Abstract
Background
In December 2019, the outbreak of coronavirus disease 2019 (COVID-19) began in Wuhan, China, and rapidly spread to other regions. We aimed to further describe the epidemiological and clinical characteristics of discharged COVID-19 cases and evaluate the public health interventions.
Methods
We collected epidemiological and clinical data of all discharged COVID-19 cases as of 17 February 2020 in Shanghai. The key epidemiological distributions were estimated and outcomes were also compared between patients whose illness were before 24 January and those whose illness were after 24 January.
Results
Of 161 discharged COVID-19 cases, the median age was 45 years, and 80 (49.7%) cases were male. All of the cases were categorized as clinical moderate type. The most common initial symptoms were fever (85.7%), cough (41.0%), fatigue (19.3%), muscle ache (17.4%), sputum production (14.9%), and there were six asymptomatic cases. 39 (24.2%) cases got infected in Shanghai, and three of them were second-generation cases of Shanghai native cases. The estimated median of the time from onset to first medical visit, admission, disease confirmation, and discharge for 161 cases was 1.0 day (95% CI, 0.6–1.2), 2.0 days (95% CI, 1.5–2.6), 5.2 days (95% CI, 4.6–5.7), 18.1 days (95% CI, 17.4–18.8), respectively. The estimated median of the time from admission to discharge was 14.0 days (95% CI, 13.3–14.6). The time from onset to first medical visit, admission and disease confirmation were all shortened after the Shanghai’s first-level public health emergency response. In Cox regression model, the significant independent covariates for the duration of hospitalization were age, the time from onset to admission and the first-level public health emergency response.
Conclusions
Local transmission had occurred in Shanghai in late January 2020. The estimated median of the time from onset to discharge of moderate COVID-19 was 18.1 days in Shanghai. Time intervals from onset to first medical visit, admission and disease confirmation were all shortened after the Shanghai’s first-level public health emergency response. Age, the first-level public health emergency response and the time from onset to admission were the impact factors for the duration of hospitalization.
Similar content being viewed by others
Background
Coronavirus Disease 2019 (COVID-19) is an infectious disease caused by 2019 novel coronavirus (2019-nCoV). The most common signs of infection include fever, respiratory symptoms (such as cough and sputum production) and fatigue [1]. The first COVID-19 case was identified in Wuhan, China in late December 2019 [2]. The COVID-19 has rapidly spread from Wuhan to other areas [3, 4]. As of 17 February 2020, a total of 72,528 COVID-19 cases in China have been confirmed and cases have been reported in 25 countries and 5 continents internationally [5].
To curb the spread of COVID-19, the Shanghai authorities have declared the first-level public health emergency response on 24 January 2020 [6]. The measures included: travelers from Wuhan and other epidemic areas were advised to report their travel records and to conduct self-quarantine for 2 weeks to prevent community transmission; comprehensive implementation of sanitary quarantine at the entrance of Shanghai; cancellation various large public events; masks were recommended to be worn in public places; strengthened publicity of health knowledge, etc. Public health interventions played an important role in controlling the epidemic. As of 17 February, there were a total of 333 confirmed COVID-19 cases in Shanghai and 161 of them had been cured to discharge [7].
Epidemiological and clinical characteristics of 333 confirmed COVID-19 cases in Shanghai have been reported [8]. However, at present, the impact of first-level public health emergency response on the epidemic of COVID-19 was not estimated and information regarding the epidemiology and clinical features of discharged COVID-19 cases is scarce [9,10,11,12]. Therefore, we provided an analysis of key epidemiological determinants and clinical characteristics of 161 discharged COVID-19 cases in Shanghai. Moreover, we described and estimated the time interval from onset to discharge, which might helpful to understanding the progression of the disease.
Methods
Study design and participants
We performed a comprehensive study of all the 161 discharge COVID-19 cases reported in Shanghai in the case reporting system as of 17 February 2020.
Case definition
All cases were tested COVID-19 positive in laboratory and diagnosed by clinical experts according to COVID-19 prevention and control program (4nd ed.) 2020 [13]. The symptom severity of COVID-19 was classified into moderate, severe and critical. Moderate cases refer to those cases who have symptoms such as fever and respiratory tract symptoms, etc. and pneumonia manifestations can be seen in imaging. Severe cases refer to any of the following criteria: (i) respiratory rate ≥ 30 breaths/min, (ii) oxygen saturation ≤ 93% at a rest state, (iii) arterial partial pressure of oxygen (PaO2)/oxygen concentration (FiO2) ≤ 300 mmHg. Critical cases refer to those cases that meeting any of the following criteria: (i) occurrence of respiratory failure requiring mechanical ventilation, (ii) presence of shock, (iii) other organ failure that requires monitoring and treatment in the ICU. The criteria of discharge included: (i) body temperature returned to normal (< 37.3 °C) for more than 3 days, (ii) respiratory symptoms improved significantly, (iii) rRT-PCR of 2019-nCoV was negative for two consecutive times (sampling interval at least 1 day).
Data collection
After cases were reported to Shanghai Municipal Centers for Disease Control and Prevention (CDC), epidemiological investigations were conducted within 2 h. Demographic data, clinical symptoms or signs, laboratory tests during hospital admission, comorbidities, exposure history in 14 days and prevention and control measures were all collected. When cases were discharged, clinical records of discharge were also collected. The Specific information in epidemiological investigation was entered into a computerized database of Epidata software (Epidata Association) in duplicate. The data were analyzed anonymously.
Laboratory testing
The 2019-nCoV laboratory test assays were based on the Technical Guidelines for Laboratory Testing of Novel Coronavirus Pneumonia [13]. Upper or lower respiratory specimens of suspected COVID-19 cases were collected and tested for 2019-nCoV by real-time reverse-transcriptase polymerase chain reaction (rRT-PCR) assay. Tests were carried out in biosafety level two facilities at district CDCs or Municipal CDC. The case was considered as laboratory tested positive only when two targets, open reading frame 1a or 1b (ORF1ab) and nucleocapsid protein (N), were both positive.
ORF1ab:
-
Forward primer CCCTGTGGGTTTTACACTTAA;
-
Reverse primer ACGATTGTGCATCAGCTGA;
-
Probe 5′-VIC-CCGTCTGCGGTATGTGGAAAGGTTATGG-BHQ1–3′.
N:
-
Forward primer GGGGAACTTCTCCTGCTAGAAT;
-
Reverse primer CAGACATTTTGCTCTCAAGCTG;
-
Probe 5′-FAM- TTGCTGCTGCTTGACAGATT-TAMRA-3′.
Key points in epidemiology
The Shanghai authorities have activated the first-level public health emergency response to curb the spread of COVID-19 on 24 January. So cases were divided into two groups (illness onset during 3 Jan to 24 Jan, illness onset during 25 Jan to 17 Feb). Estimated median intervals of onset to first medical visit, onset to admission, onset to disease confirmation, admission to discharge, and onset to discharge were obtained for the two groups, assuming that the times were γ distributed.
Statistical analysis
We present continuous variables as medians (interquartile ranges, IQR) and compared using Wilcoxon rank-sum tests between different groups. Categorical variables were described as counts and percentages in each category, and compared using chi-square or Fisher’s exact tests between different groups. Time-delay distributions (onset to first medical visit, onset to admission, onset to disease confirmation, admission to discharge, and onset to discharge) were fitted to γ distributions by maximum likelihood estimation methods. Cox regression model was used to identify factors significantly associated with the duration of COVID-19 hospitalization. These factors included: age, gender, hightest temperature, place of infection, smoking, drinking, body mass index, white blood cell count, neutrophil count, lymphocyte count, comorbidies, time from onset to admission and first-level public health emergency response.
Analyses of the time-delay distributions were performed with R software (R Foundation for Statistical Computing). Other analyses were performed with SPSS (Statistical Package for the Social Sciences) version 16.0 software (SPSS Inc).
Results
Demographic and clinical characteristics
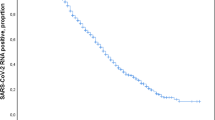
As of 17 February 2020, 161 confirmed COVID-19 cases had been discharged in Shanghai. The first cured case was discharged on 24 January 2020 (Fig. 1). The median age was 45 years (IQR, 34–61; range, 1–84), and four (2.5%) were younger than 15 years. 80 (49.7%) cases were male. 39 (24.2%) cases got infected in Shanghai, and three of them were second-generation cases of Shanghai native cases (Table 1).
On admission, 161 were all categorized as moderate severity. The most common reported initial symptoms at illness onset were fever (138 [85.7%]) (the median highest temperature, 38.0 °C; IQR, 37.7–38.5), cough (66 [41.0%]), fatigue (31 [19.3%]), muscle ache (28 [17.4%]), sputum production (24 [14.9%]). Less common symptoms were vomit (3 [1.9%]), dyspnea (3 [1.9%]), diarrhea (5 [3.1%]) (Table 2). 107 (66.5%) cases reported fever plus any one other symptom, and 66 (41.0%) cases reported fever plus two other symptoms. 46 (28.6%) cases had one or more basic diseases, 27 (16.8%) cases had hypertension, 12 (7.5%) cases had cardiovascular diseases, 9 (5.6%) cases had diabetes.
Of 161 cases, the median white blood cell counts was 5.0 × 109/L (IQR, 3.8–6.2), the median neutrophil cell counts was 3.0 × 109/L (IQR, 2.3–6.2), the median lymphocyte cell counts was 3.0 × 109/L (IQR, 2.3–6.2).
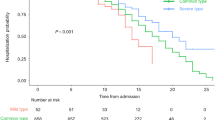
Key points in epidemiology
The time from onset to discharge for 161 cases ranged from 7 to 34 days. The estimated median of the time from onset to discharge was 18.1 days (95% CI, 17.4–18.8) (Table 3). The estimated median of the time from onset to discharge for 75 cases who had onset symptoms before 24 January was 20.5 days (95% CI, 19.5–21.5), which was significantly longer than 86 cases with illness onset after 24 January, having a median of 16.2 days (95% CI, 15.4–17.0) (p < 0.001) (Fig. 2).
The estimated median of the time from onset to first medical visit for 161 cases was 1.0 day (95% CI, 0.6–1.2). The estimated median of the time from onset to first medical visit for the 75 cases was 1.7 days (95% CI, 1.1–2.5), which was significantly longer than the 86 cases with a median of 0.6 days (95% CI, 0.3–0.8) (p < 0.001).
The estimated median of the time from onset to admission for 161 cases was 2.0 days (95% CI, 1.5–2.6). The estimated median of the time from onset to admission for the 75 cases was 3.7 days (95% CI, 2.8–5.2), which was significantly longer than the 86 cases with a median of 1.1 days (95% CI, 0.6–1.5) (p < 0.001).
The estimated median of the time from onset to disease confirmation for 161 cases was 5.2 days (95% CI, 4.6–5.7). The estimated median of the time from onset to disease confirmation for the 75 cases was 7.3 days (95% CI, 6.3–8.2), which was significantly longer than the 86 cases with a median of 3.7 days (95% CI, 3.2–4.2) (p < 0.001).
The estimated median of the time from admission to discharge for 161 cases was 14.0 days (95% CI, 13.3–14.6). The estimated median of the time from admission to discharge for the 75 cases was 14.4 days (95% CI, 13.3–15.4), which was similar to the 86 cases with a median of 13.7 days (95% CI, 12.9–14.4) (p = 0.19).
Duration of onset to discharge and hospitalization analysis
In Cox regression model, we used discharge as the outcome variable (Tables 4 and 5). For all 161 cases, the significant independent covariates for the duration of onset to discharge were age, the time from onset to admission and the first-level public health emergency response. The significant independent covariates for the duration of hospitalization were age, the time from onset to admission and the first-level public health emergency response (Fig. 3). Potential influence which did not apparently impact duration of hospitalization was gender.
Discussion
As far as we know, this research includes the largest discharged COVID-19 case series and report an initial evaluation of the epidemiological characteristics, clinical characteristics, laboratory results, and disease course of COVID-19 cases. As of 17 February 2020, a total of 333 COVID-19 cases in Shanghai had been confirmed, of which 161 (48.3%) cases had been cured and discharged. Among them, one (0.3%) case died, and case fatality rate is consistent with national (except Hubei) [14, 15].
Among 161 discharged cases, 75.8% cases were imported to Shanghai after infection in other provinces, mainly in Hubei (65.22%). Three of them were second-generation cases of Shanghai native cases, the onset of which was late January, indicating that local transmission had occurred in Shanghai in late January. The range age of the cases was 1 to 84 years, indicating that all age groups are susceptible to the 2019-nCoV.
Common symptoms at onset of illness were fever, dry cough and fatigue. However, a significant proportion of cases presented initially with atypical symptoms, such as vomit, diarrhea and dyspnea. There were a certain proportion (14.4%) of cases without fever, if screening is focused on the detection of fever, some cases may be missed. The study found that there were six asymptomatic cases of COVID-19, which indicates that asymptomatic infections or pre-symptomatic infections is possible. The asymptomatic infections make it difficult to recognize illness and difficult to quickly and effectively isolate asymptomatic and pre-symptomatic cases, increasing the effective infectious period and the risk for transmission.
In Nanshan Chen et al. study [11], mainly in moderate patients infected with 2019-nCoV, 35% of patients had lymphocytopenia, and lymphocytopenia occurred in more than 80% of critically ill patients in Xiaobo Yang et al. study [9], indicating that the severity of lymphocytopenia reflects the severity of 2019-nCoV infection. Lymphocytopenia occurred in more than 40% of cases in our study. In the Cox regression model, the lower the lymphocyte count, the longer the duration of hospitalization, but there is no statistical significance, our sample size may be limited to finding a statistical significance.
The estimated median of the time from onset to the first medical visit, admission, disease confirmation was 1 day, 2 days and 5.2 days, respectively. After first-level public health emergency response, the time were reduced to 0.6 days, 1.1 days, and 3.7 days, respectively, which was significantly shorter than that before first-level public health emergency response (1.7 days, 3.7 days, and 7.3 days, respectively). This indicates that the early identification, isolation and confirmation of cases with COVID-19 have been accelerated after the first-level public health emergency response. Shortening the duration of onset to admission does not seem to impact clinical outcomes [16, 17]. However, shortening the duration of onset to admission facilitates quarantine and reduces the risk of transmission, and the effective communicable period. And any additional shortening of the duration that symptomatic cases are in the community will bring about further benefits at the whole crowd level.
Quarantine is a traditional and yet the most effective measure to control an epidemic. Because there is no specific vaccine or cure against 2019-nCoV infections, standard public health emergency measures usually prove most efficient, including isolating the sources of infection, interrupting or cutting off transmission routes, and special care for the most susceptible people. And the COVID-19 epidemic has shown that the essential for risk disclosure that will warn and inform the citizens, in such a way that will enhance personal protection, without triggering raised fear and anxiety, as an essential part of COVID-19 epidemic control. A change in disease risk awareness would potentially bring about an increase in early reporting of COVID-19.
Cox regression analysis showed that the elder the case, the longer the duration of hospitalization. The possible explanations were that the younger case has higher recovery ability after infection with 2019-nCoV, and the elder case has a higher proportion of comorbidities. We review previous studies that found a greater number of male than female [11, 18, 19], but our research shows that there was no significant difference in the course of disease between male and female. After first-level public health emergency response, the duration of hospitalization was shorter. Shortening the time from initial symptoms to admission does not decrease the duration of hospitalization for moderate COVID-19 cases. More generally, the average time from onset to discharge was 19 days. One reason may be that there is no specific cure or vaccine against 2019-nCoV infections except for meticulous supportive. Another reason may be that it may indicates that moderate COVID-19 is self-limited disease.
This study has several limitations. First, only three of 161 cases had short and defined periods of exposure to known COVID-19 cases, so we did not estimate the distribution of the incubation period, the time from infection to the onset of symptoms of COVID-19. Second, the symptom severity of the discharged cases was moderate pneumonia, so we are unable to estimate severe or critical pneumonia.
Conclusions
In conclusion, local transmission had occurred in Shanghai in late January 2020. The estimated median of the time from onset to discharge of moderate COVID-19 was 18.1 days in Shanghai. Time intervals from onset to first medical visit, admission and disease confirmation were all shortened after Shanghai’s first-level public health emergency response. Age, first-level public health emergency response and the time from onset to admission were the impact factors for the duration of hospitalization. Male and female have the same course of disease.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author (Xiaodong Sun, sunxiaodong_scdc@163.com) on reasonable request.
Abbreviations
- COVID-19:
-
Coronavirus Disease 2019
- 2019-nCoV:
-
2019 novel coronavirus
- CDC:
-
Centers for Disease Control and Prevention
- rRT-PCR:
-
Real-time reverse-transcriptase polymerase chain reaction
References
World Health Organization. Question and answer on coronaviruses (COVID-19). 2020. https://www.who.int/news-room/q-a-detail/q-a-coronaviruses. Accessed 20 Feb 20 2020.
Lu H, Stratton CW, Tang YW. Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle. J Med Virol. 2020;92(4):401–2.
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323:1061.
Hui DS, I Azhar E, Madani TA, Ntoumi F, Kock R, Dar O, Ippolito G, Mchugh TD, Memish ZA, Drosten C, et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health — the latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis. 2020;91:264–6.
World Health Organization. Coronavirus disease 2019 (COVID-19) Situation reports-29. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200218-sitrep-29-covid-19.pdf?sfvrsn=6262de9e_2. Accessed 20 Feb 20 2020.
Shanghai Municipal People’s Government, Shanghai launched a first-level response to resolutely curb the spread of the epidemic. http://www.shanghai.gov.cn/nw2/nw2314/nw32419/nw48516/nw48539/u21aw1423526.html. Accessed 20 Feb 20 2020.
Shanghai Municipal People’s Government, One new confirmed case of COVID-19 in Shanghai. http://www.shanghai.gov.cn/nw2/nw2314/nw32419/nw48516/nw48518/u21aw1426139.html. Accessed 20 Feb 20 2020.
Yu X, Sun X, Cui P, Pan H, Lin S, Han R, Jiang C, Fang Q, Kong D, Zhu Y, et al. Epidemiological and clinical characteristics of 333 confirmed cases with coronavirus disease 2019 in Shanghai, China. TRANSBOUND EMERG DIS. 2020;67(4):1697–707.
Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475.
Xu X, Wu X, Jiang X, Xu K, Ying L, Ma C, Li S, Wang H, Zhang S, Gao H, et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ. 2020;368:m606.
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13.
Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong JY, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199.
National Health Commission of the People’s Republic of China, New coronavirus pneumonia prevention and control program (4nd ed.) (in Chinese). 2020. http://www.nhc.gov.cn/yzygj/s7653p/202001/4294563ed35b43209b31739bd0785e67.shtml. Accessed 20 Feb 20 2020.
Novel Coronavirus Pneumonia Emergency Response Epidemiology T. The epidemiological characteristics of an outbreak of 2019 Novel coronavirus diseases (COVID-19) in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(2):145–51.
Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239.
Donnelly CA, Ghani AC, Leung GM, Hedley AJ, Fraser C, Riley S, Abu-Raddad LJ, Ho L, Thach T, Chau P, et al. Epidemiological determinants of spread of causal agent of severe acute respiratory syndrome in Hong Kong. Lancet. 2003;361(9371):1761–6.
Leung GM, Hedley AJ, Ho LM, Chau P, Wong IO, Thach TQ, Ghani AC, Donnelly CA, Fraser C, Riley S, et al. The epidemiology of severe acute respiratory syndrome in the 2003 Hong Kong epidemic: an analysis of all 1755 patients. Ann Intern Med. 2004;141(9):662–73.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China The Lancet. 2020;395(10223):497–506.
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui D, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708.
Acknowledgments
We thank all medical workers taking part in investigation and treatment of COVID-19 patients in Shanghai.
Funding
This work was support by a grant from Science and Technology Commission Shanghai Municipality Grant/Award Number: 20JC1410200.
Author information
Authors and Affiliations
Contributions
SXD, WHY, PH conceived the study. LS designed the study, analyzed data and wrote manuscript. YX, CP, KDC, HRB, JCY, ZYX, GXH, XWJ, MSH, JBH and ZYY were involved in collecting data and data cleaning. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was reviewed and approved by Shanghai Municipal Center for Disease Control and Prevention Ethics Review Committee, which waived the written informed consent for emerging infectious diseases. The data were analyzed anonymously.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lin, S., Pan, H., Wu, H. et al. Epidemiological and clinical characteristics of 161 discharged cases with coronavirus disease 2019 in Shanghai, China. BMC Infect Dis 20, 780 (2020). https://doi.org/10.1186/s12879-020-05493-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-020-05493-7