Abstract
Background
Epidemiologic studies has shown an association of albuminuria and low estimated glomerular filtration rate (eGFR) with dementia, but the findings are inconsistent. This study examines the association between eGFR, MA with dementia and its subtypes: AD, VaD, a mixture of AD/VaD, and other dementias.
Methods
Data from the second wave of the HUNT 2 Study (1995–1997) were linked with a dementia register known as the Health and Memory Study (HMS) collected during 1995–2011 in Nord-Trøndelag County, Norway. Dementia was ascertained using World Health Organization’s ICD-10 criteria into subtypes: AD,VaD, mixed AD/VaD, and other dementia. eGFR and its association with dementia was examined in 48,508 participants of the HUNT Study, of which 668 were diagnosed with all-cause dementia. Association between MA and dementia were studied in a subset of 7024 participants, and 214 were diagnosed with all-cause dementia. Cox regression models were conducted analyzing the association between dementia and MA using albumin creatine ratio (ACR). Cox regression models and Fine-Gray models were used to examine the association between dementia and eGFR.
Results
A positive association was found between increasing ACR and dementia. ACR in the fourth quartile (> 1.78 mg/mmol) with increased hazard ratio of VaD, 3.97 (1.12 to 14.07), compared with ACR in the first quartile (<.53 mg/mmol). There was no association between eGFR and dementia or its subgroups.
Conclusions
Our results strengthens the hypothesis that vascular mechanisms may affect both kidney and brain as an association between MA and dementia was found. However, eGFR was not significantly associated with dementia independent of diabetes mellitus or hypertension.
Similar content being viewed by others
Background
As dementia remains to be irreversible, studies continue to examine modifiable risk factors aimed at prevention [1]. The ageing population is growing, and the number of patients with chronic kidney disease (CKD) is expected to increase [2]. Estimated glomerular filtration rate (eGFR) and albuminuria are established markers in identifying CKD or kidney damage [2, 3]. CKD is defined as a reduced GFR, increased urinary albumin excretion, or both, and is an increasing public health issue [4]. Studies have found CKD to be associated with an increase in cardiovascular disease risk and worse cognitive performance [5, 6]. Both CKD and dementia share similar risk factor profiles consisting of hypertension, diabetes mellitus, stroke, myocardial infarction, and hyperlipidemia [1, 7]. However, the association between CKD and dementia remains unclear [8]. The kidneys and the brain are susceptible to vascular damage as they are exposed to high-volume blood flow. Epidemiological studies have found albuminuria and low GFR associated with Alzheimer disease (AD) and Vascular dementia (VaD) [9, 10]. However, findings have been mixed, where adverse and no associations have been published [11,12,13,14].
An early risk marker of renal endothelial dysfunction is known as moderately increased albuminuria [formerly called microalbuminuria (MA)]. MA is a term to describe moderate amounts of albumin present in the urine, and studies have shown it to be an early risk marker of cardiovascular disease [15]. The importance of MA in cardiovascular disease has been validated, and although it is uncertain, a vascular mechanism is presumably shared by both the kidney and brain and has been suggested as the cause of any shown association [16].
The aim of this study was to evaluate the association between MA using albumin creatinine ratio (ACR) at baseline and the risk for incident AD, VaD and a mixture of these in a prospective study in a population-based cohort. In addition, we examined eGFR, to see if associations differed across samples in the varying stages of CKD.
Methods
Study population
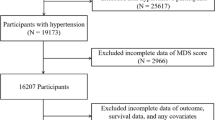
The general health survey known as HUNT 2 (1995–1997) invited all residents ≥20 years (N = 93,898) residing in Nord-Trøndelag County, Norway (see Fig. 1a). Data were collected using questionnaires, clinical measurements and collection of blood and urine samples, and 64,978 (69.2%) residents participated. The details of the HUNT study design have been published previously [17]. Participants who emigrated out of the County (n = 214), lacked a dementia diagnosis date (n = 108), diagnosed with prevalent mild cognitive impairment (MCI) (n = 48), or those who did not provide both clinical examination and self-reported questions on hypertension, diabetes mellitus (DM), stroke, smoking habits, alcohol consumption, and physical activity were removed from the sample (n = 9602). A total of 55,006 participated in both questionnaires and clinical examinations, however, a further 6498 participants were removed due to missing covariate data, resulting in 48,508 participants included in the present study examining the association between CKD and dementia. 668 participants were diagnosed with dementia and 47,840 were not diagnosed with dementia.
Flow chart indicating the number of invited participants and selection criteria from the (a) HUNT 2 study, and (b) the MA substudy. Abbreviations: Q1 HUNT 2 self-report questionnaire one, Q2 HUNT 2 self-report questionnaire two, BLM HUNT 2 data on blood samples and standardized health screenings, MCI mild cognitive impairment, MA moderately increased albuminuria, DM diabetes mellitus, HTN hypertension, ACR albumin creatinine ratio, UTI urinary tract infection
MA substudy
Participants of HUNT 2 who self-reported DM and/or treated hypertension (HTN), and a randomly selected, non-diabetic/non-treated hypertensive sample were included in MA screening, and asked to deliver three urine samples from three consecutive days. Details of the MA screening have been published [15]. The flow chart in Fig. 1b shows identical selection and inclusion criteria for both CKD and MA, where participants lacking either questionnaires, clinical examination, or relevant data on dementia diagnosis were excluded (n = 809). A further 46 did not deliver all three urine samples, 246 had an ACR over 30 mmol/L, and 332 were removed from the sample, as participants confirmed self-reported history of hematuria, menstruation, or pregnancy. 8387 remained in the sample and 1363 had missing covariate data and were removed. 7024 participants had complete data and encompass this study sample. Subgroups were created to examine those diagnosed with dementia and DM or treated for HTN (n = 184) and those diagnosed with dementia and without DM or treatment for HTN (n = 30). Similarly, 5135 participants without dementia and with DM or treatment for HTN, and 1675 controls were without DM and were not treated for HTN.
Clinical examination and laboratory procedures
In HUNT 2, the clinical examination was conducted in survey stations. Height and weight was used to generate body mass index (BMI) based on participants wearing light clothes without shoes: height to the nearest centimeter and weight to the nearest half kilogram. Pulse, systolic (SBP) and diastolic blood pressure (DBP) were measured three times using a Dinamap 845XT (Critikon) based on oscillometry. Non-fasting blood sampling occurred at survey stations during HUNT 2. Fresh serum samples were analyzed using Hitachi 91 Autoanalyser (Hitachi, Mito, Japan) and described in detail previously [18]. Serum concentration of creatinine was used to calculate eGFR using the Chronic Kidney Disease Epidemiology Collaboration equation (CKD-EPI). Further description of examination and laboratory procedures have been described in detail according to standardized protocols [17].
Dementia ascertainment
A parallel study, known as the health and memory study (HMS) of Nord Trøndelag County, took place from 1995 to 2011. The HMS study is a registry of persons diagnosed with dementia in the county from hospital memory clinics between 1995 and 2010; or from nursing home ascertainments performed in 2010–2011. Dementia ascertainment was uniform amongst hospital and nursing home panels. Ascertainment was based on clinical examination, patient, caregiver history, and diagnostic imaging. The ICD-10 classification system was thereafter applied for diagnoses of AD, VaD, a mixture of AD and VaD. Other dementias refers to patients with frontotemporal dementia (FTD), dementia of Lewy bodies (LBD), and unspecified. Establishing the date of the diagnosis of dementia was determined by a panel of specialists in geriatric medicine and psychiatry in the two hospitals or by asking nursing home staff or next of kin the number of months residents of nursing homes had displayed symptoms of memory loss. Details of this cohort have been previously published [19].
Urine sampling
Participants of the MA screening received a unit with three plastic receptacles for three first morning urine samples, three transport tubes, and pre-paid return envelopes addressed to the laboratory. Written instructions provided information how to collect the sample. Participants responded to specific questions pertaining to history of a urinary tract infection during the last week, persistent hematuria over the last year, and whether women were pregnant or menstruating at collection time. Fresh urine samples were analyzed using Hitachi 91 Autoanalyser (Hitachi, Mito, Japan). Urine albumin and creatinine were measured by an immunoturbimetric method (antihuman serum albumin from Dako Norway, Oslo) and Jaffe method [15].
Follow-up and endpoints
The national identification number of every Norwegian inhabitant enables linkage between the Death Registry at Statistics Norway to determine vital status (alive, emigrated, and dead). Each participant contributed in person-years from the date of study entry until the date of death, date diagnosed with dementia or controls who survived to the end of the study (April 23rd, 2011).
Data analysis
First, we analyzed the association between eGFR and dementia and its subtypes AD, VaD, mixed AD/VaD, and other dementia. The Cox proportional hazards model was used to calculate age-and multivariate-adjusted hazard ratios (HRs) with 95% confidence interval (CI) for dementia according to declining eGFR, examined both continuously and using the following categorical cutoffs with eGFR: > 90, 60–89.9, 30–59.9, and < 30. Repeated analyses using the Cox proportional hazards model were performed for ACR. ACR was calculated using the mean of three ACRs and was log transformed when used as a continuous variable in analyses. ACR was also examined categorically as quartiles: 0–.53, .54–.87, .88–1.77, and ≥ 1.78 mg/mmol. Participants’ age was used as a continuous variable in analyses. Level of education was categorized according to primary (seven years or less), secondary (seven to nine years), and upper secondary education (> 10 years). SBP and DBP were calculated as the mean of the second, third of three measurements, and used as continuous variables in analyses. Non-fasting glucose, cholesterol, and iron were scored as continuous variables. Self- report data on history of myocardial infarction (MI), angina, stroke, DM, and smoking were dichotomous variables, and subjective health status was used in analyses categorically according to poor, not so good, good, and very good. The independent-samples t-test and Pearson’s chi squared were used to compare the means between groups for continuous and categorical variables. Four sets of hazard regression models were performed for each endpoint in a hierarchy. Effect modification was examined by testing the age and sex multiplied with both eGFR and log transformed ACR in multi-adjusted models. Finally, supplementary analyses were performed to examine the assumption that lower levels of eGFR comes an increased risk of dying, and death as a competing risk. Competing risk regression was examined with Fine-Gray models using proportional subdistribution hazards (SHs) with 95% CI in models. SPSS Version 25 Software performed analyses shown in Tables 2 and 4. STATA version 14 performed supplementary analyses shown in supplementary material 3.
Results
eGFR
During the study period, 7606 died and 668 developed dementia. The mean age of the study sample was 49.5 ± 16.7 years, and mean eGFR was 78.8 ± 16.2 ml/min/1.73 m2. Persons diagnosed with dementia were older, with reduced eGFR, higher SBP and DBP, and higher prevalence of self-reported cardiovascular disease. Additional characteristics of this sample are shown in Table 1. There was no statistically significant association between eGFR and dementia or its subgroups when examined in hazard regression models, see Table 2. There were interactions between age and eGFR in dementia and its subgroups. Splitting the sample at median age < 72.1; > 72.2, did not change the results in either samples. An age interaction was observed in VaD, however did not provide supportive evidence of any association when examining women and men separately (data not shown). Supplementary analyses with competing risk regression were performed to assess the effect of death on the association between eGFR and dementia, and are shown in Additional file 3. The proportional assumption for the Fine-Gray model was met by testing for time-by-status interaction in the multivariate analysis.
MA substudy
Study participants with a history of DM or using HTN medication, along with participants that did not have a history of DM or treated with HTN medication were examined both combined and in separate analyses. Characteristics are shown in Table 3 for the combined sample, and according to subgroups: DM or HTN and No DM or HTN, see Additional files 1 and 2. Mean ACR did not differ across quartiles of the total sample, and persons diagnosed with dementia were older, had higher SBP, DBP, lower renal function, and higher cholesterol. Table 4 shows the results of age and multivariate-adjusted analyses at different ACR levels expressed in quartiles. We found a positive association between increasing ACR and Combined AD and VaD. ACR in the fourth quartile (> 1.78 mg/mmol) with increased HR of VaD, 3.97 (1.12 to 14.07), compared with ACR in the first quartile (<.53 mg/mmol). In crude analyses, there were no sex interactions or age interactions between ACR and total dementia, combined AD/VaD, Mixed AD/VaD, and VaD.
Discussion
The main finding of this study was that VaD and AD was positively associated with MA, expressed as ACR, in participants under 72 years of age, amongst a treated hypertensive or diagnosed with DM sample. However, despite having a study period of up to 16 years in this large population sample, we found no increased risk of dementia with decreasing eGFR regardless of DM, HTN or no illness status. Our findings contribute to a number of studies examining the association between dementia and renal disease, using ACR and eGFR as markers [11, 20,21,22,23]. Our Norwegian study contrasts with one of the first prospective studies that was performed by Miwa et al. examining 660 Japanese subjects that found an association between eGFR and incident dementia [24]. This contrasting finding could be attributed to different study populations as our study subjects had lower vascular risk compared with the Japanese subjects. Our study supports findings from the 3C Study, where eGFR values were not associated with an increased risk of incident dementia or cognitive decline over the seven-year follow-up11. Although our study featured a long follow-up, we also had a relatively low percentage of participants with eGFR < 60 ml/min). Another prospective study by Tamura et al. also found no significant association between cognitive impairment and risk for progression of CKD [25].
MA is a known pre-cursor for progressive renal damage, diabetic nephropathy, and has been reported to occur in approximately 15–30% of hypertensive patients [15, 26, 27]. There are few studies that have examined the association between MA and dementia, as most studies have data reporting on severely increased albuminuria, defined with ACR > 30 mg/mmol. A recent comparative prospective community-based cohort study has revealed a significant association between albuminuria and risk for development of AD and VaD. Furthermore, a recent systematic review and meta-analyses has concluded that albuminuria was independently associated with cognitive impairment, dementia and cognitive decline [8]. Georgakis et al. showed stronger effects for vascular dementia and cognitive performance in areas primarily affected by microvascular disease and concluded to support the association could be mediated by shared microvascular pathology in the kidney and the brain [28].
Although pathophysiological mechanisms are largely unknown, there are many hypotheses describing possible mechanisms [29, 30]. Nitric oxide (NO) deficiency regulates the microcirculation and blood brain barrier. Patients with impaired cognition show elevated levels of endogenous inhibitors of NO synthesis and decreased NO metabolites, presumably a result of CKD [31]. Strain vessel hypothesis is another presumed mechanism that vessels are exposed to very high pressure, and maintain a high vascular tone. These strained vessels are recognized to share similar pressure-induced injuries, where MA is speculated to be a marker of cerebrovascular-renal injury [3, 32]. These two end organs share similar anatomic and hemodynamic features and vessels are shown to undergo similar mechanisms responding to vascular strain [33]. Juxtamedullary afferent arterioles in the kidney and perforating arterioles in the brain are downstream from high-pressure arteries, and both organs are vulnerable to hypertensive vascular damage [34]. Cerebro-renal interactions are presumed to exist as clinical studies have found a higher prevalence of vascular cognitive impairment in participants with reduced kidney function [24, 34, 35]. Microvascular damage has shown to alter the hemodynamics of the neurovasculature that contributes to cognitive changes seen in the early stages of dementia [35, 36]. Small vessel disease in the kidney may therefore also indicate the presence of small vessel disease in the brain [24, 33, 37].
This study adjusted the effects of MA for eGFR, which is seldom in previously published studies. Participants diagnosed with dementia were an average of 77 years of age when diagnosed with dementia. Despite this relatively young age, MA is still a risk factor for developing dementia. The majority of participants were treated HTN subjects and/or with DM along with a random sample without DM and were not treated with HTN medication. The population-based approach and high attendance rate make selection bias less likely. MA analyses were performed with fresh urine samples without long-term storage, and used data from an average of three urine samples.
This study has limitations. Competing risk from death and other causes is an unavoidable limitation in studies examining participants with older age. Furthermore, older aged participants with lower eGFR are at higher risk of mortality than participants with higher eGFR are, and may therefore never develop incident dementia. Results show that the hazards are identical between groups for dementia, and both the CHR and SHR models estimate the effects as null, as expected. This study did not have access to the national prescription register that provides specific details on types of medication taken by participants. Therefore, data used in analyses was based on self-reported history. As mentioned, the number of participants with CKD was low, as only 12.2% had eGFR < 60 mL. In addition, ACR was measured only in a subsample of the HUNT 2 sample. Experienced clinicians used standardized ICD-10 criteria to ascertain the subtypes of dementia diagnoses, but this was retrospective and based on comprehensive medical records from both hospital and nursing home panels. Data inspection revealed that the period during study startup in 1995–2000 showed infrequent numbers of dementia cases. A greater number of dementia cases were diagnosed during 2000–2009, and the greatest amount of cases with dementia were identified in 2009–2011. Additionally, cognition assessment was not a standard evaluation during HUNT 2 at baseline, and one must note that there was no access to data from individuals with dementia who were under the care of their general practitioner, and these will appear as false-negatives in the data set. It is uncertain if this would influence the results substantially, but unlikely as the proportion of false negative is quite low because the prevalence of dementia is low.
Conclusion
Our results strengthens the hypothesis that vascular mechanisms may affect both kidney and brain as an association between MA, VaD, and Combined AD/VaD was found. However, eGFR was not significantly associated with dementia independent of DM or HTN.
Availability of data and materials
The funding institutions are currently granted the exclusive privilege to perform studies on data derived from the HMS Study. Future collaboration with researchers outside the current research group will be welcomed later. Information about application procedures is available at hunt@medisin.ntnu.no.
Abbreviations
- ACR:
-
Albumin creatinine ratio
- AD:
-
Alzheimer disease;
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- CHR:
-
Cause specific hazard ratio
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- CKD-EPI:
-
Chronic Kidney Disease Epidemiology Collaboration
- DBP:
-
Diastolic blood pressure
- DM:
-
Diabetes mellitus
- eGFR:
-
Estimated glomerular filtration rate
- FTD:
-
Frontal temporal dementia
- HMS:
-
Health and Memory Study of Nord-Trøndelag County
- HR:
-
Hazard ratio
- HTN:
-
Hypertension
- HUNT:
-
The Health Study of Nord-Trøndelag
- ICD-10:
-
International classification of diseases
- LBD:
-
Lewy body dementia
- MA:
-
Moderately increased albuminuria
- MCI:
-
Mild cognitive impairment
- MI:
-
Myocardial infarction
- Mixed AD/VaD:
-
Mixed Alzheimer’s Disease/vascular dementia
- NO:
-
Nitric oxide
- NTNU:
-
Norwegian University of Science and Technology
- REK:
-
Regional Committee for Medical and Health Research Ethics
- SBP:
-
Systolic blood pressure
- SH:
-
Subdistribution hazard
- SHR:
-
Subdistribution hazard ratio
- SPSS:
-
Statistical Package for the Social Sciences
- VaD:
-
Vascular dementia
References
Livingston G, Sommerlad A, Orgeta V, et al. Dementia prevention, intervention, and care. Lancet. 2017;390(10113):2673–734.
Hill NR, Fatoba ST, Oke JL, et al. Global prevalence of chronic kidney disease - a systematic review and meta-analysis. PLoS One. 2016;11(7):e0158765.
Nagasawa T, Mori T, Ohsaki Y, et al. Albuminuria indicates the pressure-associated injury of juxtamedullary nephrons and cerebral strain vessels in spontaneously hypertensive stroke-prone rats. Hypertens Res. 2012;35(10):1024–31.
Jha V, Garcia-Garcia G, Iseki K, et al. Chronic kidney disease: global dimension and perspectives. Lancet. 2013;382(9888):260–72.
Kurella Tamura M, Yaffe K. Dementia and cognitive impairment in ESRD: diagnostic and therapeutic strategies. Kidney Int. 2011;79(1):14–22.
Weiner DE, Gaussoin SA, Nord J, et al. Cognitive function and kidney disease: baseline data from the systolic blood pressure intervention trial (SPRINT). Am J kidney Dis. 2017;70(3):357–67.
Zammit AR, Katz MJ, Bitzer M, Lipton RB. Cognitive impairment and dementia in older adults with chronic kidney disease: a review. Alzheimer Dis Assoc Disord. 2016;30(4):357–66.
Deckers K, Camerino I, van Boxtel MP, et al. Dementia risk in renal dysfunction: a systematic review and meta-analysis of prospective studies. Neurology. 2017;88(2):198–208.
Barzilay JI, Gao P, O'Donnell M, et al. Albuminuria and decline in cognitive function: the ONTARGET/TRANSCEND studies. Arch Intern Med. 2011;171(2):142–50.
Takae K, Hata J, Ohara T, et al. Albuminuria increases the risks for both Alzheimer disease and vascular dementia in community-dwelling Japanese elderly: the Hisayama study. J Am Heart Assoc. 2018;7(2):e006693.
Helmer C, Stengel B, Metzger M, et al. Chronic kidney disease, cognitive decline, and incident dementia: the 3C study. Neurology. 2011;77(23):2043–51.
Sundelof J, Arnlov J, Ingelsson E, et al. Serum cystatin C and the risk of Alzheimer disease in elderly men. Neurology. 2008;71(14):1072–9.
Seliger SL, Wendell CR, Waldstein SR, Ferrucci L, Zonderman AB. Renal function and long-term decline in cognitive function: the Baltimore longitudinal study of aging. Am J Nephrol. 2015;41(4–5):305–12.
Seliger SL, Siscovick DS, Stehman-Breen CO, et al. Moderate renal impairment and risk of dementia among older adults: the cardiovascular health cognition study. J Am Soc Nephrol. 2004;15(7):1904–11.
Hallan H, Romundstad S, Kvenild K, Holmen J. Microalbuminuria in diabetic and hypertensive patients and the general population--consequences of various diagnostic criteria--the Nord-Trondelag health study (HUNT). Scand J Urol Nephrol. 2003;37(2):151–8.
Knopman DS. Invited commentary: albuminuria and microvascular disease of the brain--a shared pathophysiology. Am J Epidemiol. 2010;171(3):287–9 author reply 90-1.
Krokstad S, Langhammer A, Hveem K, et al. Cohort profile: the HUNT study. Int J Epidemiol. 2012;42(4):968–77.
Holmen J, Midthjell K, Krüger Ø, et al. The Nord-Trøndelag health study 1995-97 (HUNT 2): objectives, contents, methods and participation. Norsk Epidemiologi. 2003;13(1):19–32.
Bergh S, Holmen J, Gabin J, et al. Cohort profile: the health and memory study (HMS): a dementia cohort linked to the HUNT study in Norway. Int J Epidemiol. 2014;43(6):1759–68.
Prinz N, Stingl J, Dapp A, et al. High rate of hypoglycemia in 6770 type 2 diabetes patients with comorbid dementia: a multicenter cohort study on 215,932 patients from the German/Austrian diabetes registry. Diabetes Res Clin Pract. 2016;112:73–81.
Higuchi M, Chen R, Abbott RD, et al. Mid-life proteinuria and late-life cognitive function and dementia in elderly men: the Honolulu-Asia aging study. Alzheimer Dis Assoc Disord. 2015;29(3):200–5.
O'Hare AM, Walker R, Haneuse S, et al. Relationship between longitudinal measures of renal function and onset of dementia in a community cohort of older adults. J Am Geriatr Soc. 2012;60(12):2215–22.
Barzilay JI, Fitzpatrick AL, Luchsinger J, et al. Albuminuria and dementia in the elderly: a community study. Am J Kidney Dis. 2008;52(2):216–26.
Miwa K, Tanaka M, Okazaki S, et al. Chronic kidney disease is associated with dementia independent of cerebral small-vessel disease. Neurology. 2014;82(12):1051–7.
Kurella Tamura M, Yaffe K, Hsu CY, et al. Cognitive impairment and progression of CKD. Am J kidney Dis. 2016;68(1):77–83.
Murai S, Tanaka S, Dohi Y, Kimura G, Ohte N. The prevalence, characteristics, and clinical significance of abnormal albuminuria in patients with hypertension. Sci Rep. 2014;4:3884.
Schrader J, Luders S, Kulschewski A, et al. Microalbuminuria and tubular proteinuria as risk predictors of cardiovascular morbidity and mortality in essential hypertension: final results of a prospective long-term study (MARPLE study)*. J Hypertens. 2006;24(3):541–8.
Georgakis MK, Dimitriou NG, Karalexi MA, et al. Albuminuria in association with cognitive function and dementia: a systematic review and meta-analysis. J Am Geriatr Soc. 2017;65(6):1190–8.
Arvanitakis Z, Capuano AW, Leurgans SE, Bennett DA, Schneider JA. Relation of cerebral vessel disease to Alzheimer's disease dementia and cognitive function in elderly people: a cross-sectional study. Lancet Neurol. 2016;15(9):934–43.
Gorelick PB, Scuteri A, Black SE, et al. Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the american heart association/american stroke association. Stroke. 2011;42(9):2672–713.
Baylis C. Nitric oxide synthase derangements and hypertension in kidney disease. Curr Opin Nephrol Hypertens. 2012;21(1):1–6.
Ito S. Cardiorenal connection in chronic kidney disease. Clin Exp Nephrol. 2012;16(1):8–16.
Mogi M, Horiuchi M. Clinical interaction between brain and kidney in small vessel disease. Cardiol Res Pract. 2011;2011:306189.
Yao H, Araki Y, Takashima Y, Uchino A, Yuzuriha T, Hashimoto M. Chronic kidney disease and subclinical brain infarction increase the risk of vascular cognitive impairment: the Sefuri study. J Stroke Cerebrovasc Dis. 2017;26(2):420–4.
Kurella Tamura M, Wadley V, Yaffe K, et al. Kidney function and cognitive impairment in US adults: the reasons for geographic and racial differences in stroke (REGARDS) study. Am J Kidney Dis. 2008;52(2):227–34.
Stefani A, Sancesario G, Pierantozzi M, et al. CSF biomarkers, impairment of cerebral hemodynamics and degree of cognitive decline in Alzheimer's and mixed dementia. J Neurol Sci. 2009;283(1–2):109–15.
Toyoda K. Cerebral small vessel disease and chronic kidney disease. J Stroke. 2015;17(1):31–7.
Acknowledgements
We thank the HUNT-HMS study participants and their caregivers.
Funding
Extrastiftelsen and the Norwegian Health Association are the funding sources of the present study, and had no other role in this study. The corresponding author had full access to all data in the study and had final responsibility for the decision to submit for publication. The HUNT Study is a collaborative effort of the Faculty of Medicine and Health Sciences at the Norwegian University of Science and Technology (NTNU), the Norwegian Institute of Public Health, the Nord-Trøndelag County Council, and the Central Norwegian Regional Health Authority. The Norwegian Institute of Public Health, NTNU, Nord-Trøndelag Hospital Trust, and Innlandet Hospital Trust funded the HMS Study.
Author information
Authors and Affiliations
Contributions
JH, IS designed the HMS Study, and JH was principal investigator of the HUNT 2 Study. SR was the principal investigator of the MA sub-study during HUNT 2 and co-authored the present manuscript. JH led data collection of the HMS study, IS oversaw the dementia panel. JMG analyzed the patient data, interpreted the data and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval for this study was obtained from the Regional Committee for Medical and Health Research Ethics (REK) in Mid-Norway (reference number 2011/1793). Participation in the HUNT Study was voluntary and written consent was acquired. The HMS Study extracted hospital diagnoses retrospectively, and obtaining informed consent was not possible. However, study design was approved from the Regional Committee for Medical and Health Research Ethics in Mid-Norway. The nursing home residents provided written consent, which was obtained from patients prior to the data collection. In cases where residents lacked mental capacity to consent (evaluated by nurses in 62% of cases), residents’ next of kin were contacted, and issued written consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Characteristics of subsample study examining albumin creatinine ratio amongst participants who self-reported history of diabetes mellitus or taking anti-hypertensive medication. (DOCX 21 kb)
Additional file 2:
Characteristics of subsample study examining albumin creatinine ratio amongst participants who self-reported no history of diabetes mellitus or did not report taking anti-hypertensive medication. (DOCX 30 kb)
Additional file 3:
Estimated cause specific hazard (CHR) and subdistribution hazard ratios (SHR) for death and dementia using multivariate regression model. Cox regression cause specific hazards (CHR) and Fine-Gray subdistribution hazards (SHR) are shown with 95% CI. (DOCX 28 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Gabin, J.M., Romundstad, S., Saltvedt, I. et al. Moderately increased albuminuria, chronic kidney disease and incident dementia: the HUNT study. BMC Nephrol 20, 261 (2019). https://doi.org/10.1186/s12882-019-1425-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12882-019-1425-8