovarian endometriosis. Gynecol Oncol. 2011;120:239–46.
Sato N, Tsunoda H, Nishida M, et al. Loss of heterozygosity on 10q23.3 and mutation of the tumor suppressor gene PTEN in benign endometrial cyst of the ovary: possible sequence progression from benign endometrial cyst to endometrioid carcinoma and clear cell carcinoma of the ovary. Cancer Res. 2000;60:7052–6.
Kolasa IK, Rembiszewska A, Janiec-Jankowska A, et al. PTEN mutation, expression and LOH at its locus in ovarian carcinomas. Relation to TP53, K-RAS and BRCA1 mutations. Gynecol Oncol. 2006;103:692–7.
Yauy K, Imbert-Bouteille M, Bubien V, et al. Ovarian clear cell carcinoma in Cowden syndrome. J Natl Compr Cancer Netw. 2019;17:7–11.
Fadare O, Parkash V. Pathology of Endometrioid and clear cell carcinoma of the ovary. Surg Pathol Clin. 2019;12:529–64.
Bubien V, Bonnet F, Brouste V, et al. High cumulative risks of cancer in patients with PTEN hamartoma tumour syndrome. J Med Genet. 2013;50:255–63.
Cho MY, Kim HS, Eng C, et al. First report of ovarian dysgerminoma in Cowden syndrome with germline PTEN mutation and PTEN-related 10q loss of tumor heterozygosity. Am J Surg Pathol. 2008;32:1258–64.
Papageorgiou T, Stratakis CA. Ovarian tumors associated with multiple endocrine neoplasias and related syndromes (carney complex, Peutz-Jeghers syndrome, von Hippel-Lindau disease, Cowden's disease). Int J Gynecol Cancer. 2002;12:337–47.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
HM collected the data and wrote the manuscript, SH, YK, YH, and HM participated genetic counseling and genetically managed the patient and her family, YH and NK performed surgery and gynecological managements, MA and TO managed pathological sampling and diagnosis, SO and KU performed genetic analysis, and KY organized and approved this study. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional Review Board of Shizuoka Cancer Center ethically approved this study, and the written informed consent was obtained from the patient.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Matsubayashi, H., Higashigawa, S., Kiyozumi, Y. et al. Metachronous ovarian endometrioid carcinomas in a patient with a PTEN variant: case report of incidentally detected Cowden syndrome. BMC Cancer 19, 1014 (2019). https://doi.org/10.1186/s12885-019-6272-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-019-6272-2