Abstract
Background
Chronic inflammation and repeated infection with Opisthorchis viverrini (O. viverrini) induces intrahepatic cholangiocarcinoma (ICC). Inflammatory cytokines such as interleukin (IL) and tumor necrosis factor (TNF) are substances in the immune system that promote inflammation and causes disease to progress. Genes that help express proinflammatory cytokines can affect an individual’s susceptibility to disease, especially in cancer-related chronic inflammation. This study aimed to investigate risk factors for ICC with a focus on opisthorchiasis and polymorphisms of proinflammatory cytokines (IL-1β and TNF-α).
Methods
This study was a nested case-control study within a cohort study. 219 subjects who developed a primary ICC were identified and matched with two non-cancer controls from the same cohort based on sex and age at recruitment (±3 years). An O. viverrini-IgG antibody was assessed using enzyme linked immunosorbent assay. IL-1β and TNF-α polymorphisms were analyzed using a polymerase chain reaction with high resolution melting analysis. Associations between variables and ICC were assessed using conditional logistic regression.
Results
Subjects with a high infection intensity had higher risk of ICC than those who had a low level (OR = 2.1; 95% CI: 1.2–3.9). Subjects with all genotypes of TNF-α (GG, GA, AA) and high infection intensity were significantly related to an increased risk of ICC (p < 0.05).
Conclusions
Polymorphisms of IL-1β and TNF-α are not a risk of ICC, but an individual with O. viverrini infection has an effect on all genotypes of the TNF-α gene that might promote ICC. Primary prevention of ICC in high-risk areas is based on efforts to reduce O. viverrini infection.
Similar content being viewed by others
Background
The incidence rate of intrahepatic cholangiocarcinoma (ICC) in the Northeast – the highest incidence in Thailand – from the last report, Cancer in Thailand, Vol. VII, 2007–2009, showed that it is the most common cancer in men (age-standardized incidence rate, ASR = 67.1 per 100,000) and the third most common cancer in women (ASR = 30.9). In Khon Kaen, located in Northeast Thailand, the incidence of ICC is ASR 57.4 in men, and 23.1 in women per 100,000 [1].
ICC is a multi-factor and inflammation-linked disease. Chronic inflammation and repeated infection with liver fluke, Opisthorchis viverrini (O. viverrini), induces ICC development [2,3,4]. Inflammatory cytokines increase inflammation and can cause diseases to progress rapidly. Interleukin-1β (IL-1β) and tumor necrosis factor-β (TNF-α) are inflammatory mediators that have been implicated in carcinogenesis due to its participation in chronic inflammatory diseases [5] including ICC [6]. The genesis of ICC is a multistep process, which required interaction between mutated biliary epithelial cells and environmental factors [7]. During ICC development, chronic inflammation of the bile duct caused by O. viverrini infection can induce the epithelial cells to produce a variety of cytokines, including IL-6, IL-8, TGF-β and TNF-α [8]. This can cause bile duct epithelial cell proliferation and impaired epithelial barrier function. As a result, somatic mutations occur in several tumor-related genes, leading to cholangiocarcinogenesis [6, 8,9,10]. Some studies reported the expression of TNF-α associated with ICC [6, 9], but genetic polymorphisms in TNF-α and ICC risk has not been explored so far and requires further study. IL-1β is a proinflammatory cytokine with multiple biological effects [11]. It has been implicated as an important factor for cancer progression. Genetic polymorphisms in IL-1β are associated with gastric cancer [12], hepatitis C virus [13,14,15] and hepatitis B virus [16] linked with hepatocellular carcinoma (HCC). However, there is no study of IL-1β genetic polymorphisms on ICC risk. The present study therefore aims to investigate risk factors for ICC and inflammation-linked cancer, and focus on opisthorchiasis and polymorphisms in proinflammatory cytokines (IL-1β and TNF-α) to assess whether these genes are involved in opisthorchiasis-related ICC risk.
Methods
Study design
This study was a part of a larger study known as the Khon Kaen Cohort Study (KKCS) that was previously conducted [17,18,19,20]. This was a suitable platform to test the hypothesis on a host-environment interaction influence risk of ICC. Briefly, positive subjects of ICC (ICD-10: 22.1) and a sample of non-affected controls that were enrolled participants in the KKCS were used in these experiments.
Study subjects
Among the 23,584 subjects admitted in the KKCS (male 32.6%: female 67.4%), 219 cohort participants (0.9%) that developed a primary malignancy of the intrahepatic bile ducts of the liver (C22.1) were identified (male 57.0%: female 43.0%). Since ICC is rarely diagnosed by liver biopsy and histopathology (6.9%), the criteria for inclusion as a case included diagnosis at least by ultrasound, with or without contrast radiology (9.6%) and tumor markers such as CA19–9 (83.5%). The vital status and date of death for potential cases were ascertained by linkage to the file of deaths in Thailand, in the database of the National Health Security Office (NHSO), together with the demographic database of Ministry of Interior. All ICC cases died within 2 years of diagnosis. Two non-cancer controls from the same cohort population were randomly selected for matching with each case based on sex and age at recruitment (±3 years).
Detection of O. viverrini-IgG antibody
Detection of O. viverrini-IgG antibody was assessed at the parasitological laboratory, Faculty of Medicine, Khon Kaen University, Thailand. The indirect enzyme linked with immunosorbent assay (ELISA) was used to analyze a serum of cases and their matched controls as reported before [21, 22]. The samples were analyzed as duplicates with the optical density (OD) at 620 nm under the ELISA reader. The mean OD was used as the cut-off value, OD ≤0.24 and OD > 0.24.
Analysis of IL-1β and TNF-α polymorphisms
Genomic DNA was extracted from buffy coat fractions of 170 cases (77.6%) of 219 eligible ICC cases and 355 (81.0%) of 438 matched controls using the standard protocols of Genomic DNA mini Kit with Proteinase K (Geneaid Biotech).
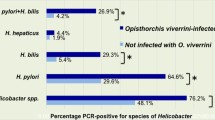
The amplification of IL-1β C-511 T was achieved by using two primers, [F]:5′- AATTTCTCAGCCTCCTACTTC-3′ and [R]: 5′- GTTTGGTATCTGICCGTTTC-3′. The TNF-α G308A gene was amplified by using [F]: 5′- TAGGTTTTGAGGGGCATG -3′ and [R]: 5′- CTGGGICCCTGACTGATTT-3′ in a PCR reaction. Both genetic polymorphisms were performed in a LightCycler® 480 Real-Time PCR System with a final volume of 20 μl containing 10 μl of master mix, 4.4 μl of H2O, 3 mM of MgCl2, 0.3 μM of each primer and 200 ng of the DNA template. The data of high resolution melting analysis was analyzed using the LightCycler 480® Gene Scanning Software version 1.5 (Roche). Normalized melting curves and melting peaks of sequence variation were evaluated and compared with the wild-type sample. Different plots of melting peaks are illustrated in Fig. 1a for IL-1β C-511 T and Fig. 1b for TNF-α G-308A. Sequence variations were distinguished by the different shape of melting curves (Fig. 1c for IL-1β C-511T and Fig. 1d for TNF-α G-308A). To improve the genotyping quality and validation, 10% of random genotyping samples were confirmed by the PCR with restriction fragment length polymorphism techniques (PCR-RFLP).
Statistical analysis
The link between O. viverrini infection intensity and proinflammatory cytokines polymorphisms (IL-1β and TNF-α) with the risk of developing ICC and odds ratios (ORs) were assessed and estimated at the 95% confidence and conditional logistic regression. The information about smoking, alcohol, and diet that was used for the adjusted ORs from the multivariate analysis in Table 2 has been previously reported [19, 20]. Possible modifications of the effects of O. viverrini infection intensity by proinflammatory cytokines polymorphisms (IL-1β and TNF-α) were also analyzed. Results that showed a p-value < 0.05 were statistically significant from the native control.
Results
Out of 23,584 participants, 219 (0.9%) subjects developed ICC. This was comprised of 92 females and 127 males and with a median age of 57 years (Table 1). Additionally, there were two controls of the same sex and age for each case.
Table 2 shows the adjusted odds ratios (OR) and 95% CIs from the multivariate analyses, including the 10 factors identified as increasing risk in univariate analysis of ICC associated with O. viverrini infection intensity, IL-1β and TNF-α polymorphisms. Participants who had the O. viverrini-IgG antibody (OD > 0.24) possessed a higher risk for ICC than those who did not (OD ≤0.24) (adjusted OR 2.1; 95% CI: 1.2–3.9). In comparison, participants with TT variant of IL-1β C-511 T polymorphisms had a decreased risk of ICC (adjusted OR 0.4; 95% CI: 0.2–0.8). Results of interactions between O. viverrini infection intensity and IL-1β and TNF-α polymorphisms on the risk of ICC have been shown in Table 3. Participants with TNF-α in all genotypes (GG, GA, AA) who had high infection intensity (IgG antibody > 0.24) had an increased risk of ICC and were statistically significant (OR 2.1 for GG wild-type, OR 2.4 for GA heterozygote and OR 2.8 for AA variant). There were no interactions between O. viverrini infection intensity and the polymorphisms of IL-1β and TNF-α that influenced the risk of ICC.
Discussion
In this work, our results successfully demonstrated the risk factors for ICC. For example, O. viverrini infection intensity detected by the IgG antibody was a risk factor for ICC and was comparable to previously reported studies in Northeast Thailand – Khon Kaen, [21] Nakhon Phanom [22] and Ubon Ratchathani [23]. Results obtained in this work showed the modified effects of O. viverrini infection with TNF-α codon 308 AA variant. Participants with only O. viverrini infection intensity had adjusted OR 2.1 (95% CI: 1.2–3.9), but participants who had both O. viverrini infection intensity together with AA variant of TNF-α had an increased OR of 2.8 (95% CI: 1.4–5.8).
The genotype frequencies of IL-1β C-511 T and TNF-α G308A polymorphisms found in the controls were consistent with other studies in Thailand [16, 24]. Prevalence of C and T alleles of IL-1β codon 511 were 45.9% vs. 46.4% and 54.1% vs. 53.6%, respectively. In addition, the allele distribution of TNF-α G308A was also consistent as reported before [24].
Very limited information exists in Thailand that reported the associations of IL-1β C-511 T and TNF-α G-308A polymorphisms with the risk of various cancers, especially in chronic hepatitis B virus infection-linked HCC [16, 24]. Although, there was no study about the association of IL-1β C-511 T and TNF-α G308A polymorphisms on ICC risk until now, the study on cytokines expression related cancer has been reported which acts as a diagnostic marker for cancer. The detection of serum levels of cytokines (such as IL-6 or IL-10) may be linked to the process of carcinogenesis or poor prognosis [25,26,27,28]. In our current study of ICC, the role of TNF-α in inducing epithelial-mesenchymal transition (EMT) of ICC cells has been published recently [6]. Moreover, the profile of cytokine production in peripheral blood mononuclear cells collected from subjects with and without O. viverrini infection was evaluated. Eleven cytokine profiles (IFN-γ, IL-1β, IL-2, IL-4, IL-5, IL-6, IL-8, IL-10, IL-12p70, TNF-α and LT-α), measured by flow cytometry, revealed that both pro-inflammatory and anti-inflammatory cytokines were increased in the O. viverrini-associated ICC compared to uninfected normal controls [29].
The basis of diagnosis of ICC was rarely done by histology (6.9%), and it is possible that other cases of fatal liver disease showing features of biliary obstruction, with a low serum alpha-fetoprotein, were possibly included in the case group. Despite this, the overall results support our hypothesis and are a pivotal factor in formulating experiments for future projects.
Conclusions
There was a known association between the polymorphisms of IL-1β and TNF-α. Polymorphisms of IL-1β C-511 T and TNF-α G-308A are not a risk of ICC but an individual with O. viverrini infection has effects on all genotypes of the TNF-α gene (GG, GA, AA) that might promote ICC. Primary prevention of ICC in high-risk areas is based on efforts to reduce O. viverrini infection.
Abbreviations
- ASR:
-
Age-standardized incidence rate
- ELISA:
-
Enzyme linked immunosorbent assay
- HCC:
-
Hepatocellular carcinoma
- ICC:
-
Intrahepatic cholangiocarcinoma
- IL:
-
Interleukin
- KKCS:
-
Khon Kaen Cohort Study
- NHSO:
-
National Health Security Office
- O. viverrini :
-
Opisthorchis viverrini
- OD:
-
Optical density
- OR:
-
Odds ratios
- PCR-HRM:
-
Polymerase chain reaction with high resolution melting analysis
- TNF:
-
Tumor necrosis factor
References
Khuhaprema T, Attasara P, Sriplung H, Wiangnon S, Sangkrajrang S. Cancer in Thailand, Vol. VII, 2007–2009. Bangkok: Bangkok Medical Publisher; 2013.
Pinlaor S, Ma N, Hiraku Y, Yongvanit P, Semba R, Oikawa S, et al. Repeated infection with Opisthorchis viverrini induces accumulation of 8-nitroguanine and 8-oxo-7,8-dihydro-2′-deoxyguanine in the bile duct of hamsters via inducible nitric oxide synthase. Carcinogenesis. 2004;25:1535–42.
Thanan R, Oikawa S, Yongvanit P, Hiraku Y, Ma N, Pinlaor S, et al. Inflammation-induced protein carbonylation contributes to poor prognosis for cholangiocarcinoma. Free Radic Biol Med. 2012;52:1465–72.
Thanan R, Pairojkul C, Pinlaor S, Khuntikeo N, Wongkham C, Sripa B, et al. Inflammation-related DNA damage and expression of CD133 and Oct3/4 in cholangiocarcinoma patients with poor prognosis. Free Radic Biol Med. 2013;65:1464–72.
Popa C, Netea MG, van Riel PLCM, van der Meer JWM, Stalenhoef AFH. The role of TNF-alpha in chronic inflammatory conditions, intermediary metabolism, and cardiovascular risk. J Lipid Res. 2007;48:751–62.
Techasen A, Namwat N, Loilome W, Bungkanjana P, Khuntikeo N, Puapairoj A, et al. Tumor necrosis factor-α (TNF-α) stimulates the epithelial-mesenchymal transition regulator snail in cholangiocarcinoma. Med Oncol. 2012;29:3083–91.
Landskron G, De la Fuente M, Thuwajit P, Thuwajit C, Hermoso MA. Chronic inflammation and cytokines in the tumor microenvironment. J Immunol Res. 2014;2014:149185.
Al-Bahrani R, Abuetabh Y, Zeitouni N, Sergi C. Cholangiocarcinoma: risk factors. environmental influences and oncogenesis Ann Clin Lab Sci. 2013;43:195–210.
Hanada S, Harada M, Koga H, Kawaguchi T, Taniguchi E, Kumashiro R, et al. Tumor necrosis factor-alpha and interferon-gamma directly impair epithelial barrier function in cultured mouse cholangiocytes. Liver Int. 2003;23:3–11.
Komori J, Marusawa H, Machimoto T, Endo Y, Kinoshita K, Kou T, et al. Activation-induced cytidine deaminase links bile duct inflammation to human cholangiocarcinoma. Hepatology. 2008;47:888–96.
Dinarello CA. Biologic basis for interleukin-1 in disease. Blood. 1996;87:2095–147.
Lee K-A, Ki C-S, Kim H-J, Sohn K-M, Kim J-W, Kang WK, et al. Novel interleukin 1beta polymorphism increased the risk of gastric cancer in a Korean population. J Gastroenterol. 2004;39:429–33.
Tanaka Y, Furuta T, Suzuki S, Orito E, Yeo AET, Hirashima N, et al. Impact of interleukin-1beta genetic polymorphisms on the development of hepatitis C virus-related hepatocellular carcinoma in Japan. J Infect Dis. 2003;187:1822–5.
Wang Y, Kato N, Hoshida Y, Yoshida H, Taniguchi H, Goto T, et al. Interleukin-1beta gene polymorphisms associated with hepatocellular carcinoma in hepatitis C virus infection. Hepatology. 2003;37:65–71.
Yeo AET, Tanaka Y, Furuta T. Interleukin 1beta gene polymorphism and hepatitis C virus-related hepatocellular carcinoma. Hepatology. 2003;38:267–8. author reply 268–9.
Hirankarn N, Kimkong I, Kummee P, Tangkijvanich P, Poovorawan Y. Interleukin-1beta gene polymorphism associated with hepatocellular carcinoma in hepatitis B virus infection. World J Gastroenterol. 2006;12:776–9.
Sriamporn S, Parkin DM, Pisani P, Vatanasapt V, Suwanrungruang K, Kamsa-ard P, et al. A prospective study of diet, lifestyle, and genetic factors and the risk of cancer in Khon Kaen Province, Northeast Thailand: description of the cohort. Asian Pac J Cancer Prev. 2005;6:295–303.
Songserm N, Promthet S, Sithithaworn P, Pientong C, Ekalaksananan T, Chopjitt P, et al. MTHFR polymorphisms and Opisthorchis viverrini infection: a relationship with increased susceptibility to cholangiocarcinoma in Thailand. Asian Pac J Cancer Prev. 2011;12:1341–5.
Songserm N, Promthet S, Sithithaworn P, Pientong C, Ekalaksananan T, Chopjitt P, et al. Risk factors for cholangiocarcinoma in high-risk area of Thailand: role of lifestyle, diet and methylenetetrahydrofolate reductase polymorphisms. Cancer Epidemiol. 2012;36:e89–94.
Songserm N, Promthet S, Pientong C, Ekalaksananan T, Chopjitt P, Wiangnon S. Gene-environment interaction involved in cholangiocarcinoma in the Thai population: polymorphisms of DNA repair genes, smoking and use of alcohol. BMJ Open. 2014;4:e005447.
Parkin DM, Srivatanakul P, Khlat M, Chenvidhya D, Chotiwan P, Insiripong S, et al. Liver cancer in Thailand. I. A case-control study of cholangiocarcinoma. Int J Cancer. 1991;48:323–8.
Honjo S, Srivatanakul P, Sriplung H, Kikukawa H, Hanai S, Uchida K, et al. Genetic and environmental determinants of risk for cholangiocarcinoma via Opisthorchis viverrini in a densely infested area in Nakhon Phanom, Northeast Thailand. Int J Cancer. 2005;117:854–60.
Manwong M, Songserm N, Promthet S, Matsuo K. Risk factors for cholangiocarcinoma in the lower part of Northeast Thailand: a hospital-based case-control study. Asian Pac J Cancer Prev. 2013;14:5953–6.
Kummee P, Tangkijvanich P, Poovorawan Y, Hirankarn N. Association of HLA-DRB1*13 and TNF-alpha gene polymorphisms with clearance of chronic hepatitis B infection and risk of hepatocellular carcinoma in Thai population. J Viral Hepat. 2007;14:841–8.
Heikkilä K, Harris R, Lowe G, Rumley A, Yarnell J, Gallacher J, et al. Associations of circulating C-reactive protein and interleukin-6 with cancer risk: findings from two prospective cohorts and a meta-analysis. Cancer Causes Control. 2009;20:15–26.
Lech-Maranda E, Bienvenu J, Michallet A-S, Houot R, Robak T, Coiffier B, et al. Elevated IL-10 plasma levels correlate with poor prognosis in diffuse large B-cell lymphoma. Eur Cytokine Netw. 2006;17:60–6.
Heikkilä K, Ebrahim S, Lawlor DA. Systematic review of the association between circulating interleukin-6 (IL-6) and cancer. Eur J Cancer. 2008;44:937–45.
Sripa B, Thinkhamrop B, Mairiang E, Laha T, Kaewkes S, Sithithaworn P, et al. Elevated plasma IL-6 associates with increased risk of advanced fibrosis and cholangiocarcinoma in individuals infected by Opisthorchis viverrini. PLoS Negl Trop Dis. 2012;6:e1654.
Surapaitoon A, Suttiprapa S, Khuntikeo N, Pairojkul C, Sripa B. Cytokine profiles in Opisthorchis viverrini stimulated peripheral blood mononuclear cells from cholangiocarcinoma patients. Parasitol Int. 2017;66:889–92.
Acknowledgements
We are grateful to all the health personnel who volunteered to assist with the mobile cancer screening program, which was the basis of this study, the Khon Kaen Cancer Registry has been established since 1985, and we also acknowledge the contribution of all registry personnel. We are grateful to Prof. Dr. Paiboon Sithithaworn, Department of Parasitology, Faculty of Medicine, Khon Kaen University, for the detection of O. viverrini-IgG antibody.
Funding
The Thailand Research Fund (Research grant No. 550502) supported this study in the design of the study, sample collection, materials and methods, interpretation of data and writing the manuscript.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
SP and NS conceived and designed the research. CP and TE contributed reagents/materials/analysis tools. SP and NS performed the research. NS and SW carried out the analyses. SWi and AA reviewed drafts of the paper. All authors contributed to the writing and revisions of the manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This present study was approved by the Khon Kaen University Ethics Committee for Human Research, based on the Declaration of Helsinki and the ICH Good Clinical Practice Guidelines; reference number HE512053. Written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Promthet, S., Songserm, N., Woradet, S. et al. Opisthorchiasis with proinflammatory cytokines (IL-1β and TNF-α) polymorphisms influence risk of intrahepatic cholangiocarcinoma in Thailand: a nested case-control study. BMC Cancer 18, 846 (2018). https://doi.org/10.1186/s12885-018-4751-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-018-4751-5