Abstract
Background
To identify risk factors associated with a composite adverse maternal outcomes in women undergoing intrapartum cesarean birth.
Methods
We used the facility-based, multi-country, cross-sectional WHO Global Survey of Maternal and Perinatal Health (2004–2008) to examine associations between woman-, labor/obstetric-, and facility-level characteristics and a composite adverse maternal outcome of postpartum morbidity and mortality. This analysis was performed among women who underwent intrapartum cesarean birth during the course of labor.
Results
We analyzed outcomes of 29,516 women from low- and middle-income countries who underwent intrapartum cesarean birth between the gestational ages of 24 and 43 weeks, 3.5% (1040) of whom experienced the composite adverse maternal outcome. In adjusted analyses, factors associated with a decreased risk of the adverse maternal outcome associated with intrapartum cesarean birth included having four or more antenatal visits (AOR 0.60; 95% CI: 0.43–0.84; p = 0.003), delivering in a medium- or high-human development index country (vs. low-human development index country: AOR 0.07; 95% CI: 0.01–0.85 and AOR 0.02; 95% CI: 0.001–0.39, respectively; p = 0.03), and malpresentation (vs. cephalic: breech AOR 0.52; CI: 0.31–0.87; p = 0.04). Women who were medically high risk (vs. not medically high risk: AOR 1.81; CI: 1.30–2.51, p < 0.0004), had less education (0–6 years) (vs. 13+ years; AOR 1.64; CI: 1.03–2.63; p = 0.01), were obstetrically high risk (vs. not high risk; AOR 3.67; CI: 2.58–5.23; p < 0.0001), or had a maternal or obstetric indication (vs. elective: AOR 4.74; CI: 2.36–9.50; p < 0.0001) had increased odds of the adverse outcome.
Conclusion
We found reduced adverse maternal outcomes of intrapartum cesarean birth in women with ≥ 4 antenatal visits, those who delivered in a medium or high human development index country, and those with malpresenting fetuses. Maternal adverse outcomes associated with intrapartum cesarean birth were medically and obstetrically high risk women, those with less education, and those with a maternal or obstetric indication for intrapartum cesarean birth.
Similar content being viewed by others
Key message
Certain woman-level, obstetric-level, and available facility-level risk factors are associated with a greater likelihood of adverse maternal outcomes following an intrapartum cesarean birth. The modifiable factors could be targeted for interventions to reduce adverse maternal outcomes of intrapartum cesarean birth.
Background
Cesarean birth rates are increasing gobally [1]. This increase in cesarean birth rates is due, in part, to the performance of medically unnecessary cesareans [2]. Cesarean birth can be a life-saving procedure for mothers and babies, but it can also be associated with maternal morbidity and mortality [3]. Cesarean birth can potentially result in longer hospitalization and neonatal respiratory complications [4]. Compared with cesarean births conducted before the onset of labor, women are at the greatest risk of harm from cesarean birth when it is performed during labor, which is variably described as an unplanned, intrapartum, or emergency cesarean birth [5]. This is often due to lack of availability of anesthetic and surgical workforce and availability of supplies such as oxygen, anesthesia, and bloodbanks [6]. In order to mitigate the risks of adverse outcomes, cesarean birth should be used at the right time, for the right indications, and with appropriate surgical technique [7].
Given that cesarean birth rates are increasing globally, identifying actionable, modifiable risk factors associated with adverse maternal outcomes following intrapartum cesarean birth may help prevent some maternal morbidity and mortality related to this procedure [5]. We conducted a secondary analysis of the WHO Global Survey on Maternal and Perinatal Health dataset in order to compare women from low- and middle-income countries who gave birth by intrapartum cesarean and experienced an adverse maternal outcome, to women who experienced an intrapartum cesarean birth without having an adverse outcome [8]. Our aim was to identify any modifiable risk factors associated with a composite adverse maternal outcome following intrapartum cesarean birth to determine if there are any target areas that might improve pregnancy outcomes in this population.
Methods
Dataset
The methodology of the WHO Global Survey of Maternal and Perinatal Health (WHOGS) has been published [9]. In brief, WHOGS was undertaken in 2004–05 (in 8 Latin American and 7 African countries) and in 2007–08 in 9 Asian countries [10,11,12]. Data were gathered for 2 months in these low- and middle-income countries in institutions with at least 6000 deliveries per year and for 3 months in institutions with fewer than 6000 annual deliveries [9]. Data about the sociodemographic, obstetric, birth, and labor characteristics, and a range of maternal and perinatal outcomes, were captured from all women who gave birth in participating institutions during the data collection period [9]. Data were collected for 290,610 deliveries in 373 facilities in 24 countries [9]. Data were collected prospectively from the time of maternal presentation at the facility until discharge, death or the seventh day postpartum, whichever occurred first [9]. Data collectors reviewed medical records daily and abstracted de-identified data from these records into an individual data form [9]. Additionally, an institutional data form was completed for each participating facility via an interview with the head of the obstetrics/gynaecology department [9]. All countries were included except for Angola, which was dropped due to outlier data related to the ICU admission variable, which has been noted in prior WHOGS analyses [13].
Study overview
This was a secondary analysis of the prospectively collected WHOGS data. Our study population included women who underwent intrapartum cesarean birth after the onset of spontaneous or induced labor between the gestational ages of 24 and 43 weeks. We compared women who experienced a composite adverse maternal outcome to those women who did not experience the composite outcome.
Primary outcome
Our primary outcome of interest was a composite measure of severe maternal morbidity and mortality. A woman was considered to have had this composite outcome associated with cesarean birth if she experienced any one or more of the following: hysterectomy, intensive care unit (ICU) admission greater than or equal to 2 days, or maternal death [14]. It should be noted that an assumption of our analysis was that the ICU admission occurred after birth, but there is no method to verify this in the dataset, which was the methodology used in our major WHOGS analyses.
Analysis
Covariates considered in our analysis were sociodemographic characteristics (education, human development index (2008) of the country where woman gave birth, number of antenatal visits, medical risk level (defined below), age, marital status, body mass index, obstetric risk level (defined below), referral to a higher level of care during the course of labor, gestational age, and birthweight [15]. We also included parity, number of fetuses, fetal presentation, onset of labor, and history of prior cesarean birth [16, 17]. Facility-level covariates considered in the analysis were teaching facility status, total deliveries at facility per year, and location of facility (urban versus rural).
The WHOGS collected the indication for cesarean birth as a checklist of 21 non-mutually exclusive possibilities; more than one indication for cesarean could be assigned to each woman [8, 9]. We considered the indication for cesarean birth in our analysis by dividing the 21 indications into five mutually exclusive groups—women had to have one of the indications in a given group, and none of the indications under the definition of another indication group; these are listed in Table 1.
For this secondary analysis, women were categorized into the “high” maternal medical risk category if the survey reported they had HIV, chronic hypertension, cardiac or renal disease, respiratory disease, diabetes, malaria, anemia, urinary tract infection, genital ulcers, or condyloma. In addition, we defined obstetric risk level as “high” for women who experienced pregnancy-related hypertension, pre-eclampsia or eclampsia, or suspected fetal growth impairment. Though multiple gestation, non-cephalic presenting fetuses, and history of prior cesarean birth are considered high-risk issues, these are considered obstetric variables and are presented separately from those who experienced the aforementioned pregnancy complications that made them “obstetrically high risk” for the purposes of this analysis.
Due to the hierarchical structure of the data, mixed effects logistic regression analyses was performed with a random effect for country and for facility nested within country. Univariate and multivariable analyses were used to assess the association between the adverse maternal composite outcome of cesarean birth and the identified facility- and individual-level covariates. P-values and 95% confidence intervals (CI) were reported, and statistical analyses was conducted using SAS v.9.4 software.
Results
Primary outcome
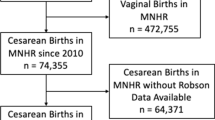
From a total 290,610 women included in the WHOGS, 29,516 (10.2%) of women gave birth by intrapartum cesarean at a gestational age between 24 and 43 weeks and had the composite adverse outcome data available. Women experiencing cesarean birth prior to the onset of labor were not included in the analysis population. The CONSORT diagram in Fig. 1 illustrates the studied cohort. In total, 1040 (3.5%) of these women experienced the maternal adverse composite outcome (Table 2). The remaining 28,476 (96.5%) of the women experienced uncomplicated, intrapartum cesarean births.
Summary of populations
Table 3 summarizes the characteristics of the women in the study population. The majority of women lived in medium human development index countries (74%), attended four or more antenatal visits (72%), were not medically high risk (81%), were between the age of 19 and 34 (81%), had 7–12 years of education (55%), were married or cohabitating (87%), and were of normal (28%) or overweight (39%) body mass index. The majority of women had not had a cesarean (80%), were not obstetrically high-risk (90%), were not referred during the course of labor (74%), had a term birth (91%) of a cephalic fetus (87%), had a baby between 2500 and 3499 g (61%), went into spontaneous labor (86%), were nulliparous (53%), and delivered a singleton (97%) baby. Most women were delivered by an obstetrician (59%) at a teaching facility (82%), and at facilities that had 3500–9999 deliveries in a year (43%). 89% of deliveries were at facilities that were not in an urban setting. The most prevalent indication for cesarean birth was “no other indication” (32%), which was defined as not having another specific indication (Table 1), followed by failure to progress/dystocia (24%), fetal indication (17%), “elective” (11%), multiples or malpresentation (8%), and maternal or obstetric indication (7%).
Univariate analysis (unadjusted odds ratios, UOR)
Odds ratios (ORs) and corresponding 95% confidence intervals (CIs) from the univariate analysis are presented in the first column of Table 3. The composite maternal adverse outcome of intrapartum cesarean birth was less likely to occur in women who delivered in a medium or high human development index country vs. a low human development index country, overall (p = 0.003). It was also less likely to occur in women who had at least four antenatal visits (UOR 0.46 [0.35,0.59], p < 0.0001), in babies with a birthweight of 3500–4499 (vs. 2500–3499; UOR 0.75 [0.59,0.97], p < 0.0001), and in women with a history of prior cesarean birth (vs. no prior cesarean; UOR 0.66 [0.51,0.86], p = 0.002).
Women who were medically high risk (UOR 2.17 [1.70,2.77], p < 0.0001), were less educated (0–6 years versus 13 or more years; UOR 1.82 [1.26,2.63], p < 0.0001), were obstetrically high risk (UOR 4.48 [3.50,5.74], p < 0.0001), were referred in labor (UOR 1.92 [1.47,2.50], p < 0.0001), or were preterm (24–33 weeks UOR 5.16 [3.33,8.00] and 34–36 weeks UOR 2.82 [2.06,3.87], p < 0.0001) had an increased risk of the adverse outcome. Similarly, women with babies less than 2500 g were at increased risk (< 1500 g UOR 7.37 [4.33,12.6] and 1500–2499 g UOR 2.06 [1.52,2.78], p < 0.0001), as were those with multiple gestation (UOR 2.17 [1.44,3.28], p = 0.0002). Finally, compared to the elective category of indications, women with a maternal or obstetric indication (UOR 6.81 [4.25,10.9]) or no other indication (UOR 2.41 [1.56,3.73) were at an increased risk of the composite adverse outcome, p < 0.0001.
Multivariable analysis (adjusted odds ratios, AOR)
Odds ratios (ORs) and corresponding 95% confidence intervals (CIs) from the multivariate analysis are presented in the second column of Table 4. The composite maternal adverse outcome of intrapartum cesarean birth was overall less likely to occur in women who delivered in a medium or high human development index country vs. a low human development index country (AOR 0.07[0.01,0.85] and AOR 0.02[0.001,0.39], respectively; p = 0.03), women having four or more antenatal visits (AOR 0.60; 95% CI: 0.43–0.84; p = 0.003), and women with malpresenting fetuses (vs. cephalic: breech AOR 0.52; CI: 0.31–0.87; p = 0.04).
Women who were medically high risk (vs. not medically high risk: AOR 1.81; CI: 1.30–2.51, p < 0.0004), had less education (0–6 years) (vs. 13+ years; AOR 1.64; CI: 1.03–2.63; p = 0.01), were obstetrically high risk (vs. not high risk; AOR 3.67; CI: 2.58–5.23; p < 0.0001), or had a maternal or obstetric indication or no other indication (vs. elective: AOR 4.74; CI: 2.36–9.50; p < 0.0001) had increased odds of the adverse outcome.
Discussion
In this analysis of 29,516 women who underwent intrapartum cesarean birth in 22 countries in Africa, Asia, and Latin America, factors independently associated with the composite adverse maternal outcome following intrapartum cesarean included women being medically or obstetrically high risk or having a maternal, obstetric, or no other indication for cesarean birth. Factors associated with a reduction in the composite outcome were giving birth in a country of medium or high Human Development Index of the country in which the woman delivered, having had at least four antenatal care visits, and having a breech or other malpresenting fetus compared to cephalic. We hypothesize that our result related to malpresentation represents the fact that most women with non-cephalic fetuses were likely delivered by pre-labor cesarean birth, and only those with very advanced, spontaneous labor delivered vaginally with overall good outcomes.
A potential target for modifying risk associated with intrapartum cesarean birth is attendance at antenatal care. Our analysis suggests that four or more antenatal care visits during pregnancy is associated with 40% fewer adverse outcomes in women who experienced an intrapartum cesarean birth. Though antenatal attendance has previously shown an association with cesarean birth, we could not find other analyses suggesting that increased antenatal care attendance reduces adverse maternal outcomes of intrapartum cesarean birth [18]. This suggests the possibility that this variable is confounded by another variable or may reflect that women with preterm birth attend less antenatal visits. However, researchers in the United States have suggested that improving recovery after cesarean birth does begin in early antenatal care [19]. WHO has recently published recommendations that women have at least eight antenatal contacts during the course of pregnancy to improve outcomes, which might have an impact on this composite outcome, but we have no evidence of this potential effect [20, 21].
Improving maternal outcomes of intrapartum cesarean birth could involve triaging women during antepartum care to assess their need for specialized care as another potential strategy to improve outcomes. Women with obstetric complications of pregnancy (i.e. hypertensive disorders or suspected fetal growth impairment), who were shown to have an increased risk of maternal adverse outcomes, might benefit from additional prenatal management, a more skilled antenatal care provider, or management by a high-risk service in labor [22]. Specialty clinics and risk scoring have been previously explored as methods to meet the needs of subpopulations of women with special antepartum needs [23, 24]. As such, we hypothesize that optimizing management or prevention of these obstetric and medical issues, and recommending specific birth planning that takes current or potential complications into account, may improve maternal outcomes in the event an intrapartum cesarean birth occurs.
Our definition of obstetrically high risk included women with hypertension in pregnancy, pre-eclampsia, eclampsia, or have suspected fetal growth impairment, with other high risk variables (history of cesarean birth, number of gestations, fetal presentation) entered separately into the model. The WHO, in addition to a number of other organizations such as the American College of Obstetricians and Gynecologists, have published guidelines for managing hypertension in pregnancy as hypertensive disorders are a contributor to maternal mortality [25,26,27,28]. Additionally, women referred during the course of labor also had an increased risk of the composite adverse outcome. WHO, in its guidelines on respectful maternity care during labor and childbirth, specifically notes that delivery of high-quality care requires timely and appropriate referral in labor when complications are encountered, through improved infrastructure and established referral pathways [20, 29, 30].
Finally, our analysis found that among women with a maternal or obstetric indication for intrapartum cesarean birth, as compared to cases where the indication was reported as “elective” (see Table 1 for definition), women were more likely to experience the composite adverse outcome. Compared to these cases, women that experience emergency cesarean birth have been shown to have worse maternal and fetal/neonatal outcomes [31, 32]. That being said, cesarean birth should be provided at the right time, for appropriate reasons, and with high-quality technique [7]. It is a major abdominal surgery that can in itself result in adverse outcomes, and can be quite expensive to deliver, so it should only be provided when medically necessary [1,2,3, 33, 34]. Indication for cesarean birth is a modifiable risk factor in that it can be modified to promote best obstetric practices. Guidelines for prevention of primary cesarean birth have been produced to assist in the decision-making process to proceed to cesarean birth [35, 36].
The limitations of this study include the fact that the data were collected 10 years ago and that unmeasured facility, sociodemographic, or obstetric variables may confound the results. Due to the large amount of missingness for some maternal outcome variables (intrapartum and postpartum blood transfusion, internal iliac artery ligation, and postpartum urogenital fistula) they were not included in the definition of the composite outcome, although we ideally would have wanted to include them. Additionally, 16% of BMI data was missing, and while the weight parameter was meant to reflect the most recently recorded weight of a woman, the time of collection could vary. We also note that the criteria for definition of the various morbidities was according to local practices and the methodology of the survey did not impose any specific definition, which makes interpretation of some the results more challenging. For example, the collecting agency did not specify criteria for ICU admittance. We noted in our initial analysis that the component of the composite outcome that accounted for the most adverse outcomes was ICU admission. This was a subjective parameter in the data set as each hospital had its own admittance criteria. We ran a histogram of days in the ICU and found that most women were only admitted to the ICU for 1 day (data not shown); we hypothesized this was the result of it being common practice in some settings where the only hospital location capable of monitoring a post-operative patient is the ICU. In order to try to refine the definition to include only those women who had severe morbidity and were not just in the ICU for monitoring, we adjusted the definition to stays of greater than or equal to 2 days.
A previous paper observed the association of cesarean birth, considering indication, with maternal and perinatal outcomes in Asian populations from this dataset [10]. Our analysis adds to this prior analysis by evaluating the association of additional, potentially modifiable risk factors with a composite adverse maternal outcome following intrapartum cesarean birth in the entire dataset. Other strengths of this analysis are the use of a large data set, the collection of multiple variables potentially associated with the outcome, the fact that the survey was designed to assess method of birth, and that the multi-country data were collected using a standard approach/protocol/measurement tool and abstracted from routine medical records [9].
Conclusion
We found reduced adverse maternal outcomes following intrapartum cesarean birth associated with women giving birth in medium or high human development index countries and those who attended ≥ 4 antenatal visits. Maternal adverse outcomes of intrapartum cesarean birth were increased in medically and obstetrically high risk women and those with a maternal or obstetric indication for cesarean birth.
Availability of data and materials
Requests for data should be made to the WHO Human Reproductiuon Program for consideration.
Abbreviations
- WHO:
-
World Health Organization
- WHOGS:
-
WHO Global Survey of Maternal and Perinatal Health
- UOR:
-
Unadjusted odds ratio
- AOR:
-
Adjusted odds ratios
References
Betran AP, et al. The increasing trend in caesarean section rates: global, regional and national estimates: 1990-2014. PLoS One. 2016;11(2):e0148343.
Betran AP, et al. Interventions to reduce unnecessary caesarean sections in healthy women and babies. Lancet. 2018;392(10155):1358–68.
Betran AP, et al. WHO statement on caesarean section rates. BJOG. 2016;123(5):667–70.
Mariani GL, Vain NE. The rising incidence and impact of non-medically indicated pre-labour cesarean section in Latin America. Semin Fetal Neonatal Med. 2019;24(1):11–7.
Sobhy S, et al. Maternal and perinatal mortality and complications associated with caesarean section in low-income and middle-income countries: a systematic review and meta-analysis. Lancet. 2019;393(10184):1973–82.
Ologunde R, et al. Assessment of cesarean delivery availability in 26 low-and middle-income countries: a cross-sectional study. Am J Obstet Gynecol. 2014;211(5):504.e1–504.e12.
Gibson K, Bailit JL. Cesarean delivery as a marker for obstetric quality. Clin Obstet Gynecol. 2015;58(2):211–6.
World Health Organization. Global survey on maternal and perinatal health. 2019. [June 5, 2019]. Available from: https://www.who.int/reproductivehealth/topics/maternal_perinatal/globalsurvey/en/.
Shah A, et al. Methodological considerations in implementing the WHO global survey for monitoring maternal and perinatal health. Bull World Health Organ. 2008;86(2):126–31.
Lumbiganon P, et al. Method of delivery and pregnancy outcomes in Asia: the WHO global survey on maternal and perinatal health 2007–08. Lancet. 2010;375(9713):490–9.
Shah A, et al. Cesarean delivery outcomes from the WHO global survey on maternal and perinatal health in Africa. Int J Gynecol Obstet. 2009;107(3):191–7.
Villar J, et al. Caesarean delivery rates and pregnancy outcomes: the 2005 WHO global survey on maternal and perinatal health in Latin America. Lancet. 2006;367(9525):1819–29.
Vogel JP, et al. Use of the Robson classification to assess caesarean section trends in 21 countries: a secondary analysis of two WHO multicountry surveys. Lancet Glob Health. 2015;3(5):e260–70.
Maswime S, Buchmann E. A systematic review of maternal near miss and mortality due to postpartum hemorrhage. Int J Gynecol Obstet. 2017;137(1):1–7.
Human Development Index. Human Development Index. 2008. [July 17, 2019]. Available from: http://hdr.undp.org/en/data.
Robson MS. Classification of caesarean sections. Fetal Matern Med Rev. 2001;12(1):23–39.
World Health Organization. Robson classification: implementation manual. 2017. [June 5, 2019]. Available from: https://www.who.int/reproductivehealth/publications/maternal_perinatal_health/robson-classification/en/.
Nimi T, et al. Prenatal care and pregnancy outcomes: a cross-sectional study in Luanda, Angola. Int J Gynecol Obstet. 2016;135(S1):S72–8.
Wilson RD, et al. Guidelines for antenatal and preoperative care in cesarean delivery: enhanced recovery after surgery society recommendations (part 1). Am J Obstet Gynecol. 2018;219(6):523.e1–523.e15.
World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience; 2016. p. 1–172.
Vogel JP, et al. Antenatal care packages with reduced visits and perinatal mortality: a secondary analysis of the WHO antenatal care trial. Reprod Health. 2013;10(1):19.
Yeoh PL, Hornetz K, Dahlui M. Antenatal care utilisation and content between low-risk and high-risk pregnant women. PLoS One. 2016;11(3):e0152167.
Malouf R, Redshaw M. Specialist antenatal clinics for women at high risk of preterm birth: a systematic review of qualitative and quantitative research. BMC Pregnancy Childbirth. 2017;17(1):51.
Humphrey MD, Foxcroft KF, Callaway LK. Obstetric risk score - revalidated for triaging high-risk pregnancies in rural areas. Aust N Z J Obstet Gynaecol. 2017;57(1):63–7.
Say L, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2(6):e323–33.
Abalos E, et al. Pre-eclampsia, eclampsia and adverse maternal and perinatal outcomes: a secondary analysis of the World Health Organization multicountry survey on maternal and newborn health. BJOG. 2014;121(Suppl 1):14–24.
World Health Organization. WHO recommendations for prevention and treatment of pre-eclampsia and eclampsia. Chicago: World Health Organization; 2011.
American College of Obstetricians and Gynecologists. Gestational hypertension and preeclampsia: ACOG Practice Bulletin, number 222. Obstet Gynecol. 2020;135(6):e237–e260.
World Health Organization. WHO recommendations: intrapartum care for a positive childbirth experience; 2018. p. 1–210.
World Health Organization. WHO safe childbirth checklist implementation guide: improving the quality of facility-based delivery for mothers and newborns. 2015 [June 11, 2019]. Available from: https://apps.who.int/iris/bitstream/handle/10665/199177/9789241549455_eng.pdf?sequence=1.
Suwal A, Shrivastava VR, Giri A. Maternal and fetal outcome in elective versus emergency cesarean section. JNMA J Nepal Med Assoc. 2013;52(192):563–6.
Benzouina S, et al. Fetal outcome in emergency versus elective cesarean sections at Souissi Maternity Hospital, Rabat, Morocco. Pan Afr Med J. 2016;23:197.
Betran AP. Reducing unnecessary cesarean section: a generic formative phase protocol for implementation preparation: World Health Organization; 2019. p. 1–148.
Betran AP, et al. What is the optimal rate of caesarean section at population level? A systematic review of ecologic studies. Reprod Health. 2015;12:57.
ACOG, Safe prevention of the primary cesarean delivery. 2016.
Smith H, Peterson N, Lagrew D, Main E. Toolkit to support vaginal birth and reduce primary cesareans: a quality improvement toolkit. Stanford: California Maternal Quality Care Collaborative; 2016.
Acknowledgements
We want to thank all the women and men involved in collection of the data analyzed in this work and all the women who participated in the study—their health, well-being, and successful pregnancy outcomes are the motivation for performing this work.
Funding
Our study is a secondary analysis of the WHO Global Survey on Maternal and Perinatal Health which was financially supported by the UNDP/UNFPA/UNICEF/ WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction; WHO; the Governments of China, India, and Japan; and the United States Agency for International Development (USAID). These funding bodies had no role in the design, analysis, or interpretation of this secondary analysis of previously collected data.
This article represents the views of the named authors only, and does not represent the views of the World Health Organization. This secondary analysis of the survey was supported by the Eunice Kennedy Shriver National Institutes of Child Health and Human Development Women’s Reproductive Health Research K12 award (5K12HD001271) and the Doris Duke Charitable Foundation. These funding bodies (NICHD and DDCF) had no role in the design, analysis, or interpretation of this secondary analysis of previously collected data.
Author information
Authors and Affiliations
Contributions
MSH conceived of the analytic plan with feedback and input from APB, JPV, RLG, and AMG. MSH and KS performed the analysis with feedback and oversight from APB, JPV, and RLG. MSH and KS wrote the manuscript with input from all authors. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This de-identified data analysis was reviewed and approved by the Colorado Multiple Institutional Review Board, 18–0875. For this original WHOGS data collection each institution submitted the ethical clearance approval before commencing the project. Ethical clearance was provided by the institutional committees of the participating facilities, where available, or by the national review committees (available at: http://www.who.int/making_pregnancy_safer/health_systems/global_survey/en/index.html). In addition, ethical clearance was obtained from WHO’s Scientific and Ethical Review Group and Ethics Review Committee. Individual informed consent was not obtained, and the ethics committee waived the need for individual consent, as this was a cluster-level study, where data were extracted from medical records without any subject identification. However, key subject information (name, study number, birth date and delivery date) was recorded in the logbook at the institution level by the data collector to assist with follow-up if required.
Consent for publication
Not Applicable.
Competing interests
The authors have no relationships to disclose that may be deemed to influence the objectivity of this paper and its review. The authors report no commercial associations, either directly or through immediate family, in areas such as expert testimony, consulting, honoraria, stock holdings, equity interest, ownership, patent-licensing situations or employment that might pose a conflict of interest to this analysis. Additionally, the authors have no conflicts such as personal relationships or academic competition to disclose. The findings presented in this paper represent the views of the named authors only, and not the views of their institutions or organizations. Regarding data, supporting data cannot currently be accessed.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Harrison, M.S., Betrán, A.P., Suresh, K. et al. Risk factors associated with adverse maternal outcomes following intrapartum cesarean birth: a secondary analysis of the WHO global survey on maternal and perinatal health, 2004–2008. BMC Pregnancy Childbirth 20, 687 (2020). https://doi.org/10.1186/s12884-020-03390-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-020-03390-0