Abstract
Background
The roles of carcinoembryonic antigen (CEA), cytokeratin 19 fragments (CYFRA21-1) and neuron-specific enolase (NSE) in metastases occurrence and poor diagnosis in specific histological classifications of lung cancer need further exploring. In this study, we investigated relationship between elevated levels of three biomarkers of CEA, CYFRA21-1 and NSE (individually and in combination) and metastasis, survival status and prognosis in lung cancer patients.
Methods
Eight hundred and sixty eight lung cancer patients including adenocarcinoma (ADC, N = 445), squamous cell carcinoma (SCC, N = 215), small cell lung cancer (SCLC, N = 159) and other types (N = 49) were categorized into negative, moderate and high groups according to serum levels of biomarkers, and were then categorized into negative, single, double and triple groups according to any positive combination of three biomarkers. The cutoff values of three biomarkers for groupings were developed on the training group (N = 432) and verified in a validation group (N = 436). Clinical and laboratory characteristics were then assessed for correlation with occurrence of metastasis, survival status and prognosis between the two groups. Further correlation analyses were also conducted by different subtypes (ADC, SCC and SCLC) and tumor stages (I + II, III and IV) of lung cancers.
Results
The consistent results between training and validation group confirmed the rationality of grouping methods. CYFRA21-1 levels had stronger association with metastases and survival status than CEA and NSE in all lung cancer patients. When stratified by subtypes, these significances only existed in ADC patients for CYFRA21-1. Cox regression analyses showed that CYFRA21-1 and NSE were independent prognostic factors for lung cancer patients. However, only CYFRA21-1 was an independent prognostic factor in ADC and SCLC patients subtypes. Cox-regression results also indicated that CYFRA21-1 could act as independent prognostic factor in different stages (I + II, III and IV) of lung cancer.
Conclusion
CYFRA21-1 was more important in metastasis occurrence and in predicting poor prognosis in lung cancer patients than CEA, NSE and positive numbers of biomarkers.
Similar content being viewed by others
Background
Globally, lung cancer has the highest associated mortality among all malignant cancers [1]. The 5-year survival rate in advanced stage cancers is 15%, as compared to 80% in early stage lung cancers [2]. One of the reasons is that most patients are diagnosed at advanced stages due to lack of sensitive and specific early diagnostic biomarkers [3]. Non-small-cell lung cancer (NSCLC) accounts for approximately 85% of all lung cancers; the remaining 15% cases are classified as small cell lung cancer (SCLC) [4]. Although chemotherapy and targeted therapy are the main clinical treatment especially of stage IV patients, yet there is only 4–5% improvement in 5-year survival rates for stage I-III patients, and no significant improvement for stage IV patients [5]. The diagnostic methods include chest x-ray, computed tomography (CT) and needle biopsy of lung [6, 7]. However, the high cost and/or invasive nature of these investigations limit the widely use in clinical diagnosis.
During past decades, many advances have been made in the identification of tumor-associated markers in body fluids such as plasma, serum or bio-aerosols such as exhaled breath condensate (EBC) [8, 9]which could facilitate early detection and help for treatment monitoring [10]. For lung cancer diagnosis, the leading markers used are carcinoembryonic antigen (CEA), cytokeratin 19 fragments (CYFRA 21–1) and neuron-specific enolase (NSE). CEA, which is closely related to histological classification, is considered valuable for diagnosis of ADC [11]. CYFRA 21–1 and NSE are used for the diagnosis of SCLC [12, 13]. Increasing trend in levels of CEA, CYFRA21-1 and NSE have been associated with metastasis and poor prognosis [14–16]. However, limitations of previous studies are either in small sample sizes (N = 200-300) or not analyzed in combinations.
In this retrospective study we evaluated the predictive values of serum levels of CEA, CYFRA21-1 and NSE for prognosis and occurrence of metastasis, and the association of these biomarkers with clinical characteristics.
Methods
Patients
This study recruited 868 lung cancer patients who were admitted to West China Hospital between 2008 through 2012. All data were obtained from medical records within 2 weeks of diagnosis, and information regarding metastasis was obtained through reports of whole-body CT scan, bone scan, lymph node and fiber optic bronchoscopy biopsy. Survival time was obtained during subsequent follow-up visit or telephonic inquiry. Those patients who did not receive CEA, CYFRA21-1 and NSE determinations and lack of follow-up data were excluded. Data on stage were according to the TNM Classification of Malignant Tumors, 7th Edition [17].
The overall survival time was calculated as time from the date of diagnosis through the date of death or last follow up visit (if the exact date of death was unavailable). Prior to surgery or any other treatments, serum concentrations of CEA, CYFRA21-1 and NSE were measured by immunoassays. Based on the reported literatures, the threshold values for CEA, CYFRA21-1 and NSE levels were 3.4 ng/mL, 3.0 ng/mL and 15.0 ng/mL, respectively [17].
Study design
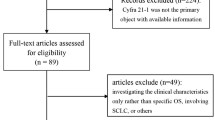
Depending on the levels of CEA, CYFRA21-1 and NSE, the study subjects were divided into three groups (negative, moderate and high). For CEA analysis, moderate and high groups were defined as 1–10 folds and >10 folds cutoff value, respectively. For CYFRA21-1 analysis 1–3 folds and >3 folds, respectively. For NSE analysis, 1–2 folds and >2 folds, respectively. This analysis was performed in a randomly selected training group (N = 432), reserving the left 436 cases for validation. The cutoff values of three biomarkers for groupings were developed on the training group and tested in a validation group.
Next, we determined the correlations of biomarker levels with three main histological subtypes, ADC, SCC and SCLC. The association analyses of other tumor types (N = 49) such as large cell lung cancers and adenosquamous carcinoma were also performed which showed no positive prognostic value (Data not shown).
Finally, the diagnosis, metastasis and prognostic values of combination patterns of three biomarkers were also evaluated. In brief, patients were grouped as negative, single, double and triple positive of biomarkers. Negative indicated that serum levels of all three biomarkers were below cutoff levels. Single, double, triple positive meant that concentrations of any one, two or all three biomarkers exceeded cutoff values.
Statistical methods
SPSS 19.0 for Windows (SPSS Inc, Chicago, USA) was used for data analyses. Chi-square test was performed to evaluate the inter-group differences. Kaplan-Meier test was used to calculate the survival status of different groups, and Log-rank test was used to compare the survival among three groups. Multivariate Cox regression analysis was used to determine the clinical characteristics, metastasis and survival status in order to estimate the hazards ratio for different serum levels of CEA, CYFRA21-1 and NSE and identify independent predictors of poor prognosis.
Results
Increased levels of CYFRA21-1 significantly correlated with metastatic disease
Total 868 lung cancer patients were randomly divided into training group (TA, 432 cases) and validation (VA, 436 cases) group to confirm the rationality of grouping methods. Among them, 320 patients tested negative (TA: 164, VA: 156) (<3.4 ng/mL) while 365 (TA: 179, VA: 186) and 210 (TA: 89, VA: 94) had moderate and high levels of CEA, respectively. For CYFRA21-1, 231 patients tested negative (TA: 115, VA: 116) while 390 (TA: 190, VA: 200) and 247 (TA: 127, VA: 120) had moderate and high levels, respectively. For NSE, 412 patients (TA: 206, VA: 206) tested negative while 256 (TA: 128, VA 128) and 200 (TA: 98, VA: 102) had moderate and high levels.
The results indicated strong correlations of increased levels of CEA, CYFRA21-1 and NSE with histological classifications in both TA and VA groups (All P < 0.001). CEA and CYFRA21-1 were also related closely to TNM stages in TA and VA groups (P < 0.05, P < 0.01 and P < 0.001), while NSE had dramatic correlation with smoke status (TA: P < 0.01, VA: P < 0.05). CEA correlated closely to bone metastasis (TA: P < 0.05, VA: P < 0.01) and NSE had significant correlation with metastasis of bone (TA: P < 0.001, VA: P < 0.01), liver (TA: P < 0.001, VA: P < 0.01), lymph node (TA: P < 0.01, VA: P < 0.01) and mediastinum (TA: P < 0.01, VA: P < 0.05) (Table 1, Additional file 1: Table S1A and B).
Among all three biomarkers, levels of CYFRA21-1significantly correlated with occurrence of organ metastasis. Besides metastasis to bone (TA: negative9.6%, moderate 25.3%, high 27.6%, P < 0.01; VA: negative 12.9%, moderate 20.0%, high 34.2%; P < 0.001) and liver (TA: negative 1.7%, moderate10.5%, high 15.6%, P < 0.01; VA: negative 5.2%, moderate11.5%, high 20.0%; P < 0.001), CYFRAY21-1 levels were also associated with metastases to lymph nodes (TA: negative 42.6%, moderate 64.2%, high 70.9%, P < 0.001; VA: negative 50%, moderate 66%, high 65.8%; P < 0.01), pleura (TA: P < 0.01, VA: P < 0.05) and peritoneum (TA: P < 0.01, VA: P < 0.01) (Table 1). However, CEA and NSE levels showed relative poor correlation with metastases (Additional file 1: Table S1A and B), which confirmed the importance of CYFRA21-1 in metastasis. Consistent results between training and validation groups also indicated the grouping rationality although several deviations such as sex, brain metastasis and adrenal gland metastasis in CYFRA21-1 and NSE, while brain and liver metastasis in CEA (Table 1, Additional file 1: Table S1A and B).
Correlation of CYFRA21-1 and NSE with metastases in ADC and SCC, respectively
In this study, the CYFRA21-1 levels showed a stronger correlation with occurrence of metastasis in ADC patients when compared with that of CEA and NSE. It also showed a significant correlation with presence of metastatic lesions in brain (P < 0.05), bone (P < 0.001), liver (P < 0.05), lymph node (P < 0.001), intrapulmonary (P < 0.05), pleural (P < 0.05) and peritoneum (P < 0.05) (Table 2). However, CEA positive levels correlated only with bone (P < 0.05) and liver metastasis (P < 0.05) (Additional file 2: Table S2A), while NSE levels correlated only with metastatic lesions in brain (P < 0.001) and bone (P < 0.001) (Additional file 2: Table S2B).
An interesting finding which differs from those reported earlier is the significant correlation of NSE levels with occurrence of metastasis in SCC patients, as compared with that of CEA and CYFRA21-1. In the present study, NSE levels were associated with occurrence of metastases to brain (P < 0.05), bone (P < 0.05), lymph nodes (P < 0.05), mediastinum (P < 0.05) and peritoneal cavity (P < 0.05) (Table 3). However, CEA levels correlated only with lymph node metastasis (Additional file 3: Table S3A), while CYFRA21-1 was associated with metastasis to brain (Negative: 5.6%; moderate: 2.4%; high: 16.0%, P < 0.05), and lymph node (Negative: 41.7%; moderate: 60%; high: 74.5%; P < 0.05) (Additional file 3: Table S3B).
In the present study, 18.3% of all subjects were small cell lung cancer (SCLC) patients. In these patients, we observed a correlation between increased levels of CEA and occurrence of mediastinal and peritoneal metastasis (P < 0.05) (Additional file 4: Table S4A); between increased levels of CYFRA21-1 and liver metastasis (P < 0.05) (Additional file 4: Table S4B); and between increased NSE levels and occurrence of lymph node metastasis (Negative: 42.1%; moderate: 60.1%; high: 77.8%;P < 0.05) (Additional file 4: Table S4C).
Increased positive numbers of biomarkers as predictors of metastases
The analysis of increased positive numbers of biomarkers in all lung cancer patients was performed in training group and validation groups. In training group, the numbers of negative, single, double and triple groups were 37, 101, 172 and 122 cases, respectively, while 27, 118, 161 and 130 in the validation group. The number TA and VA groups indicated less data deviation among different groups. The results suggested strong correlation of increased positive numbers with stages (TA: P < 0.05, VA: P < 0.05). In metastasis analysis, increased positive numbers related closely to occurrence of metastasis in bone (TA: Neg 10.8%, Single 13.9%, Double 26.2%, Triple 27.9%, P < 0.05; VA: Neg 0%, Single 12.7%, Double 23.6%, Triple 33.1%, P < 0.001) and lymph node (TA: Neg 32.4%, Single 55.4%, Double 59.9%, Triple 73.8%, P < 0.001; VA: Neg 29.6%, Single 50.8%, Double 68.9%, Triple 69.2%, P < 0.001) (Table 4).
The application of 3-tier classification to all types of lung cancers revealed that lymph node metastasis was significantly associated with increased levels of biomarkers (ADC P < 0.05; SCC P < 0.001; SCLC P < 0.05) (Additional file 5: Table S5A-C). In ADC and SCC, increased levels correlated with metastasis to both lymph nodes and other organs (Additional file 5: Table S5A-C).
CYFRA21-1 levels correlated with survival in ADC, SCC and SCLC
Kaplan-Meier survival curves were used to analyze mortality at 3–5 years using SPSS19.0. The results of 3–5 year survival analyses indicated that presence of high concentrations of CEA (TA P < 0.01; VA P < 0.01), CYFRA21-1 (TA P < 0.001; VA P < 0.001), NSE (TA P < 0.05; VA P < 0.05) and positive numbers of biomarkers (TA P < 0.001; VA P < 0.01) were closely associated with survival status in both training group and validation groups (Fig. 1a-d).
For ADC patients, high levels of CEA (P < 0.001), CYFRA21-1 (P < 0.001), NSE (P < 0.05), and numbers of increased biomarkers (P < 0.001), were all closely associated with survival status of patients (Fig. 2). In SCC patients only CYFRA21-1 was associated with mortality (Additional file 6: Figure S1A). In SCLC patients, the high concentrations of CYFRA21-1 (P < .05) and NSE (P < .05) were closely associated with survival status (Additional file 7: Figure S1B).
Multivariate Cox regression analysis to identify poor prognostic factors
We observed a significant correlation between overall survival and CYFRA21-1, NSE and occurrence of metastasis. Compared with negative group, the hazards ratio increased 1.226 in CYFRA21-1 moderate positive group (Confidence Interval [CI]: 0.977–1.537) and 1.647 in CYFRA21-1 high positive group (CI: 1.273–2.130, P < .001) (Table 5). For NSE, we did not find a significant difference between hazard risk and NSE moderate positive group (HR: 1.010, CI: 0.808–1.263) but the HR increased 1.291 in NSE high positive group compared with that of negative group (CI: 1.032–1.715, P < .05). As expected, occurrence of metastasis was an independent predictor of poor prognosis (HR: 1.291, CI: 1.025–1.625, P < .05) (Table 5).
The specific histological grade analysis indicated that high and moderate levels of serum CYFRA21-1 significantly correlated with poor prognosis (HR: 1.860, CI: 1.036–3.338, P < 0.05) in both ADC and SCLC patients (HR: 1.365, CI: 0.514–3.624, P < 0.05) respectively (Table 6). In SCC and SCLC patients, only occurrence of metastasis was an independent factor for poor prognosis (Table 6). When compared with negative groups, the number of positive biomarkers meant increased mortality risk in SCLC (Single: HR 2.107, CI 0.460–9.644; double: HR 2.247 CI 0.386–13.077; triple: HR 2.508, CI 0.231–27.287) (Table 6) although the associated P value was >0.05.
Lung cancer patients were then divided into three groups according to stages (I + II, III and IV) and Cox regression was conducted to analyze which biomarker could act as independent factor of poor prognosis in specific stage. The results indicated that CYFRA21-1 correlated dramatically with poor prognosis in all stages of lung cancer patients (Stages I-II: HR 3.666 CI: 1.095–12.279, P < 0.05; Stage III: HR 1.919 CI: 1.200–3.071, P < 0.05; Stage IV: HR 1.473 CI: 1.056–2.053, P < 0.05) (Table 7 A-C), which confirm the importance of CYFRA21-1 in poor prognosis in different stages of lung cancer besides in specific histological classifications.
Discussion
Although several tumor markers for lung cancer have been identified, none of them is specific for lung cancer diagnosis. CYFRA21-1 has been reported as a poor prognostic factor in various cancers, while NSE has been associated with metastasis, and also used for monitoring response to treatment in multiple myeloma. However, these important biomarkers have not been thoroughly investigated in lung cancer patients. In our study, analyses were performed to confirm the correlations between serums CEA, CYFRA 21–1, NSE, as well as the number of positive biomarkers and metastasis and survival status of lung cancer patients.
All patients were randomly divided into training and validation groups to confirm the grouping rationality of this study. In brief, survival curves and associations with clinical characteristics in the validation group were generally similar to those in training group, though there were some non-significant inconsistence in sex and several organs of metastasis. The results indicated that the increased levels of CYFRA21-1 were strongly associated with metastatic sites and histological grades of lung cancers in both training and validation groups. In specific histological subtypes (ADC, SCC and SCLC) analyses, we also found that CYFRA21-1 correlated more closely to metastasis and survival status than CEA and NSE. To our knowledge, these results have not been reported in any of the earlier literatures.
In multivariate Cox regression analysis, only CYFRA21-1 and NSE were found to be independent predictors of prognosis in lung cancer patients. When sub-grouped, only CYFRA21-1was an independent predictor of poor prognosis in ADC (1.86-fold increased risk in high concentration group) and SCLC (1.365-fold increased risk in moderate group) but not CEA and NSE. Finally it was found that CYFRA21-1 could act as independent factor in early (I + II) and advanced stages (III and IV) of lung cancer. Thus, CYFRA21-1 appears to be more important as a prognostic predictor than the other two biomarkers.
Several reports have reported the useful roles of CEA in diagnosis of ADC, CYFRA21-1 in SCC and NSE in SCLC [18–21]. The increased levels of biomarkers are known to correlate with cancer progression, with their sensitivity depending largely on tumor stage and histological classification [22]. In contrast with the previous reports [25], we found no correlation between increased CEA levels and brain metastasis; however, we did observe a correlation with bone, liver, pleural and peritoneal metastases. The inconsistency could be explained by the smaller sample size (approximate N = 300). Research also indicated that high circulating concentrations of CYFRA21-1 and CEA were associated with advanced stages of lung cancer; levels that were two times higher than cutoff value were associated with stage III and IV lung cancer patients [23]. Although CYFRA21-1 appears to be the most sensitive and specific marker for NSCLC [26], its relationship with different histological lung cancers has largely remained unknown. An earlier report suggested that CYFRA was a more sensitive and specific marker for SCC diagnosis and was found to be of prognostic values in patients with recurrent NSCLC receiving gefitinib therapy [27, 28]. In our study, however, high levels of CYFRA21-1 correlated with survival status in ADC and SCLC but not in SCC patients. It also could be used as an independent predictor of poor prognosis in ADC and SCLC patients. Currently, NSE is the most widely used marker for diagnosis and prognosis of SCLC patients [24]. In our study, although positive levels of NSE significantly correlated with survival in SCLC, it did not qualify as an independent predictor for poor prognosis.
Conclusions
We designed this study to evaluate whether positive levels of biomarkers correlate with occurrence of metastasis and poor survival. The retrospective design and cross-sectional nature of our study are limitations that did not permit correlation analysis for all clinic pathological parameters. Our study suggested the important role of CYFRA21-1 in predicting occurrence of metastasis as well as poor prognosis in lung cancer patients. Our results could provide important perspectives for diagnosis, prognosis and management of lung cancer.
Abbreviations
- ADC:
-
Adenocarcinoma
- CEA:
-
Carcinoembryonic antigen
- CT:
-
Computed tomography
- CYFRA21-1:
-
Cytokeratin 19 fragments
- EBC:
-
Exhaled breath condensate
- HR:
-
Hazard ration
- NSCLC:
-
Non-small cell lung cancer
- NSE:
-
Neuron-specific enolase
- SCC:
-
Squamous cell carcinoma
- SCLC:
-
Small cell lung cancer
- TA:
-
Training
- VA:
-
Validation
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65:5–29.
American cancer society. Lung cancer (non-small cell). 2012. p. 1–68.
Patz JE, Campa MJ, Gottlin EB, et al. Panel of serum biomarkers for the diagnosis of lung cancer. J Clin Oncol. 2007;25:5578–83.
Sandeler A, Gray R, Perry MC, et al. Paclitaxel-carboplatin alone or with bevacizumab for non-small cell lung cancer. N Eng J Med. 2006;335:2542–50.
Maemondo M, Inoue A, Kobayashi K, et al. Gefitinib or chemotherapy for non-small cell lung cancer with mutated EGR. N Eng J Med. 2010;362:2380–8.
Mulshine JL, D’Amico TA. Issues with implementing a high-quality lung cancer screening program. CA Cancer J Clin. 2015;64:351–63.
Johnson DH, Schiller JH. Recent clinical advances in lung cancer management. J Clin Oncol. 2014;32:1–10.
Sun N, Chen ZL, Tan FW, et al. Isocitrate dehydrogenase 1 is a novel plasma biomarker for the diagnosis of non-small cell lung cancer. Clin Can Res. 2013;19:5136–45.
Arnold JN, Saldova R, Galligan MC, et al. Novel glycan biomarkers for the detection of lung cancer. J Proteome Res. 2011;10:1755–64.
Feng Q, Yu M, Kiviat NB. Molecular biomarkers for the cancer detection in blood and bodily fluids. Crit Rev Clin Lab Sci. 2006;43:497–560.
Hsu WH, Huang CS, Hsu HS, et al. Preoperative serum carcinoembryonic antigen level is a prognostic factor in women with early non-small-cell lung cancer. Ann ThroacSurg. 2007;83:419–24.
Rastel D, Ramaioli A, Cornillie F, et al. CYFRA 21–1, a sensitive and specific new tumor marker for squamous cell lung cancer. Report of the first European multicentre evaluation. CYFRA 21–1 multicentre study group. Eur J Cancer. 1994;30A:601–6.
Li J, Dai CH, Chen P, et al. Survival and prognostic factors in small cell lung cancer. Med Oncol. 2010;1:73–81.
Jung M, Kim SH, Hong S, et al. Prognostic and predictive value of carcinoembryonic antigen and cytokeratin 19 fragment levels in advanced non-small cell lung cancer patients treated with gefitinib or erlotinib. Yonsei Med J. 2012;53:931–9.
Chu XY, Hou XB, Song WA, et al. Diagnostic values of SCC, CEA, CYFRA21-1 and NSE for lung cancer in patients with suspicious pulmonary masses: a single center analysis. Cancer Biol Ther. 2011;11:995–1000.
Hur J, Lee HJ, Nam JE, et al. Additional diagnostic value of tumor markers in cytological fluid for diagnosis of non-small-cell lung cancer. BMC Cancer. 2012;12:392.
Goldstraw P, Crowley J, Chansky K, et al. The IASLC lung cancer staging project: proposals for the revision of the TNM stage groupings in the forthcoming (Seventh) edition of the TNM classification of malignant tumors. J Thorac Oncol. 2007;2:706–14.
Wang P, Piao YZ, Zhang XH, et al. The concentration of CYFRA21-1, NSE and CEA in cerebro-spinal fluid can be useful indicators for diagnosis of meningeal carcinomatosis of lung cancer. Can Biomark. 2013;13:123–30.
Park SY, Lee JG, Kim J, et al. Preoperative serum CYFRA21-1 level as a prognostic factor in surgically treated adenocarcinoma of lung. Lung Cancer. 2013;79:156–60.
Grunnet M, Sorensen JB. Carcinoembryonic antigen (CEA) as tumor marker in lung cancer. Lung Cancer. 2012;76:138–43.
Tomita M, Shimizu T, Ayabe T, et al. Prognostic significance of tumor marker index based on preoperative CEA and CYFRA21-1 in non-small cell lung cancer. Anticancer Res. 2010;30:3009–12.
Molina R, AugeJM FX, et al. Pro-gastrin-releasing peptide (proGRP) in patients with benign and malignant diseases: comparison with CEA, SCC, CYFRA21-1 and NSE in patients with lung cancer. Anticancer Res. 2005;25:1773–8.
Lee DS, Kim YS, Jung SL, et al. The relevance of serum carcinoembryonic antigen as an indicator of brain metastasis detection in advanced non-small cell lung cancer. Tumor Biol. 2013;33:1065–73.
Okamura K, Takayama K, Izumi M, et al. Diagnostic value of CEA and CYFRA21-1 tumor markers in primary lung cancer. Lung Cancer. 2013;80:45–9.
Kosacka M, Jankowska R. Comparison of cytokeratin 19 expression in tumor tissue and serum CYFRA 21–1 levels in non-small cell lung cancer. Pol Arch Med Wewn. 2009;119:33–7.
Edelman MJ, Hodgson L, Rosenblatt PY, et al. CYFRAY 21–1 as a prognostic and predictive marker in advanced non-small-cell lung cancer in a prospective trial: GALGB 150304. J ThoracOncol. 2012;7:649–54.
Barlesi F, Tchouhadjian C, Doddoli C, et al. CYFRA 21–1 level predicts survival in non-small cell lung cancer patients receiving gefitinib as third-line therapy. Br J Cancer. 2005;92:13–4.
Petrovic M, Bukumiric Z, Zdravkoivc V, et al. The prognostic significance of the circulating neuroendocrine markers chromogranin A, pro-gastrin-releasing peptide, and neuron-specific enolase in patients with small cell lung cancer. Med Oncol. 2014;31:823.
Acknowledgements
We acknowledged to Medical Records Department for help in collecting and analyzing the all patients’ data.
Funding
This work is supported by Sichuan province science and technology support program (2014SZ0148, 2014SZ0126 and 2014SZ023) and the Nature Science Foundation of China (81201851).
These four fundings are all non-commercial research fundings and granted by nation and province. The research contents and participants of these four fundings are interconnected.
Funding 2014SZ-148 was granted to lung cancer database establishment. The part of clinical data of this research was extracted from this datablse.
Funding 2014SZ0126 and 2014SZ023 were involved the follow up data of this cohort patients in this research. These follow up data of lung cancer patients were also collected by participants of these two funding.
Funding 81201851 was granted to the research of role of exhaled breath condensate in diagnosis of early lung cancer. In this manuscript, values of plasma tumor markers including CEA, CYFRA21-1 and NSE for those diagnosed lung cancer were collected and classified according to tumor stages.
Availability of data and materials
All data generated or analyzed during this study are included in this published article (table, figure, as well as supplement tables and figures).
Authors’ contributions
All authors have read and approved the manuscript. ZL - acquisition of data, analysis and interpretation of data; manuscript writing; LD - acquisition of data, analysis and interpretation of data; manuscript writing; LL - acquisition of data, analysis and interpretation of data; PD - acquisition of data, analysis and interpretation of data; ZP - acquisition of data for follow up, interpretation of data; J-YT - acquisition of data for follow up, interpretation of data; HY - acquisition of data for follow up, interpretation of data; W-YW - acquisition of data, analysis and interpretation of data; Z-YH - acquisition of data, analysis and interpretation of data; H-YQ - acquisition of data, analysis and interpretation of data; L-YL - acquisition of data, analysis and interpretation of data; ZS - analysis and interpretation of data; Q-ZX - analysis and interpretation of data; L-WM - conception and design; interpretation of data, manuscript writing; final approval of manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
This study was approved by ethics committees of West China Hospital, Sichuan University.
For those survival data were followed up via outpatient visit, written informed consents were obtained. Part of the survival data were obtained thorough telephone follow-up, the written informed consent could not be available due to the long journey from their resident to our hospital. Under these conditions, only verbal informed consents were obtained from these subjects or their legal guardians.
Author information
Authors and Affiliations
Corresponding author
Additional files
Additional file 1: Table S1.
Association analysis between CEA, NSE and all lung cancer patients. (DOCX 36 kb)
Additional file 2: Table S2.
The association analysis between CEA, NSE positive levels and ADC patients. (DOC 55 kb)
Additional file 3: Table S3.
The association analysis between bio-markers positive levels and SCC. (DOC 65 kb)
Additional file 4: Table S4.
The association analysis between bio-markers positive levels and SCLC. (DOC 63 kb)
Additional file 5: Table S5.
The association analysis between positive numbers and ADC, SCC, SCLC patients. (DOC 59 kb)
Additional file 6: Figure S1A.
Survival functions between SCC patients and the level of CEA, CYFRA21-1, NSE and positive numbers. *P < 0.05, **P < 0.001. (TIF 1909 kb)
Additional file 7: Figure S1B.
The survival functions analysis in SCLC patients based on increased concentrations in CEA, CYFRA21-1, NSE and positive numbers of biomarkers. *P < 0.05, **P < 0.001. (TIF 1899 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zhang, L., Liu, D., Li, L. et al. The important role of circulating CYFRA21-1 in metastasis diagnosis and prognostic value compared with carcinoembryonic antigen and neuron-specific enolase in lung cancer patients. BMC Cancer 17, 96 (2017). https://doi.org/10.1186/s12885-017-3070-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-017-3070-6