Abstract
Background
Anomalies of pyramidal tract decussation are rare phenomena that can be caused by ectodermal dysplasia. Herein, we describe a patient with ichthyosis who exhibited ipsilateral hemiparesis after stroke and whose neuroimaging results showed evidence of motor control being provided by the ipsilateral motor cortex.
Case presentation
A 24-year-old right-handed man presented with skin abnormalities, sudden-onset left hemiparesis, and dysarthria. He exhibited a mild-to-moderate left-sided weakness (grade 4 on the Medical Research Council scale). Magnetic resonance imaging revealed an acute infarct in the left corona radiata. Diffusion tensor imaging revealed uncrossed corticospinal tracts. Next-generation sequencing identified heterozygous FLG mutations. The patient was diagnosed with cerebral infarction and ichthyosis vulgaris and was treated with aspirin (100 mg/d). His symptoms gradually dissipated.
Conclusions
This case suggests that pyramidal decussation anomalies can be associated with ichthyosis. Patients with ichthyosis should therefore be evaluated for nerve involvement.
Similar content being viewed by others
Background
Supratentorial stroke is widely known to cause neurological impairment on the contralateral side of the body. Previous neuroanatomic studies have shown that the primary motor cortex predominantly controls the contralateral half of the body [1]. Corticospinal tract decussation anomalies are mostly nonspecific and coincidental. Since the first report [2], such anomalies have been described in patients with posterior fossa malformations and extensive brainstem malformations [3]. Furthermore, a few reports have described ipsilateral hemiparesis in patients with agenesis of the corpus callosum and scoliosis [4, 5], and such reports show that pyramidal tract abnormalities can arise in patients with developmental disorders. Herein, we describe a patient with ichthyosis who exhibited ipsilateral hemiparesis after stroke and whose neuroimaging results showed evidence of motor control being provided by the ipsilateral motor cortex.
Case presentation
A 24-year-old man presented with sudden-onset mild left-sided hemiparesis that had manifested 2 days earlier. He had no history of smoking, or excessive alcohol consumption. A medical examination showed that he had dry and scaly skin (Fig. 1). He claimed to have experienced his skin disorder for 20 years. On neurological examination, he was conscious and alert. No other focal neurologic deficits were noted except mild left-sided hemiparesis.
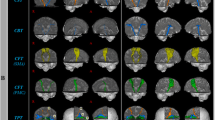
Initial head CT demonstrated no acute infarction. The following day, brain magnetic resonance imaging (MRI) (Siemens, Germany) with diffusion-weighted sequences revealed punctate areas of restricted diffusion in the left corona radiata that represented small acute infarct (Fig. 2a). Magnetic resonance angiography revealed no significant flow-limiting stenosis. Because the MRI-detected lesions were ipsilateral to the paralyzed limb, the patient underwent diffusion tensor imaging (DTI) (Siemens Magnetom trioatim 3.0 T, Siemens Leonardo) tractography, which revealed uncrossed corticospinal tracts (Fig. 2b). The level of D-dimer was within the normal range in our patient who without history of hypertensive disease, in addition, no abnormalities were found in carotid ultrasound, cervical MRI, echocardiography, foaming test and microembolism monitoring, the probabilities of arterial dissection or patent foramen ovale were reduced.
Cerebrovascular risk factors such as serum lipid, uric acid, homocystein, high-sensitivity C-reactive protein, B12 vitamin, folate, fasting blood glucose were all within the normal range and the patient has no history of hypertension, diabetes mellitus, smoking, and alcohol consumption. Body mass index (BMI), routine blood test, coagulation routine, renal function and liver function, erythrocyte sedimentation rates (ESR), HIV serology, syphilis serology, serum lactate, anti-nuclear antibody were all normal or negative. An electrocardiogram and a transthoracic echocardiogram revealed no sources of cardiac embolism. Besides, the patient’s other MRI sequences were negative, so we could exclude cerebral small vessel disease and microbleeds. Noteworthy, his skin was abnormal for about 20 years. We performed a genetic test on the patient. However, next-generation sequencing of a DNA sample identified two known heterozygous FLG nonsense mutations: (c.3905C > A, p.Ser1302Ter)(which was inherited from his father) and (c.5368C > T, p.Gln1790Ter) (which was inherited from his mother) [6, 7]. The two mutations have an effect on the protein functions.
Based on these genetic findings and the patient’s 20-year history of skin complaints, the patient was diagnosed with ichthyosis vulgaris and cerebral infarction. His left-side hemiparesis gradually dissipated after symptomatic treatment. Aspirin therapy played a crucial role in the secondary prevention of ischemic stroke. After discharge, the patient continued to take aspirin with daily dose of 100 mg.
Discussion
Ichthyosis is a group of disorders resulting from variants in more than 50 genes, and it is characterized by thickening and splitting of the skin [8]. Roy et al. [9] reported that spasticity, epilepsy, and intellectual disability are the primary neurological findings. Our case represents the first report of cerebral infarctions as neurological comorbidities in a patient with ichthyosis.
We diagnosed our patient with ichthyosis vulgaris, which typically results from heterozygous or compound heterozygous FLG mutations. However, all forms of ichthyosis have been associated with protein and lipid abnormalities [8]. Our young patient had almost no risk factors for cerebrovascular disease, indicating that ichthyosis might be associated with the development of infarction. Interestingly, our patient exhibited brain lesions that were ipsilateral to his paralyzed limb.
Previous reports suggested anomalies of the dorsal column medial lemniscus pathway associated with uncrossed pyramidal tracts and abnormalities of bimanual tasks in pyramidal tract crossing anomalies [10,11,12]. After we had performed a careful physical examination and asked history of disease entirely, not found any sensory abnormality, synkinetic contralateral movements or mirror movement in this patient.
Donkelaar et al. [3] described the development and potential malformations of the human pyramidal tract and noted that certain malformations may lead to pyramidal decussation anomalies. Decussation anomalies of the corticospinal tracts can be found in association with other cerebral anomalies, such as congenital scoliosis, corpus callosum agenesis, occipital encephaloceles, posterior fossa malformations, Dandy-Walker malformations, Joubert syndrome, and extensive brainstem malformations [3].
In terms of embryogenesis, the skin and nervous system are homologous to the ectoderm. Congenital ectodermal dysplasia causes simultaneous neurological and cutaneous lesions, resulting in various clinically complex hereditary neurocutaneous syndromes. Sprecher et al. [13] described a novel neurocutaneous disease called CEDNIK syndrome that is characterized by cerebral dysgenesis, neuropathy, ichthyosis, and keratoderma. We therefore speculate that our patient’s pyramidal decussation anomalies may be caused by the same FLG mutations that cause his ichthyosis.
Conclusions
In conclusion, we identified uncrossed pyramidal tracts in a patient with clinically and genetically confirmed ichthyosis and there might be a pathophysiological association, becoming clinically relevant in certain scenarios, such as stroke.
Abbreviations
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- DTI:
-
Diffusion tensor imaging
References
Weiller C, Chollet F, Friston KJ, et al. Functional reorganization of the brain in recovery from striatocapsular infarction in man. Ann Neurol. 1992;31:463–72. https://doi.org/10.1002/ana.410310502.
Hosokawa S, Tsuji S, Uozumi T, et al. Ipsilateral hemiplegia caused by right internal capsule and thalamic hemorrhage: demonstration of predominant ipsilateral innervation of motor and sensory systems by MRI, MEP, and SEP. Neurology. 1996;46:1146–9. https://doi.org/10.1212/wnl.46.4.1146.
ten Donkelaar HJ, Lammens M, Wesseling P, et al. Development and malformations of the human pyramidal tract. J Neurol. 2004;251:1429–42. 2005/01/13. https://doi.org/10.1007/s00415-004-0653-3.
Ng AS, Sitoh YY, Zhao Y, et al. Ipsilateral stroke in a patient with horizontal gaze palsy with progressive scoliosis and a subcortical infarct. Stroke. 2011;42:e1–3. 2010/11/23. https://doi.org/10.1161/STROKEAHA.110.591271.
Kang K, Choi N. Ipsilateral hemiparesis and spontaneous horizontal nystagmus caused by middle cerebral artery territory infarct in a patient with agenesis of the corpus callosum. Neurol Sci. 2012;33:1165–8. 2011/12/14. https://doi.org/10.1007/s10072-011-0871-2.
Zhang H, Guo Y, Wang W, et al. Mutations in the filaggrin gene in Han Chinese patients with atopic dermatitis. Allergy. 2011;66:420–7. 2010/11/03. https://doi.org/10.1111/j.1398-9995.2010.02493.x.
Chen H, Common JE, Haines RL, et al. Wide spectrum of filaggrin-null mutations in atopic dermatitis highlights differences between Singaporean Chinese and European populations. Br J Dermatol. 2011;165:106–14. 2011/03/25. https://doi.org/10.1111/j.1365-2133.2011.10331.x.
Paller AS. Profiling Immune Expression to Consider Repurposing Therapeutics for the Ichthyoses. J Invest Dermatol. 2019;139:535–40. 2019/01/24. https://doi.org/10.1016/j.jid.2018.08.027.
Roy U, Das U, Pandit A, et al. Sjogren-Larsson syndrome: a rare disease of the skin and central nervous system. BMJ Case Rep 2016; 2016: 10 1136/bcr-2016-215110. 2016/04/21. DOI: https://doi.org/10.1136/bcr-2016-215110.
Cincotta M, Borgheresi A, Liotta P, et al. Reorganization of the motor cortex in a patient with congenital hemiparesis and mirror movements. Neurology. 2000;55:129. https://doi.org/10.1212/WNL.55.1.129.
Terakawa H, Abe K, Nakamura M, et al. Ipsilateral hemiparesis after putaminal hemorrhage due to uncrossed pyramidal tract. Neurology. 2000;54:1801–5. https://doi.org/10.1212/wnl.54.9.1801.
Ueki Y, Mima T, Oga T, et al. Dominance of ipsilateral corticospinal pathway in congenital mirror movements. J Neurol Neurosurg Psychiatry. 2005;76:276–9. 2005/01/18. https://doi.org/10.1136/jnnp.2004.040949.
Sprecher E, Ishida-Yamamoto A, Mizrahi-Koren M, et al. A mutation in SNAP29, coding for a SNARE protein involved in intracellular trafficking, causes a novel neurocutaneous syndrome characterized by cerebral dysgenesis, neuropathy, ichthyosis, and palmoplantar keratoderma. Am J Hum Genet. 2005;77:242–51. https://doi.org/10.1086/432556.
Acknowledgments
We are grateful to the patient who was willing to share his medical data.
Availability of data and material
Not applicable.
Funding
This work was supported by the National Natural Science Foundation of China (grant number 81974191). The funding body played no role in the design of the study, in writing the manuscript, nor in the collection, analysis, or interpretation of the data.
Author information
Authors and Affiliations
Contributions
HJ-Y: drafting the manuscript; accepts responsibility for conduct of research and final approval. HW-Z: analysis or interpretation of data, accepts responsibility for conduct of research and final approval, acquisition of data, study supervision. J-M: critically revised and gave final approval for publication of the paper. All author have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, H., Zhou, H. & Miao, J. Uncrossed corticospinal tracts in a patient with ichthyosis and hemiparesis: a case report. BMC Neurol 20, 120 (2020). https://doi.org/10.1186/s12883-020-01698-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-020-01698-0