Abstract
Background
Epileptic seizures can lead to cardiac arrhythmias. The arrhythmias may be in the form of tachycardia, bradycardia or asystole. Ictal bradycardia and asystole can lead to sudden unexpected death.
Case presentation
A case report of a 40-year-old male with complex partial temporal lobe epilepsy. He has coincident attacks of fall and pallor. The patient underwent simultaneous electrocardiogram (ECG) and video electroencephalogram (EEG) monitoring. The slow activity in EEG coincide with the appearance of bradycardia in ECG then cardiac asystole which clinically correspond to the patient syncope. After insertion of a cardiac pacemaker, only complex partial attacks develop with a marked reduction in frequency and no more fall attacks.
Conclusion
Epileptic seizures can present with cardiac arrhythmias, with ictal asystole leading to sudden unexpected death. Simultaneous EEG and ECG are essential for the diagnosis. A cardiac pacemaker can be lifesaving for patients with ictal arrhythmias.
Similar content being viewed by others
Background
Epileptic seizures can affect the heart rate leading to arrhythmia [1]. The most common arrhythmia associated with epilepsy is ictal tachycardia (80–100% of all seizures) [2]. Ictal bradycardia occurs in fewer than 6% of seizures. This slowing of the heart rate may be severe enough to cause ictal asystole. Ictal asystole defined as the absence of ventricular complexes for more than 4 s, accompanied by electrographic seizure onset [3].
Ictal asystole is found in 0.27–0.4% of patients undergoing video-EEG. Clinically, a loss of epileptic activity occurs due to brain anoxia along with a loss of muscle tone and consciousness [4, 5]. Approximately 80% of cases are associated with temporal lobe epilepsy while 20% of cases occur with extratemporal lobe seizures [6, 7].
Ictal bradycardia and ictal asystole may lead to sudden unexpected death in epilepsy patients (SUDEP) [8, 9].
Case presentation
The patient is a 40- years- old right-handed Egyptian male accountant with a negative perinatal history, no family history of epilepsy, no consanguineous marriage, and no medical comorbidities.
At the age of 23, after graduating from university, his father noticed recurrent nocturnal attacks in the form of right-sided head and neck deviation with tonic movements in both the upper and lower limbs. The episodes lasted for approximately 30–40 s and recurred 2–3 times on the same night with no tongue biting or urinary incontinence.
Conventional EEG showed left temporal epileptiform discharge.
Improvement was observed with carbamazepine (400 mg/day), and the patient became seizure-free for 1 year.
At the age of 32, he started to develop recurrent attacks with the following characteristics: A prodromal sense of dizziness followed by loss of contact with the environment, automatism, and stereotyped motor movement in both the upper and lower limbs (marching movements). He became pale and then experienced a loss of tone, causing him to fall to the ground, lasting 40–60 s. No tongue biting or urinary incontinence were reported, but sometimes self-injuries occurred. Then the patient regained consciousness after approximately 15 min of confusion. Each time he asked, “What day is it today?” and “What time is it?” This episode was followed by a sense of fatigue.
These attacks did not occur out of sleep and recurred every 1–2 weeks.
Neurological Examination, conventional EEG, and brain magnetic resonance imaging (MRI) were normal.
The patient was prescribed levetiracetam 2000 mg /day, oxcarbazepine 500 mg/day, clonazepam 0.5 mg /day, and lacosamide 150 mg per day with a partial reduction in the frequency of the attacks.
When patient attended our clinic, he was monitored to ensure that he was compliant with his medications, and the doses were adjusted according to his body weight. We increased the doses and gave him 4 anti-epileptic drugs (AEDs) (Levetiracetam 3000 mg, oxcarbazepine 900 mg, lacosamide 200 mg, clonazepam 0.5 mg/day).
The frequency of events (dizziness, loss of contact, motor automatism) was reduced. However, the attacks of pallor and falling still recurred once per month. Sometimes the attacks were related to psychological or mental stress. Thus, the patient was referred for overnight video-EEG in our unit.
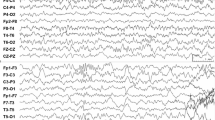
The video- EEG recording was performed overnight using a Nihon Kohden Neurofax 9200 EEG apparatus (Tokyo, Japan). The electrodes were applied according to the 10–20 electrode placement system, in addition to T1 and T2 electrodes. An additional ECG channel was included. Three minutes of hyperventilation and photic stimulation were performed as provocative procedures (Fig. 1).
The patient was awake when his father indicated that the usual seizure had started. The patient had lost contact and began experiencing motor automatism in the form of repetitive movements of the right hand, then the left hand, and finally, the lower limbs. The EEG showed rhythmic alpha frequencies over the left temporal region evolving into theta frequencies that involved both hemispheres. Then, the patient turned his head to the left side and displayed tonic movement in both upper limbs. The simultaneous EEG revealed bilateral, rhythmic temporal theta frequencies. The ECG channel showed 5 s of bradycardia then a 10- s asystole (Fig. 2). Approximately 7 s after the onset of asystole, the patient had atonia and fell to the right side (syncope). The EEG indicated diffuse slowing with amplitude suppression. Next, the patient showed tonic extensor posturing of the right upper limb and brief myoclonic jerks. Here, the EEG was masked by movement and electromyogram (EMG) artifacts. Meanwhile, the ECG revealed bradycardia and then a regular rhythm.
After video EEG ictal recording we decided to stop lacosamide 200 mg to avoid the aggravation of the cardiac arrhythmia. In the same week, the patient was referred for permanent cardiac pacemaker implantation and advised to continue his prescribed antiepileptic medications.
After implantation of a dual chamber pacemaker, only complex partial attacks occurred and did so with a lower frequency. No additional falling attacks followed.
Discussion
A complex relationship exists between seizures and the heart.
Epileptic activity originating in the amygdala, insular cortex, cingulate gyrus, frontopolar region, and frontotemporal region can produce a broad range of cardiac abnormalities, including supraventricular tachycardia, sinus tachycardia, sinus bradycardia, sinus arrest, atrioventricular block, and asystole [4].
Intraoperative stimulation of the human insular cortex reveals that right insular stimulation leads to tachycardia and pressor responses, while left insular stimulation leads to bradycardia and depressor responses [10].
Ictal bradycardia is observed in patients with a long history of epilepsy, especially those with refractory seizures. This may occur because repeated seizures or antiepileptic drugs use impairs the neurocardiac regulatory system [11].
Ictal asystole should be suspected if the typical seizure semiology is associated with syncopal episodes [12, 13].
Simultaneous EEG and ECG recordings are the only methods to differentiate between primary cerebrogenic and cardiogenic causes of arrhythmias. In primary cerebrogenic bradyarrhythmia, EEG seizure activity precedes the onset of bradyarrhythmia. Also, a 24-h Holter ECG is essential to exclude intrinsic cardiac disease, which may be a predisposing factor for ictal asystole [10].
This case is a diagnostic challenge and difficult to be diagnosed unless in a highly specialized integrated epilepsy unit with a rapid and easy referral and effective communication between departments.
Conclusion
Epileptic seizures can present with cardiac arrhythmias and ictal asystole, which may lead to sudden unexpected death. Simultaneous EEG and ECG recordings are essential for diagnosis. A cardiac pacemaker can be lifesaving for patients with ictal arrhythmias.
Abbreviations
- AEDs:
-
Anti-epileptic drugs
- ECG:
-
Electocardiogram
- EEG:
-
Electroencephalogram
- EMG:
-
Electromyogram
- MRI:
-
Magnetic resonance imaging
- SUDEP:
-
Sudden unexpected death in epilepsy patients
References
Nei M, Ho RT, Sperling MR. EKG abnormalities during partial seizures in refractory epilepsy. Epilepsia. 2000;41(5):542–8.
Sevcencu C, Struijk JJ. Autonomic alterations and cardiac changes in epilepsy. Epilepsia. 2010;51(5):725–37.
Moseley BD, Ghearing GR, Munger TM, Britton JW. The treatment of ictal asystole with cardiac pacing. Epilepsia. 2011;52(4):e16–9.
Rocamora R, Kurthen M, Lickfett L, Von Oertzen J, Elger CE. Cardiac asystole in epilepsy: clinical and neurophysiologic features. Epilepsia. 2003;44:179–85. https://doi.org/10.1046/j.1528-1157.2003.15101.x.
Nguyen-Michel V-H, Adam C, Dinkelacker V, Pichit P, Boudali Y, Dupont S, et al. Characterization of seizure-induced syncopes: EEG, ECG, and clinical features. Epilepsia. 2014;55(1):146–55.
Mascia A, Quarato PP, Sparano A, Esposito V, Sebastiano F, Occhiogrosso G, et al. Cardiac asystole during right frontal lobe seizures: a case report. Neurol Sci. 2005;26:340–3.
Duplyakov D, Golovina G, Lyukshina N, Surkova E, Elger CE, Surges R. Syncope, seizure-induced bradycardia, and asystole: two cases of clinical and pathophysiological features. Seizure. 2014;S1059-1311(14):00070–3.
Hirsh LJ, Hauser WA. Can sudden unexplained death in epilepsy be prevented? Lancet. 2004;364:2157–8.
Bergen DC. In a heartbeat: autonomic changes during seizures. Epilepsy Curr. 2005;5:194–6.
Lim EC, Lim S, Wilder-Smith E. Brain seizes, heart ceases: a case of ictal asystole. J Neurol Neurosurg Psychiatry. 2000;69:557–9.
Jansen K, Lagae L. Cardiac changes in epilepsy. Seizure. 2010;19:455–60.
Rubboli G, Bisulli F, Michelucci R, Meletti S, Ribani MA, Cortelli P, et al. Sudden falls due to seizure-induced cardiac asystole in drug-resistant focal epilepsy. Neurology. 2008;70:1933–5.
Beal JC, Sogawa Y, Ceresnak SR, Mahgerefteh J, Moshe SL. Late-onset ictal asystole in refractory epilepsy. Paediatr Neurol. 2011;45:253–5.
Acknowledgments
Many thanks to our cooperative patient, the nurses, the EEG technicians and the operative team and finally to our head of the department for her support and encouragement.
This publication is approved by all authors and explicitly by the responsible authorities where the work was carried out, and that, if accepted, it will not be published elsewhere in the same form, in English or any other language.
Availability of data and materials
The authors declare that all the data regarding the patient condition is included in the manuscript and the supplementary files (Figs. 1 and 2).
Author information
Authors and Affiliations
Contributions
NK and AR had performed the interview and did the clinical assessment of the patient; AN was responsible for the video EEG and its interpretation; AE was the one who did the cardiac evaluation and inserted the pacemaker. All authors shared in the writing, read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research is approved by the research ethics committee of the faculty of medicine, Cairo University. An informed written consent was taken from the patient to participate in the study.
Consent for publication
The authors have obtained an informed written consent from the patient to publish any data, image or video related to his case and that these data will be accessible to anyone through the internet.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kishk, N., Nawito, A., El-Damaty, A. et al. Ictal asystole: a case presentation. BMC Neurol 18, 100 (2018). https://doi.org/10.1186/s12883-018-1105-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-018-1105-5