Abstract
Background
To investigate predictors of postoperative acute intracranial hemorrhage (AIH) and recurrence of chronic subdural hematoma (CSDH) after burr hole drainage.
Methods
A multicenter retrospective study of patients who underwent burr hole drainage for CSDH between January 2013 and March 2019.
Results
A total of 448 CSDH patients were enrolled in the study. CSDH recurrence occurred in 60 patients, with a recurrence rate of 13.4%. The mean time interval between initial burr hole drainage and recurrence was 40.8 ± 28.3 days. Postoperative AIH developed in 23 patients, with an incidence of 5.1%. The mean time interval between initial burr hole drainage and postoperative AIH was 4.7 ± 2.9 days. Bilateral hematoma, hyperdense hematoma and anticoagulant drug use were independent predictors of recurrence in the multiple logistic regression analyses. Preoperative headache was an independent risk factor of postoperative AIH in the multiple logistic regression analyses, however, intraoperative irrigation reduced the incidence of postoperative AIH.
Conclusions
This study found that bilateral hematoma, hyperdense hematoma and anticoagulant drug use were independently associated with CSDH recurrence. Clinical presentation of headache was the strongest predictor of postoperative AIH, and intraoperative irrigation decreased the incidence of postoperative AIH.
Similar content being viewed by others
Introduction
Chronic subdural hematoma (CSDH) is one of the most common types of intracranial hemorrhage; however, its pathogenic mechanism remains unclear. The incidence of CSDH is ~ 3.4–5/100000 per year in the general population and 60–80/100000 per year in those aged ≥65 [1,2,3,4,5]. The treatment is often surgical evacuation, using techniques such as twist-drill craniotomy and burr hole drainage (BHD) or craniotomy. BHD is the most widely used technique, and has a satisfactory outcome, but has a CSDH recurrence rate of 4–38% [6,7,8,9,10,11,12]. Several studies have revealed that predictors of CSDH recurrence following surgical evacuation include age, sex, antiplatelet or anticoagulation therapy, Glasgow Coma Scale (GCS), diabetes mellitus, hypertension, bilateral hematoma, preoperative hematoma size, midline shift, hematoma density, intraoperative irrigation, type of surgery and postoperative air collection, however, these results are inconsistent [7, 13,14,15,16,17,18,19]. The more controversial risk factors include surgery type and intraoperative irrigation [9, 10, 20,21,22]. Previous reports have shown a CSDH mortality rate of 1.8–32% [6, 23].
Surgical complications, such as irritability, wound infection and acute intracranial hemorrhage (AIH), occur at a rate of 0–38% [24,25,26]. AIH, in particular, can cause severe neurological dysfunction, leading to a poor prognosis. However, the mechanism is still unclear and there is limited information on risk factors associated with AIH following surgery for CSDH. Some previous studies have evaluated recurrence risk following CSDH surgery using only a single or few predictors, however, the majority of these were single-center retrospective studies and lacked interaction between other variables and confounding factors. It is, therefore, important to identify the clinical and perioperative risk factors associated with AIH and CSDH recurrence following BHD surgery. In this multi-center retrospective study we evaluated the clinical factors associated with postoperative AIH and CSDH recurrence, to determine an optimal perioperative management strategy for BHD with or without irrigation in CSDH patients.
Methods
We retrospectively analyzed the medical records of all patients diagnosed with CSDH at the Department of Neurosurgery, the First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, China between September 2015 and March 2019 (n = 315), and the Department of Neurosurgery of Shanghai Tenth People’s Hospital, Shanghai, China between January 2013 and May 2016 (n = 133). The patients were diagnosed by computed tomography (CT) or magnetic resonance imaging (MRI).
Inclusion and exclusion criteria
The inclusion criteria were as follows: all patients were diagnosed with CSDH by CT or MRI; and initially underwent BHD with or without irrigation at one of the two institutions. Exclusion criteria included: CSDH that was treated conservatively or by surgical methods other than BHD (such twist-drill craniotomy and formal craniotomy with excision of subdural membrane); any other intracranial pathologies or intracranial surgery, such as ventriculoperitoneal shunt, epidural hematoma, parenchymal hemorrhage, intraventricular hemorrhage or ischemic insult; and recurrent CSDH.
Definitions
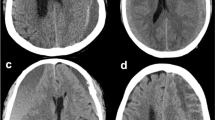
In this study, we defined CSDH as subdural hematoma that could be treated with BHD. We defined postoperative recurrence of CSDH as a subsequent radiographic discharge following the primary treatment, with re-bleeding and/or increased size of the subdural hematomas on the operated side, with or without any clinical presentation. AIH was identified as a hyperdense lesion in the ventricle, brain parenchyma, subarachnoid, subdural space or epidural space, visible on CT scan during hospitalization, and accompanied by neurological deterioration. Chronic intracranial hemorrhage (CIH) in this study refers to cerebral hemorrhage other than recurrent CSDH or AIH.
The hematoma was classified as hypodense [< 30 Hounsfield units (HU)], isodense (30–60 HU), hyperdense (> 60 HU), or mixed density based on the density difference of the hematoma and the brain parenchyma. Patients with bilateral CSDH of different types were attributed according to which reflected the greater bleeding tendency.
Surgical evacuation of CSDH was carried out when the following indications were observed:
-
1.
Unilateral or bilateral CSDH with maximum thickness > 10 mm and/or midline shift > 7 mm;
-
2.
CSDH of any thickness causing mass effect, midline shift, or neurological signs and symptoms, such as focal deficit, and mental status changes;
-
3.
Progressive increase in size of CSDH as observed through a series of CT or MRI scans.
In bilateral CSDH, the decision to evacuate one or both sides was generally made based on hematoma size and neurological symptoms. (i) Unilateral evacuation of bilateral CSDH: when the maximum diameter of the CSDH on the operation side was > 10 mm, when the contralateral hematoma was < 10 mm thick, and when the laterality of neurological symptoms could only be attributed to the thicker hematoma. (ii) Bilateral evacuation of bilateral CSDH: both sides received the same treatment in a single operation.
Surgical procedures and general management
In all cases, a single burr hole was made under anesthesia. Local or general anesthetic was selected depending on the patient’s general status and ability to co-operate. A 4–5 cm vertical skin incision was made at the superior temporal line near the coronal suture or at the point of maximum thickness of the CSDH. A 1.5–2 cm craniotomy was performed. After opening the dura and outer membrane of the hematoma, a soft silicon tube was inserted into the subdural space through the burr hole overlying the large part of the subdural cavity, and tunneled for a minimum of 5 cm away from the scalp incision. Irrigation was not carried out in all surgeries. If carried out, irrigation was with 0.9% normal saline via the tube, until the output was clear. The drain was connected to a soft collection bag and the drainage tube was removed when there was no more drainage fluid. The patient stayed in bed until the drain was removed. If CT scan showed that subdural collections remained in the hematoma cavity after the operation, the patient was treated with urokinase, according to the surgeon’s preference. CT scanning indicated if the affected brain region showed sufficient re-expansion or when the amount decreased to < 50 ml per day.
All patients had their anticoagulant or antiplatelet status optimized prior to surgery, ensuring a preoperative international normalized ratio (INR) between 0.8 and 1.2. It was managed in various ways depending on the type of anticoagulant treatment. Agents used to reverse anticoagulant or antiplatelet medications were vitamin K1, thrombocytes, blood plasma, tranexamic acid, prothrombin complex concentrate, and desmopressin analogs. Antiplatelet or anticoagulant agents were usually re-started 1 month from the day of surgery.
Following CSDH diagnosis, some patients were given atorvastatin (20 mg per night) prior to the operation. The decision to give the patient preoperative atorvastatin was made by the neurosurgeon. In general, atorvastatin was discontinued for at least 1 month after surgery or based on follow-up imaging. All patients were followed-up for at least 12 months.
Data collection
Demographic, clinical and radiographic data were collected using a standardized case report form and the information was added to a database. The following data were included: gender, age, history of anticoagulant or antiplatelet, head trauma event, GCS score on admission, medical history (e.g., hypertension, diabetes), preoperative main clinical symptoms (e.g., headache, dizziness), operation side (unilateral, unilateral evacuation of bilateral CSDH, bilateral evacuation of bilateral CSDH), hematoma density characteristics on CT (hyperdense, hypodense, mixed density, isodense), hematoma maximal thickness (preoperative hematoma thickness on the axial cut that showed the maximal diameter), midline shift, anesthesia method, intraoperative irrigation (non-irrigation versus irrigation), duration of drainage (days), urokinase injection after operation, complications (including acute intracranial bleeding, fever > 38 °C, seizure, irritability, poor wound healing and intracranial infection), time interval between initial operation and recurrence (days), time interval between initial operation and bleeding (days), and hospitalization time (days). All CT interpretations and measurements were made by a neurosurgeon and recorded after corroborating with the neuroradiologist’s report.
Statistical analyses
SPSS software (version 16.0) was used for the statistical analysis.
Continuous data are expressed as the mean ± standard deviation (SD) and categorical data are expressed as the median value (IQR). Univariable (Student t-test and the Mann–Whitney U-test), bivariable (Chi-square) and multivariable (multiple logistic regression) analyses were performed to determine which, if any, of the studied variables were associated risk factors of CSDH recurrence and AIH. The variables with P < 0.1 in the univariate analysis were included in the multivariate model. Statistical significance was defined as P-value < 0.05.
Results
Baseline clinical characteristics of patients
A total of 448 patients (354 males, 94 females) were included in the analysis. The mean age was 68.1 ± 12.4 years (range: 14–98 years). CSDH recurrence occurred in 60 (13.4%) patients, including 26 with unilateral BDH evacuation, 11 with unilateral evacuation of bilateral CSDH, and 23 with bilateral evacuation of bilateral CSDH. Complications occurred in 122 patients (27.2%), including 23 (5.1%) with AIH (16 patients with unilateral evacuation, five with unilateral evacuation of bilateral CSDH, and two with bilateral evacuation of bilateral CSDH). One patient died (mortality rate = 0.2%). The mean duration of hospitalization time was 14.0 ± 5.5 days (range: 3–42 days). Patient information is provided in Table 1.
Analysis of patients with recurrence
Sixty patients (53 males, seven females) experienced CSDH recurrence following the initial BHD. The mean age was 69.6 ± 10.8 years (range: 31–88 years). The mean time interval between initial BHD and recurrence was 40.8 ± 28.3 days (range: 12–180 days).
Univariate analysis (Table 2) showed that risk factors including anticoagulant drugs (P = 0.038), density of hematoma (P = 0.009), operation side (P < 0.001), and atorvastatin administration (P = 0.021) were significantly related to CSDH recurrence. Unilateral or bilateral evacuation of bilateral CSDH were not significantly correlated with CSDH recurrence following BHD (2.5% versus 5.1%, P = 0.707). Although there was no significant correlation between gender and recurrence (P < 0.1), it was included in the multivariate analysis according to our multivariate inclusion analysis criteria. Other variables that were not significantly correlated with CSDH recurrence are shown in Table 2.
In the multivariate logistic regression model, bilateral hematoma [Odds ratio (OR), 2.563; 95% confidence interval (CI), 1.439–4.563; P = 0.001], mixed density (OR, 0.433; 95%CI, 0.229–0.818; P = 0.010, hyperdense as reference) and anticoagulant drugs (OR, 4.309; 95%CI, 1.244–14.923; P = 0.021) were significantly associated with CSDH recurrence. Other variables not significantly associated with CSDH recurrence are detailed in Table 3.
Analysis of patients with acute intracranial hemorrhage
Twenty-three patients (15 males, eight females) experienced postoperative AIH. The mean age was 68.5 ± 11.5 years (range: 42–87 years). The mean time interval between initial BHD and postoperative AIH was 4.7 ± 2.9 days (range: 1–10 days).
Univariate analysis indicated that preoperative headache (P = 0.046), preoperative hematoma thickness (P = 0.043) and intraoperative irrigation (P = 0.020) were significantly related to postoperative AIH (Table 4). Operation side (P = 0.683) was not significantly related to postoperative AIH, and there was no significant difference in the incidence of postoperative AIH between unilateral or bilateral evacuation of bilateral CSDH (1.1% versus 0.4%, P = 0.052). Other variables with P > 0.1 in the univariate analysis are shown in Table 4.
Multivariate analysis showed that preoperative headache (OR, 3.053; 95%CI, 1.181–7.890; P = 0.021) and intraoperative irrigation (OR, 0.289; 95%CI, 0.114–0.735; P = 0.009) were significantly associated with postoperative AIH. Other variables not significantly associated with postoperative AIH or CSDH recurrence are shown in Table 5.
Discussion
CSDH is one of the most commonly treated neurosurgical disorders and BHD is a universal surgical treatment [11, 18, 27]. The rate of CSDH recurrence following BHD is 4–38% and the complications rate is 0–38% [6,7,8,9,10,11,12, 24, 26]. In this study, we found the CSDH recurrence rate after BDH was 13.4% and the complication rate was 27.2%. Of the 122 patients with complications, 23 had postoperative AIH (5.1% incidence). Pang et al. similarly reported an incidence of postoperative AIH of 4.57% [25]. According to the literature, the mortality rate due to CSDH is 1.8–32%, however, in this study, only one patient died of respiratory failure, giving a lower mortality rate of 0.2% [6, 23]. Comparing our results with previous studies, our definition of CSDH, postoperative recurrence of CSDH and postoperative AIH are in accordance with medical norms and logic.
CSDHs are usually unilateral, but do present as bilateral in ~ 9.2–34.9% of cases [5, 28,29,30]. However, not all patients with bilateral CSDH warrant evacuation of both sides at initial presentation. The major determinants of unilateral or bilateral evacuation are preoperative maximal thickness, the degree of midline shift, and lateralized clinical symptoms, followed by surgical treatment of only the largest or the symptomatic hematoma, leaving the other hematoma non-operated [31]. In our study, 154 patients (34.4%) had bilateral CSDH. Fifty-four (12.1%) had unilateral evacuation and 100 (22.3%) were evacuated bilaterally. Previous studies have shown that simultaneous bilateral decompression in bilateral CSDH reduces complications and the rate of CSDH recurrence, however, others have not corroborated this result [31,32,33]. In our study, there was no significant difference between the rate of CSDH recurrence and incidence of AIH following unilateral or bilateral evacuation in bilateral CSDH.
The recurrence rate in unilateral CSDH is lower than that of bilateral CSDH, making bilateral hematoma a risk factor for CSDH recurrence [16, 19]. This could be due to poor brain re-expansion in bilateral CSDH compared to unilateral CSDH, which may result in a brain parenchymal shift, tearing of the blood vessels, postoperative pneumocephalus and cerebrospinal fluid accumulation in the hematoma cavity, leading to a higher recurrence rate [19, 34, 35]. Another theory is that patients with bilateral CSDH tend to have a history of brain atrophy, which leads to poor re-expansion, resulting in a higher recurrence rate [19, 35]. In our study, bilateral hematoma was found to be a risk factor for postoperative recurrence of CSDH, but was not a risk factor for postoperative AIH. Whether the brain re-expansion theory or the brain atrophy theory were correct will require time to accumulate results. In our study, the mean time interval (4.7 ± 2.9 days) between initial surgery and postoperative AIH was significantly lower than the mean time interval (40.8 ± 28.3 days) between initial surgery and postoperative recurrence.
Some studies have reported that male sex is an independent risk factor of CSDH recurrence, and that males likely have more trauma and more frequent complications than females. However, other studies have suggested that gender is not associated with CSDH recurrence [13, 36]. In our study, 295 patients had a history of trauma, including 233 males and 62 females. According to multivariate logistic regression analysis, there was no significant correlation between gender and CSDH recurrence. To date, no literature has reported the relationship between gender and postoperative AIH. We found that gender was not significantly associated with postoperative AIH.
The clinical presentation of CSDH varies from asymptomatic to headache, limb weakness, incontinence, etc. According to our study, preoperative headache is an independent risk factor for postoperative AIH. When CSDH presents as a clinical manifestation of headache, it indicates a higher intracranial pressure and a secondary cerebral blood flow reduction in the deep cerebral regions, causing blood vessels to spasm and increasing the risk of vascular accidents [37]. Thus, when blood flow in the brain changes or intracranial pressure changes significantly in a short period of time, blood vessels rupture, resulting in bleeding.
Many studies suggest that preoperative hematoma density is associated with CSDH recurrence, and hyperdense hematoma is an independent risk factor for CSDH recurrence [13, 38]. In present study, although nearly 1/3 of the patients had hyperdense imaging findings, according to our clinical experience and our definition of CSDH, neurosurgeons evaluated patients with subdural hematoma no matter what the density of subdural hematoma on imaging, once they were able to be treated with BHD, these patients could be managed as patients with CSDH. In our study, hyperdense hematoma were more prone to CSDH recurrence than mixed density (OR, 0.433; 95%CI, 0.229–0.818; P = 0.010, hyperdense as reference). The relationship between hematoma density and postoperative AIH has not been reported in the literature. In our study, hematoma density was not significantly associated with postoperative AIH. We suspect that when hyperdense hematoma are compared with the other three types of hematoma density, repeated microhemorrhages from the immature capillary network in the outer membrane take place and accumulate over time, causing CSDH recurrence [38].
Preoperative hematoma thickness has been reported as an independent risk factor for CSDH recurrence [7]. It is thought that hematoma thickness has an increased tendency to recur because the subdural space is larger than a small lesion postoperatively [7, 36]. As hematoma thickness is related to many factors, such as age, midline shift and brain atrophy, it may not be a useful predictor of CSDH recurrence and postoperative AIH. However, other studies have shown no significant relationship between hematoma thickness and CSDH recurrence [13, 39], and the relationship between hematoma thickness and postoperative AIH has not been reported. In our study, the hematoma thickness of 20 mm was selected as a threshold, compared with the trauma subdural hematoma guidelines threshold of 10 mm, there were two reasons. First, a part of the patients were non-traumatic chronic subdural hematomas; second, according to our clinical experience, when the thickness of hematoma is between 10 mm and 20 mm, some patients had no obvious clinical manifestations and did not require surgical treatment. According to the results, there was no significant relationship between hematoma thickness and CSDH recurrence or postoperative AIH.
Our results showed that anticoagulant drug use is an independent risk factor for CSDH recurrence. Antiplatelet drugs did not increase the CSDH recurrence rate following BHD. Similarly, a recent systematic study showed that anticoagulant drugs increased re-bleeding on the operation side of CSDH, but antiplatelet therapy did not [40]. However, this result is controversial as in other studies, antiplatelets or anticoagulants were not associated with CSDH recurrence [16, 36, 41]. The authors speculated that the reason for this finding may be that the patients were not adequately anticoagulated, especially in the non-recurrence group. At present, only one study has reported that anticoagulants or antiplatelet drugs do not increase the incidence of postoperative AIH [25]. Similar to our results, we suspect that it may be the result offset caused by insufficient sample size. Therefore, a large sample clinical trial is necessary to verify this result.
Atorvastatin is another management option, which may be used alone or in conjunction with surgery. Several studies have shown that CSDH is caused by impaired angiogenesis in the neomembrane and localized inflammation, and that atorvastatin improves angiogenesis and reduces the inflammatory response [42, 43]. A randomized control study showed that the oral administration of atorvastatin is safe and effective in treating CSDH, and promotes the resolution of hematoma [44]. A prospective study showed that atorvastatin administration may decrease the risks of CSDH recurrence [45]. However, in our study, atorvastatin did not reduce the rate of CSDH recurrence, nor did it reduce the incidence of postoperative AIH. We suspect that different research methods may lead to varying results.
In our study, intraoperative saline irrigation was based on the surgeon’s preference. Some studies have shown that intraoperative saline irrigation of the hematoma cavity does not improve the incidence of postoperative AIH and CSDH recurrence [25, 46]. According to our results, intraoperative irrigation does not reduce the risk of CSDH recurrence, however, it does reduce the incidence of postoperative AIH. We speculate that BHD for CSDH without irrigation significantly reduces intracranial pressure for a short period of time. The abrupt decrease in intracranial pressure may cause further damage to the intracranial blood vessels and lead to acute intracranial bleeding.
Our study had some limitations. First, our study is a retrospective design, which usually produces a risk of bias. Based on our data and personal communication with neurosurgeons in each participating department, neurosurgeons not only choose the surgical method based on symptoms and hematoma size, but also according to their preferences. For example, the use of a single burr hole, the 1.5-2 cm craniotomy and whether to irrigate is based on neurosurgeon preference. However, according to literature reports and our results, the selection of these surgical methods did not result in significant differences postoperative complications in total and recurrence rates [25]. Second, in the multivariate model, although ideally more stringent criteria for variable inclusion in the model would be applied in lieu of p < 0.1. However, it may lead to too few variables and too many confounding factors, which will have a greater impact on the results.
Conclusions
In this study, we evaluated predictors of CSDH recurrence and postoperative AIH following BHD in a multi-center retrospective study of patients with CSDH. We identified bilateral hematoma, hyperdense hematoma and anticoagulant drugs as independent risk factors for recurrence of CSDH. Preoperative headache is an independent risk factor for postoperative AIH, and intraoperative irrigation reduces the incidence of postoperative AIH. Further prospective multi-center studies will be required to evaluate these findings.
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AIH:
-
Acute intracranial hemorrhage
- BHD:
-
Burr hole drainage
- CIH:
-
Chronic intracranial hemorrhage
- CSDH:
-
Chronic subdural hematoma
- CT:
-
Computed tomography
- GCS:
-
Glasgow coma scale
- MRI:
-
Magnetic resonance imaging
References
Santarius T, Hutchinson PJ. Chronic subdural haematoma: time to rationalize treatment? Br J Neurosurg. 2004;18(4):328–32.
Asghar M, Adhiyaman V, Greenway MW, Bhowmick BK, Bates A. Chronic subdural haematoma in the elderly--a North Wales experience. J R Soc Med. 2002;95(6):290–2.
Chronic subdural hematoma in elderly people: present status on Awaji Island and epidemiological prospect. 1992.
Karibe H, Kameyama M, Kawase M, Hirano T, Kawaguchi T, Tominaga T. Epidemiology of chronic subdural hematomas. No Shinkei Geka. 2011;39(12):1149–53.
Hsieh CT, Su IC, Hsu SK, Huang CT, Lian FJ, Chang CJ. Chronic subdural hematoma: differences between unilateral and bilateral occurrence. J Clin Neurosci. 2016;34:252–8.
Kolias AG, Chari A, Santarius T, Hutchinson PJ. Chronic subdural haematoma: modern management and emerging therapies. Nat Rev Neurol. 2014;10(10):570–8.
Chon KH, Lee JM, Koh EJ, Choi HY. Independent predictors for recurrence of chronic subdural hematoma. Acta Neurochir. 2012;154(9):1541–8.
Berghauser Pont LM, Dammers R, Schouten JW, Lingsma HF, Dirven CM. Clinical factors associated with outcome in chronic subdural hematoma: a retrospective cohort study of patients on preoperative corticosteroid therapy. Neurosurgery. 2012;70(4):873–80 discussion 880.
Ducruet AF, Grobelny BT, Zacharia BE, Hickman ZL, DeRosa PL, Andersen KN, et al. The surgical management of chronic subdural hematoma. Neurosurg Rev. 2012;35(2):155–69 discussion 169.
Lega BC, Danish SF, Malhotra NR, Sonnad SS, Stein SC. Choosing the best operation for chronic subdural hematoma: a decision analysis. J Neurosurg. 2010;113(3):615–21.
Lind CR, Lind CJ, Mee EW. Reduction in the number of repeated operations for the treatment of subacute and chronic subdural hematomas by placement of subdural drains. J Neurosurg. 2003;99(1):44–6.
Miranda LB, Braxton E, Hobbs J, Quigley MR. Chronic subdural hematoma in the elderly: not a benign disease. J Neurosurg. 2011;114(1):72–6.
Fujitani S, Ishikawa O, Miura K, Takeda Y, Goto H, Maeda K. Factors predicting contralateral hematoma growth after unilateral drainage of bilateral chronic subdural hematoma. J Neurosurg. 2017;126(3):755–9.
Rust T, Kiemer N, Erasmus A. Chronic subdural haematomas and anticoagulation or anti-thrombotic therapy. J Clin Neurosci. 2006;13(8):823–7.
Tahsim-Oglou Y, Beseoglu K, Hänggi D, Stummer W, Steiger H-J. Factors predicting recurrence of chronic subdural haematoma: the influence of intraoperative irrigation and low-molecular-weight heparin thromboprophylaxis. Acta Neurochir. 2012;154(6):1063–8.
Torihashi K, Sadamasa N, Yoshida K, Narumi O, Chin M, Yamagata S. Independent predictors for recurrence of chronic subdural hematoma: a review of 343 consecutive surgical cases. Neurosurgery. 2008;63(6):1125–9 discussion 1129.
Song DH, Kim YS, Chun HJ, Yi HJ, Bak KH, Ko Y, et al. The predicting factors for recurrence of chronic subdural hematoma treated with Burr hole and drainage. Kor J Neurotrauma. 2014;10(2):41–8.
Motiei-Langroudi R, Stippler M, Shi S, Adeeb N, Gupta R, Griessenauer CJ, et al. Factors predicting reoperation of chronic subdural hematoma following primary surgical evacuation. J Neurosurg. 2018;129(5):1143–50.
Han MH, Ryu JI, Kim CH, Kim JM, Cheong JH, Yi HJ. Predictive factors for recurrence and clinical outcomes in patients with chronic subdural hematoma. J Neurosurg. 2017;127(5):1117–25.
Mondorf Y, Abu-Owaimer M, Gaab MR, Oertel JM. Chronic subdural hematoma--craniotomy versus burr hole trepanation. Br J Neurosurg. 2009;23(6):612–6.
Wang W, Liu H, Yang J. Burr hole craniostomy irrigation with and without drainage during surgical treatment of chronic subdural hematoma: a retrospective study of 87 cases. Turk Neurosurg. 2017. https://doi.org/10.5137/1019-5149.JTN.19747-16.2. PMID:29044453.
Yuan Y, Wang QP, Cao YL, Zhang H, Burkutally MSN, Budryte K, et al. Burr hole drainage and burr hole drainage with irrigation to treat chronic subdural hematoma: a systematic review and meta-analysis. Medicine (Baltimore). 2018;97(33):e11827. https://doi.org/10.1097/MD.0000000000011827.PMID:30113471.
Wang S, Ma Y, Zhao X, Yang C, Gu J, Weng W, et al. Risk factors of hospital mortality in chronic subdural hematoma: a retrospective analysis of 1117 patients, a single institute experience. J Clin Neurosci. 2019;67:46–51. https://doi.org/10.1016/j.jocn.2019.06.026. PMID:31213382.
Rohde V, Graf G, Hassler W. Complications of burr-hole craniostomy and closed-system drainage for chronic subdural hematomas: a retrospective analysis of 376 patients. Neurosurg Rev. 2002;25(1–2):89–94.
Pang CH, Lee SE, Kim CH, Kim JE, Kang H-S, Park C-K, et al. Acute intracranial bleeding and recurrence after bur hole craniostomy for chronic subdural hematoma. J Neurosurg. 2015;123(1):65–74.
Bucher B, Maldaner N, Regli L, Sarnthein J, Serra C. Standardized assessment of outcome and complications in chronic subdural hematoma: results from a large case series. Acta Neurochir. 2019;161(7):1297–304.
Ramachandran R, Hegde T. Chronic subdural hematomas--causes of morbidity and mortality. Surg Neurol. 2007;67(4):367–72 discussion 372-363.
Park HS, Park ES, Park JB, Kwon SC, Lyo IU, Kim MH, et al. Chronic subdural hematomas: comparison between unilateral and bilateral involvement. Korean J Neurotrauma. 2014;10(2):55–9.
Huang YH, Yang KY, Lee TC, Liao CC. Bilateral chronic subdural hematoma: what is the clinical significance? Int J Surg. 2013;11(7):544–8.
Tsai TH, Lieu AS, Hwang SL, Huang TY, Hwang YF. A comparative study of the patients with bilateral or unilateral chronic subdural hematoma: precipitating factors and postoperative outcomes. J Trauma. 2010;68(3):571–5.
Motiei-Langroudi R, Thomas AJ, Ascanio L, Alturki A, Papavassiliou E, Kasper EM, et al. Factors predicting the need for surgery of the opposite side after unilateral evacuation of bilateral chronic subdural hematomas. Neurosurgery. 2018;85(5):648–55.
Andersen-Ranberg NC, Poulsen FR, Bergholt B, Hundsholt T, Fugleholm K. Bilateral chronic subdural hematoma: unilateral or bilateral drainage? J Neurosurg. 2017;126(6):1905–11.
Sadrolhefazi A, Bloomfield SM. Interhemispheric and bilateral chronic subdural hematoma. Neurosurg Clin N Am. 2000;11(3):455–63.
Kung WM, Hung KS, Chiu WT, Tsai SH, Lin JW, Wang YC, et al. Quantitative assessment of impaired postevacuation brain re-expansion in bilateral chronic subdural haematoma: possible mechanism of the higher recurrence rate. Injury. 2012;43(5):598–602.
Shen J, Gao Y, Li Q, Ge R, Wang Q, Jiang X, et al. Risk factors predicting recurrence of bilateral chronic subdural hematomas after initial bilateral evacuation. World Neurosurg. 2019;130:e133–9.
Bartek J, Sjåvik K, Kristiansson H, Ståhl F, Fornebo I, Förander P, et al. Predictors of recurrence and complications after chronic subdural hematoma surgery: a population-based study. World Neurosurg. 2017;106:609–14.
Okuyama T, Saito K, Fukuyama K, Yamamoto K, Morimoto M, Aburano T. Clinical study of cerebral blood flow in bilateral chronic subdural hematoma measured by 99mTc-HMPAO SPECT. No To Shinkei. 2000;52(8):709–14.
Lin CC, Lu YM, Chen TH, Wang SP, Hsiao SH, Lin MS. Quantitative assessment of post-operative recurrence of chronic subdural haematoma using mean haematoma density. Brain Inj. 2014;28(8):1082–6.
Nakaguchi H, Tanishima T, Yoshimasu N. Factors in the natural history of chronic subdural hematomas that influence their postoperative recurrence. J Neurosurg. 2001;95(2):256–62.
Nathan S, Goodarzi Z, Jette N, Gallagher C, Holroyd-Leduc J. Anticoagulant and antiplatelet use in seniors with chronic subdural hematoma systematic review. Neurology. 2017;88(20):1889–93.
Okano A, Oya S, Fujisawa N, Tsuchiya T, Indo M, Nakamura T, et al. Analysis of risk factors for chronic subdural haematoma recurrence after burr hole surgery: optimal management of patients on antiplatelet therapy. Br J Neurosurg. 2014;28(2):204–8.
Xu M, Chen P, Zhu X, Wang C, Shi X, Yu B. Effects of atorvastatin on conservative and surgical treatments of chronic subdural hematoma in patients. World Neurosurg. 2016;91:23–8.
Tang R, Shi J, Li X, Zou Y, Wang L, Chen Y, et al. Effects of atorvastatin on surgical treatments of chronic subdural hematoma. World Neurosurg. 2018;117:e425–9.
Jiang R, Zhao S, Wang R, Feng H, Zhang J, Li X, et al. Safety and efficacy of atorvastatin for chronic subdural hematoma in Chinese patients. JAMA Neurol. 2018;75(11):1338–46.
Liu H, Luo Z, Liu Z, Yang J, Kan S. Atorvastatin may attenuate recurrence of chronic subdural hematoma. Front Neurosci. 2016;10:303.
Almenawer SA, Farrokhyar F, Hong C, Alhazzani W, Manoranjan B, Yarascavitch B, et al. Chronic subdural hematoma management: a systematic review and meta-analysis of 34,829 patients. Ann Surg. 2014;259(3):449–57.
Acknowledgments
Not applicable.
Funding
This study was supported the National Natural Science Foundation of China (No.81470052).
Author information
Authors and Affiliations
Contributions
XFY, LG, ZBC, HW designed research, performed research, analyzed data. FMC, KW, KLX collected data, analyzed the data and drafted the manuscript. LW, TXZ, FC collected and analyzed the data. All authors checked and agreed on the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committees of the two medical centers. The requirement for obtaining informed consent from patients was waived because the data sets were anonymous.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, F.M., Wang, K., Xu, K.L. et al. Predictors of acute intracranial hemorrhage and recurrence of chronic subdural hematoma following burr hole drainage. BMC Neurol 20, 92 (2020). https://doi.org/10.1186/s12883-020-01669-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-020-01669-5