Abstract
Background
Coffee consumption represents a negative risk factor for Parkinson’s disease (PD) and seems to affect PD motor symptoms. We aimed to investigate the association between coffee consumption and motor symptoms in de novo PD patients.
Methods
In total, 284 patients with de novo PD were included in the current study. Motor and non-motor symptoms were evaluated using various scales. History of coffee consumption was obtained via a semi-structured interview.
Results
In total, 204 patients were categorized as coffee drinkers and 80 as non-coffee drinkers. Coffee drinkers were predominantly male and had early symptom onset; in addition, they were younger, reported more years in formal education, and had better motor and non-motor scores than did non-coffee drinkers. After adjustments, coffee drinkers had lower tremor scores than did non-coffee drinkers, and coffee consumption was related to tremors in a dose-dependent manner. These relationships were statistically significant in case of rest tremor but not in case of action tremor. The dose-dependent relationship between coffee consumption and tremor severity was significant only in men. Non-motor symptom scores were not significantly different between coffee drinkers and non-coffee drinkers.
Conclusions
Coffee consumption and tremor severity are inversely related in male patients with de novo PD.
Similar content being viewed by others
Background
Parkinson’s disease (PD) is a heterogeneous neurodegenerative disorder with diverse clinical manifestations that include both motor and non-motor symptoms [1]. Cardinal motor symptoms used for diagnosing PD include bradykinesia, which is one of the most important features, as well as rigidity, resting tremor, and postural instability [2]. Since tremor may have a different pathophysiology than bradykinesia and rigidity [3], the response of tremor to dopaminergic agents is less clear than that of bradykinesia or rigidity [4].
Previous epidemiological studies established that coffee is a negative risk factor for PD [5,6,7,8]. This is further supported by a study showing that caffeine, a major chemical component of coffee, attenuates the loss of striatal dopamine and dopamine transporter binding sites in an experimental PD mouse model [9]. Additional experimental and observational PD studies demonstrated that coffee consumption had a beneficial effect on PD motor symptoms [10, 11]. Since coffee consumption reduces the risk of PD, there might be a relationship between coffee consumption and the severity of motor symptoms. However, few studies have investigated the relationship between coffee consumption and PD motor symptoms.
Gender differences in PD phenotypic presentation and disease progression are widely accepted, and the impact of caffeine on PD differs based on gender [5, 12,13,14,15]. In addition, the association between coffee consumption and the severity of motor symptoms may differ between genders. Therefore, in the current study, we investigated the association between coffee consumption and motor symptoms in de novo PD patients based on their gender.
Methods
Study population
We performed a baseline survey to determine the association between coffee consumption and motor symptoms in a cohort of newly diagnosed, treatment-naïve, early-stage PD patients consisting of 284 participants. All participants were enrolled from the outpatient clinic at the Chonnam National University Hospital and were recruited consecutively from January 2011 to December 2016.
Parkinsonism comprises multiple syndromes including PD. Thus, according to the international criteria, both parkinsonism and PD symptoms must be evaluated to make a proper PD diagnosis [2]. Parkinsonism is defined by the presence of bradykinesia and one additional symptom, including 4–6 Hz rest tremor, muscular rigidity, or postural instability not caused by primary visual, vestibular, cerebellar, or proprioceptive dysfunction, according to a previous study [2]. The United Kingdom Parkinson’s Disease Society Brain Bank clinical diagnostic criteria were used for the clinical diagnosis of PD [2]. An additional inclusion criterion for our study was the lack of significant cerebral lesions, as assessed by brain magnetic resonance imaging (MRI). None of the patients had a history of taking either antiparkinsonian or antidopaminergic agents. In contrast, the exclusion criteria were an uncertain diagnosis, secondary or atypical parkinsonism according to the recent clinical diagnostic criteria [16,17,18,19], failure to complete the coffee consumption questionnaire, and dementia. The time at which one of the four cardinal PD signs was first noted by the patient or caregiver was defined as the onset of PD.
All participants provided written informed consent. The study was approved by the Institutional Review Board of the hospital and was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki.
Clinical evaluation
All PD patients were diagnosed by a specialist in movement disorders (S.M.Choi). The history of the patient and a neurological examination were used to obtain detailed clinical information, prior to the administration of antiparkinsonian medication.
Participants underwent a thorough neurological examination and were asked about the age at symptom onset and duration of formal education, as well as past and current medications. Both the severity and stage of the parkinsonism were evaluated using the modified Hoehn and Yahr (mHY) staging scale and Unified Parkinson’s Disease Rating Scale (UPDRS) motor (part III) and activities of daily living (ADL; part II) sub-scores. The effect of coffee consumption on the sum of each motor symptom score in the UPDRS, in addition to postural instability and gait disturbance (PIGD) and akinetic-rigid (AR) scores, was evaluated. Patients were scored for these variables using the methods proposed by both Jankovic at al. and Kang et al. [20, 21]. In short, in Jankovic’s method, the tremor score was calculated by dividing the sum of the UPDRS III items 20 and 21 and UPDRS II item 16 by 8, whereas the PIGD score was calculated by dividing the sum of the UPDRS III items 29 and 30 and UPDRS II items 13–15 by 5 [20, 22]. In contrast, in Kang’s method, the tremor score was calculated by dividing the sum of the UPDRS III items 20 and 21 by 4, and the AR score was calculated by dividing the sum of the UPDRS III items 22–27 and 31 by 15 [21].
To evaluate non-motor PD symptoms and general cognition, the Korean versions of the Mini-Mental State Examination (K-MMSE) and the Montreal Cognitive Assessment (MoCA-K) were used [23, 24]. Additionally, the Non-Motor Symptoms assessment scale for PD (NMSS) and the Beck Depression Inventory (BDI) were used [25, 26].
Data on past and present coffee consumption were obtained via a semi-structured interview. In brief, the interview had the following questions: 1) Have you ever had coffee or do you currently drink coffee? 2) If you have ever drunk coffee, when did you start drinking coffee? 3) How long have you been drinking coffee? 4) On average, how many cups of coffee do you drink per day? 5) If you have stopped drinking coffee, when did you stop drinking coffee? For the analyses, we allocated our participants to two groups, the coffee drinker and non-coffee drinker group.
Statistical analysis
The results are presented as the mean ± standard deviation (SD) for continuous variables while numbers and percentages are provided for categorical variables. Comparisons of the demographic and clinical variables between PD patients with and without a history of drinking coffee were conducted using bivariate analyses (Student’s t-test or chi-square test, depending on the data distribution). Adjustments were made for the variables when bivariate analyses revealed a significant difference between coffee and non-coffee drinkers. Comparison of the severity of motor and non-motor scores between PD patients with and without a history of drinking coffee was conducted using analysis of covariance (ANCOVA), which controlled for the significantly different demographic and clinical variables. We further evaluated the dose-dependent effect of the amount of coffee consumption in a day. Additionally, such analyses were performed in each gender subgroup to investigate the gender differences underlying the association. The p-values for the motor score on UPDRS and motor score on subtypes were corrected for by multiple testing using the false discovery rate. All statistical analyses were performed using the SPSS software for Windows (version 22.0, IBM corp., Armonk, NY, USA). A p-value < 0.05 was considered statistically significant.
Results
Comparison between coffee and non-coffee drinkers
Of the 284 de novo PD patients enrolled (Table 1), a total of 204 patients (71.83%) and 80 patients (28.17%) were categorized as coffee drinkers (coffee drinker group) and non-coffee drinkers (non-coffee drinker group), respectively. The coffee drinker group comprised current coffee drinkers and those who have had coffee in the past but have now stopped. Most of the patients who quit drinking coffee had a history of coffee drinking for more than 10 years. As shown in Table 2, intergroup comparisons revealed that coffee drinkers were younger, included more men, younger in age at cardinal motor symptom onset, and reported more years in formal education than the non-coffee drinkers. When comparing motor- and ADL-related scores, coffee drinkers had significantly lower UPDRS motor scores (p = 0.020) as well as tremor (p = 0.002), bradykinesia (p = 0.022), and gait and posture (p = 0.022) scores than non-coffee drinkers. When the tremor was divided into rest and action tremors, only rest tremor (p = 0.001) showed a significant difference. Furthermore, the univariate analysis revealed that coffee drinkers had significantly lower tremor scores (p = 0.001 for Jankovic’s method, p = 0.002 for Kang’s method) than non-coffee drinkers. However, PIGD and AR scores were not significantly different between the two groups. When comparing non-motor scores, we found that coffee drinkers had higher MMSE (p = 0.005), but lower BDI (p = 0.005) and total NMSS (p = 0.007) scores than non-coffee drinkers.
After adjustment for significant clinical variables found in the univariate analysis, we found that rest tremor score (p = 0.001) on UPDRS and tremor scores on Jankovic’s and Kang’s methods (all p-values < 0.001) were lower in coffee drinkers than in non-coffee drinkers. However, scores related to other motor manifestations, such as bradykinesia, gait and posture, PIGD, and AR, were not significantly different between the two groups. Furthermore, after adjustment, there was no significant difference between the two groups for all the non-motor symptom scores (Table 2).
Since the prevalence of coffee consumption differed according to gender, we compared the demographic and clinical variables between coffee drinkers and non-coffee drinkers in each gender. Similar to the results described above, rest tremor scores were lower in coffee drinkers than in non-coffee drinkers in both the male and female subgroups, after adjusting for the significant variables found in the univariate analysis (Table 3).
Dose-dependent relationship between coffee consumption and PD symptoms
The median value of coffee consumption was one cup a day; therefore, PD patients were categorized as non-coffee drinkers, coffee drinkers - one cup a day, and coffee drinkers - more than one cup a day, to evaluate the dose-dependent effect of the coffee consumption on tremor. We found that mHY stage, UPDRS motor, UPDRS tremor, UPDRS rest tremor, UPDRS bradykinesia, UPDRS gait and posture, tremor scores in both the Jankovic’s and Kang’s methods, and the AR score in Kang’s method were inversely related to the number of cups of coffee per day, and this was significant. Additionally, we found a significant inverse relationship between the BDI score and the number of cups of coffee per day, although MMSE and MoCA scores were directly related to the number of cups of coffee per day. However, after adjustment for the confounders, only tremor scores (UPDRS tremor, UPDRS rest tremor, and tremor scores in both Jankovic’s and Kang’s methods) were found to be related to coffee consumption in a dose-dependent manner (Table 4).
Finally, we evaluated the dose-dependent effect of coffee consumption on tremor in each gender. Tremor scores (UPDRS tremor, UPDRS rest tremor, and tremor scores in both the Jankovic’s and Kang’s methods) had an inverse relationship with coffee consumption in a dose-dependent manner only in the male subgroup, after adjustment for significant clinical variables found in the univariate analysis (Table 5).
Discussion
This study investigated the relationship between coffee consumption and motor symptoms in de novo PD patients. In summary, we found that 1) coffee drinkers have lower tremor scores than non-coffee drinkers, 2) the low tremor scores in coffee drinkers are found in both the male and female subgroups, 3) coffee consumption is related to tremor in a dose-dependent manner, 4) the relationship between coffee consumption and tremor was statistically significant only in rest tremor, not in action tremor, and 5) the dose-dependent, inverse relationship between coffee consumption and tremor scores was significant only in the male subgroup.
The relationship between coffee consumption and tremor is controversial. Some people have previously stated that drinking coffee made their hands prone to tremor, and a small proportion of patients with essential tremor or PD thought that coffee worsened their tremor [27]. However, caffeine only infrequently induces tremor in the general population, and it does not exacerbate pathological tremor [27, 28]. Although caffeine consumption is not correlated to tremor severity in patients with essential tremor [29], currently, no studies exist on the association between caffeine and tremor in PD patients. Our study shows that coffee consumption could attenuate tremor severity in de novo PD patients.
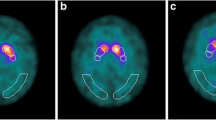
Tremor may have distinct pathophysiology compared to bradykinesia and rigidity. Previous neuroimaging studies reported that patients with the tremor-dominant PD subtype show higher dopamine transporter binding than those with the AR subtype, whereas tremor severity does not correlate to striatal dopamine deficits [30, 31]. Furthermore, another neuroimaging study revealed the involvement of both the cerebellothalamic circuit and basal ganglia in PD tremor generation [32]. Coffee is a major source of caffeine, which is the most widely consumed methylxanthine (1,3,4-trimethylxanthine) and is also a nonspecific adenosine A1/A2A receptor antagonist. Several studies have suggested that A2A receptor antagonists have a tremolytic effect in PD animal models [10, 33, 34]. Although it is possible that caffeine has a symptomatic benefit on tremor, there might be other explanations, including the neuroprotective effect of caffeine, reverse causality (prodromal PD patients might have reduced desires for caffeine), or residual confounding by other factors (specific personality or changes in reward mechanism in PD) [35]. In this study, we found that coffee consumption prior to diagnosis could influence tremor severity in de novo PD patients. Selective adenosine A2A antagonism through the modulation of basal ganglia function via opposing dopamine D2 receptors seems to be effective for the treatment of PD motor symptoms as a monotherapy or an adjunct therapy to dopaminergic agents [36, 37]. We believe that the effects of coffee on tremor severity in PD patients could be caused by the modulation of dopaminergic signaling even before clinical diagnosis. As such, future large prospective studies should investigate the therapeutic effects of coffee or adenosine A2A antagonists on tremor in PD. The findings from this study, therefore, suggest a potential therapeutic option for PD tremor, which responds less effectively to dopaminergic treatment than bradykinesia or rigidity.
In our study, the relationship between coffee consumption and tremor was significant only in rest tremor. One possible explanation is that rest tremor rather than action tremor is a typical symptom that reflects Parkinson’s pathophysiology [38]. However, these results could be related to the limitations of the UPDRS scoring system, because the total score of rest tremor is higher than that of action tremor.
A number of studies on the gender differences in PD patients were reported [13]. For example, although female PD patients show a mild disease phenotype at first, they have a more aggressive disease progression and a higher probability of motor complications as the disease progresses [13]. The impact of coffee and caffeine on PD risk and mortality also differs between genders [5, 12, 14, 15]. In fact, our study shows that the dose-dependent inverse association between coffee consumption and tremor severity is prominent in men but not in women. Such gender differences in PD have been partly explained by the effect of estrogen. Similar to our results, caffeine was reported to reduce the risk of PD, and its beneficial effect was prevented by the use of estrogen replacement therapy [12]. In addition, caffeine was found to reduce the risk of PD in postmenopausal women without hormonal replacement therapy; however, increased PD risk was observed in estrogen users [39]. Since estrogen has neuroprotective or neurotrophic effects and modulates the nigrostriatal dopaminergic system [40], we suggest that estrogen modulates the effects of caffeine on the dopaminergic system and that a complex interaction between caffeine, estrogen, and dopamine exists in the basal ganglia system. Large prospective studies could elucidate the mechanism behind such observations.
In this study, we included de novo PD patients to ensure that the effects of medication would not represent a confounder. Additionally, we prospectively recruited patients with PD based on a registry to reduce the selection bias. Our study has several limitations. First, there were significant differences between coffee drinkers and non-coffee drinkers in demography, including age, sex, age at symptom onset, and formal education. Although, we adjusted for these variables in other analyses, it is possible that these differences could affect the relationship between coffee consumption and tremor. Second, we investigated the association between coffee consumption and motor symptoms in de novo PD patients only, without examining control or advanced PD groups. Further controlled studies would reveal a more precise association between tremor severity and coffee consumption in PD patients. Third, this study did not include information regarding the consumption of other caffeine-containing beverages. There is a possibility that other beverages containing caffeine can influence motor symptoms in PD patients. Fourth, we did not collect information on the menopausal status and hormonal replacement therapy in women. Therefore, the analysis of the association between coffee consumption and motor severity in the female subgroup according to the hormonal status was not possible.
Conclusion
Coffee drinkers had lower tremor scores when compared to non-coffee drinkers, and the coffee consumption was inversely related to tremor severity in a dose-dependent manner in de novo PD patients. These relationships were statistically significant only in rest tremor, not in action tremor. The effect of coffee consumption on tremor severity was gender-dependent, and it was significant only in men. Further investigations are needed to reveal the exact causal relationship between coffee consumption and tremor in PD patients.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ADL:
-
Activities of daily living
- ANCOVA:
-
Analysis of covariance
- AR:
-
Akinetic-rigid
- BDI:
-
Beck Depression Inventory
- K-MMSE:
-
Korean versions of the Mini-Mental State Examination
- mHY:
-
modified Hoehn and Yahr scale
- MoCA-K:
-
Montreal Cognitive Assessment
- MRI:
-
Magnetic resonance imaging
- NMSS:
-
Non-Motor Symptoms assessment scale for Parkinson’s disease
- PD:
-
Parkinson’s disease
- PIGD:
-
Postural instability and gait disturbance
- SD:
-
Standard deviation
- UPDRS:
-
Unified Parkinson’s Disease Rating Scale
References
Lees AJ, Hardy J, Revesz T. Parkinson’s disease. Lancet. 2009;373:2055–66.
Hughes AJ, Daniel SE, Ben-Shlomo Y, et al. The accuracy of diagnosis of parkinsonian syndromes in a specialist movement disorder service. Brain. 2002;125(Pt 4):861–70.
Hallett M. Parkinson’s disease tremor: pathophysiology. Parkinsonism Relat Disord. 2012;18(Suppl 1):S85–6.
Hallett M. Tremor: pathophysiology. Parkinsonism Relat Disord. 2014;20(Suppl 1):S118–22.
Ross GW, Abbott RD, Petrovitch H, et al. Association of coffee and caffeine intake with the risk of Parkinson disease. JAMA. 2000;283:2674–9.
Nefzger MD, Quadfasel FA, Karl VC. A retrospective study of smoking in Parkinson's disease. Am J Epidemiol. 1968;88:149–58.
Hellenbrand W, Seidler A, Boeing H, et al. Diet and Parkinson's disease. I: a possible role for the past intake of specific foods and food groups. Results from a self-administered food-frequency questionnaire in a case-control study. Neurology. 1996;47:636–43.
Fall PA, Fredrikson M, Axelson O, et al. Nutritional and occupational factors influencing the risk of Parkinson’s disease: a case-control study in southeastern Sweden. Mov Disord. 1999;14:28–37.
Chen JF, Xu K, Petzer JP, et al. Neuroprotection by caffeine and a (2A) adenosine receptor inactivation in a model of Parkinson's disease. J Neurosci. 2001;21:RC143.
Morelli M, Di Paolo T, Wardas J, et al. Role of adenosine A2A receptors in parkinsonian motor impairment and l-DOPA-induced motor complications. Prog Neurobiol. 2007;83:293–309.
Schwarzschild MA, Agnati L, Fuxe K, et al. Targeting adenosine A2A receptors in Parkinson's disease. Trends Neurosci. 2006;29:647–54.
Ascherio A, Weisskopf MG, O'Reilly EJ, et al. Coffee consumption, gender, and Parkinson's disease mortality in the cancer prevention study II cohort: the modifying effects of estrogen. Am J Epidemiol. 2004;160:977–84.
Picillo M, Nicoletti A, Fetoni V, et al. The relevance of gender in Parkinson's disease: a review. J Neurol. 2017;264:1583–607.
Ascherio A, Zhang SM, Hernan MA, et al. Prospective study of caffeine consumption and risk of Parkinson's disease in men and women. Ann Neurol. 2001;50:56–63.
Benedetti MD, Bower JH, Maraganore DM, et al. Smoking, alcohol, and coffee consumption preceding Parkinson's disease: a case-control study. Neurology. 2000;55:1350–8.
Gilman S, Wenning GK, Low PA, et al. Second consensus statement on the diagnosis of multiple system atrophy. Neurology. 2008;71:670–6.
Litvan I, Agid Y, Calne D, et al. Clinical research criteria for the diagnosis of progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome): report of the NINDS-SPSP international workshop. Neurology. 1996;47:1–9.
Lang AE. Cortical basal ganglionic degeneration presenting with “progressive loss of speech output and orofacial dyspraxia”. J Neurol Neurosurg Psychiatry. 1992;55:1101.
McKeith IG. Consensus guidelines for the clinical and pathologic diagnosis of dementia with Lewy bodies (DLB): report of the consortium on DLB international workshop. J Alzheimers Dis. 2006;9(3 Suppl):417–23.
Jankovic J, McDermott M, Carter J, et al. Variable expression of Parkinson's disease: a base-line analysis of the DATATOP cohort. The Parkinson Study group. Neurology. 1990;40:1529–34.
Kang GA, Bronstein JM, Masterman DL, et al. Clinical characteristics in early Parkinson's disease in a Central California population-based study. Mov Disord. 2005;20:1133–42.
Stebbins GT, Goetz CG, Burn DJ, et al. How to identify tremor dominant and postural instability/gait difficulty groups with the movement disorder society unified Parkinson's disease rating scale: comparison with the unified Parkinson's disease rating scale. Mov Disord. 2013;28:668–70.
Kang Y, Na DL, Hahn S. A validity study on the Korean mini-mental state examination (K-MMSE) in dementia patients. J Korean Neurol Assoc. 1997;15:300–8.
Lee JY, Dong Woo L, Cho SJ, et al. Brief screening for mild cognitive impairment in elderly outpatient clinic: validation of the Korean version of the Montreal cognitive assessment. J Geriatr Psychiatry Neurol. 2008;21:104–10.
Martinez-Martin P, Rodriguez-Blazquez C, Abe K, et al. International study on the psychometric attributes of the non-motor symptoms scale in Parkinson disease. Neurology. 2009;73:1584–91.
Beck AT, Beamesderfer A. Assessment of depression: the depression inventory. Mod Probl Pharmacopsychiatry. 1974;7:151–69.
Koller W, Cone S, Herbster G. Caffeine and tremor. Neurology. 1987;37:169–72.
Morgan JC, Sethi KD. Drug-induced tremors. Lancet Neurol. 2005;4:866–76.
Louis ED, Jurewicz EC, Applegate L, et al. Semiquantitative study of current coffee, caffeine, and ethanol intake in essential tremor cases and controls. Mov Disord. 2004;19:499–504.
Spiegel J, Hellwig D, Samnick S, et al. Striatal FP-CIT uptake differs in the subtypes of early Parkinson's disease. J Neural Transm (Vienna). 2007;114:331–5.
Rossi C, Frosini D, Volterrani D, et al. Differences in nigro-striatal impairment in clinical variants of early Parkinson’s disease: evidence from a FP-CIT SPECT study. Eur J Neurol. 2010;17:626–30.
Helmich RC, Janssen MJ, Oyen WJ, et al. Pallidal dysfunction drives a cerebellothalamic circuit into Parkinson tremor. Ann Neurol. 2011;69:269–81.
Correa M, Wisniecki A, Betz A, et al. The adenosine A2A antagonist KF17837 reverses the locomotor suppression and tremulous jaw movements induced by haloperidol in rats: possible relevance to parkinsonism. Behav Brain Res. 2004;148:47–54.
Simola N, Fenu S, Baraldi PG, et al. Blockade of adenosine A2A receptors antagonizes parkinsonian tremor in the rat tacrine model by an action on specific striatal regions. Exp Neurol. 2004;189:182–8.
Postuma RB, Anang J, Pelletier A, et al. Caffeine as symptomatic treatment for Parkinson disease (Café-PD). Neurology. 2017;89:1795–803.
Ferre S, Fredholm BB, Morelli M, et al. Adenosine-dopamine receptor-receptor interactions as an integrative mechanism in the basal ganglia. Trends Neurosci. 1997;20:482–7.
Kondo T, Mizuno Y, Japanese Istradefylline Study G. A long-term study of istradefylline safety and efficacy in patients with Parkinson disease. Clin Neuropharmacol. 2015;38:41–6.
Deuschl G, Bain P, Brain M, and an Ad Hoc Scientific Committee. Mov Disord. 1998;13:2–23.
Ascherio A, Chen H, Schwarzschild MA, et al. Caffeine, postmenopausal estrogen, and risk of Parkinson's disease. Neurology. 2003;60:790–5.
Shulman LM. Is there a connection between estrogen and Parkinson's disease? Parkinsonism Relat Disord. 2002;8:289–95.
Acknowledgements
We would like to thank all patients, researchers, and institutions for their collaboration and contribution to this study.
Authors’contributions
BHC: study concept and design, data analysis and interpretation, drafting of the manuscript. BCK: data analysis and interpretation, critical revision of the manuscript for important intellectual content. SMC: study design, acquisition of data, data analysis and interpretation, critical revision of the manuscript for important intellectual content. All authors have edited and critically reviewed the paper for intellectual content and approved the final version of the paper.
Funding
This work was supported by a grant from the Brain Research Program through the National Research Foundation of Korea, funded by the Ministry of Science, ICT, & Future Planning NRF-2016M3C7A1905469 (to BC Kim). The funder involved in the collection and analysis of data and approved the final submission.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Institutional Review Board of the Chonnam National University Hospital and was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki. All participants provided their written informed consent to participate in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Cho, BH., Choi, SM. & Kim, B.C. Gender-dependent effect of coffee consumption on tremor severity in de novo Parkinson’s disease. BMC Neurol 19, 194 (2019). https://doi.org/10.1186/s12883-019-1427-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-019-1427-y