Abstract
Background
HIV continues to be the main determinant morbidity with high mortality rates in Sub-Saharan Africa, with a high number of patients being late presenters with advanced HIV. Clinical management of advanced HIV patients is thus complex and requires strict adherence to updated, empirical and simplified guidelines. The current study investigated the impact of the implementation of a new clinical guideline on the management of advanced HIV in Kinshasa, Democratic Republic of Congo (DRC).
Methods
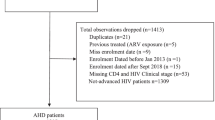
A retrospective analysis of routine clinical data of advanced HIV patients was conducted for the periods; February 2016 to March 2017, before implementation of new guidelines, and November 2017 to July 2018, after the implementation of new guidelines. Eligible patients were patients with CD4 < 200 cell/μl and presenting with at least 1 of 4 opportunistic infections. Patient files were reviewed by a medical doctor and a committee of 3 other doctors for congruence. Statistical significance was set at 0.05%.
Results
Two hundred four and Two hundred thirty-one patients were eligible for inclusion before and after the implementation of new guidelines respectively. Sex and age distributions were similar for both periods, and median CD4 were 36 & 52 cell/μl, before and after the new guidelines implementation, respectively. 40.7% of patients had at least 1 missed/incorrect diagnosis before the new guidelines compared to 30% after new guidelines, p < 0.05. Clinical diagnosis for TB and toxoplasmosis were also much improved after the implementation of new guidelines. In addition, only 63% of patients had CD4 count test results before the new guidelines compared to 99% of patients after new guidelines. Death odds after the implementation of new guidelines were significantly lower than before new guidelines in a multivariate regression model that included patients CD4 count and 10 other covariates, p < 0.05.
Conclusions
Simplification and implementation of a new and improved HIV clinical guideline coupled with the installation of laboratory equipment and point of care tests potentially helped reduce incorrect diagnosis and improve clinical outcomes of patients with advanced HIV. Regulating authorities should consider developing simplified versions of guidelines followed by the provision of basic diagnostic equipment to health centers.
Similar content being viewed by others
Background
Increased access to antiretroviral therapy (ART) has led to an overall decrease in HIV hospitalizations and subsequent mortality. However, mortality rates are still unacceptably high and most low-resourced countries are yet to meet targets set by the Joint United Nations Programme on HIV/AIDS (UNAIDS) back in 2014 [1]. .Compounding the problem is the fact that many patients still present late rendering the treatment of opportunistic infections (OIs) such as tuberculosis (TB), cryptococcal meningitis, Pneumocystis pneumonia (PCP) and non-TB pneumonia clinically complex [2]. The changing dynamics of the HIV epidemic including resistance to antivirals and antibiotics, change in demographic of infected patients, increase in the number of people living with HIV and the advancement of screening and testing techniques, has prompted calls for the review of existing guidelines so that they are comprehendible, accessible and adaptive to specific contexts and settings [3].
While generic guidelines have proven to be generally effective in the management of advanced HIV, reports and studies have shown that clinicians- especially those in resource limited settings- usually struggle to effectively incorporate guidelines into their everyday practice [4]. In countries with high HIV prevalence, algorithms and guidelines have been specifically adapted so that they are apt and responsive to their respective populations [5]. As such, HIV related hospitalizations and mortality in those countries have been on a steady decline [6,7,8]. On the other hand, in low HIV prevalence and low resource settings, most departments and agencies usually rely on the use of external clinical guides and algorithms for the management of HIV patients with OIs [9]. The use of these guidelines usually present a host of issues including mismatch between competencies of clinicians and proposed algorithms, lack of recommended resources, and complexity of language and/or presentation [3]. Therefore, over the years, health ministries, departments and organizations working in low prevalence and low resource settings have been reviewing existing clinical algorithms and guidelines so that they are specific and responsive to their context. As new guidelines are introduced, it is necessary for a review of those guidelines against previous guidelines to assess and measure their effectiveness and limitations in the real world clinical setting.
Why this study?
Médecins Sans Frontières (MSF), with support from its Southern African Medical Unit (SAMU), has been working on reviewing and adapting existing advanced HIV clinical guidelines for use by it partners in low resource settings. These guidelines and algorithms are usually developed and adapted in consultation with other agencies and resources including the World Health Organization (WHO) and health ministries. The ultimate goal is to improve patient management in clinics and hospitals, thereby improving patient health outcomes. From April 2017 to November 2017, MSF-SAMU introduced and implemented a new guideline for use at “Centre Hospitalier De Kabinda” CHK in Kinshasa, Democratic Republic of Congo (DRC). After a successful implementation of the guideline, it was officially published in November, 2017. Both the previous and new guidelines focused on empirical treatment of OIs. However, the new guideline had a number of additions and revisions to help guide clinician decision making and improve patient outcomes. Changes made to the previous guideline included;
-
Compilation of various clinical guideline documents into a single simplified guideline with explanatory texts and scenarios to help with diagnosis
-
Improvement in the language and visual aesthetic of the guideline using images, colour codes, notepads, etc.
-
Clarity in clinical diagnoses for opportunistic infections including clear guidelines and emphasis on empirical treatment
-
Extensive training of clinicians on the new guidelines and support through HIV expert clinician visits from MSF-SAMU.
-
Installation of advanced laboratory and point of care testing packages including GeneXpert®, TB-Mycobacterial Lipoarabinomannan (TB-Lam) and Serum Cryptococcal Antigen (CRAG) tests
-
Periodically testing blood cultures of patients suspected of having OIs at external laboratories in Kinshasa.
The current study was conducted to evaluate the impact of the implementation of new guidelines on the management of patients hospitalized at the CHK in Kinshasa, DRC. In the past, results from routine annual reports showed a steady increase in mortality rates at the CHK from 2015 (24%), 2016 (28%), and the first quarter of 2017 (30%). A mortality audit conducted in July 2017 identified specific gaps in care. Diseases were underdiagnosed, and median times for the initiation of treatments were longer than recommended times. In the months following the implementation of algorithms from the new guidelines, significant decrease in mortality was observed at CHK. Although it would be difficult to determine the exact cause(s) for a change in mortality frequency using this study, nonetheless, this analysis will allow us to compare gaps in care before and after the implementation of new guidelines, and identify factors that may be associated with mortality at CHK during both periods.
Specific objectives
Specifically, this study aimed to;
-
Compare the accuracy of clinical diagnoses for OIs against existing algorithms
-
Determine whether OIs diagnosed at admission are treated within recommended time frames
-
Identify possible factors related to a change in mortality frequencies recorded during the study period.
Method
Type of study
The study is a retrospective, uncontrolled before and after cross-sectional study comparing clinical data of patients hospitalized at the CHK before and after the implementation of new clinical guidelines for the management of advanced HIV developed by MSF-SAMU [10].
Study context
In Kinshasa, DRC, MSF has been operating one of the only dedicated advanced HIV referral clinic, the CHK. The clinic provides specialized care to advanced HIV patients and also provides support to partner and non-partner health centers in Kinshasa, DRC. The CHK was opened in 2002 providing only outpatient HIV services but expanded to providing inpatient care to advanced HIV patients in 2008. CHK today serves as a reference hospital and training center for MSF and its partners. The inpatient unit consists of a 41 bed hospital unit with an average of ~ 160 admissions per month and hospital stays averaging ~ 5 days. The outpatient unit follows an active cohort of ~ 1200 patients, and another 1500 patients from its partner health centers in Kinshasa. Although located in the Lingwala health zone of Kinshasa-DRC, the CHK admits HIV patients from all over Kinshasa and other provinces in DRC. The influx of patients is significant throughout the year with an inpatient bed occupancy rate of around 150% since 2017. Patients admitted at the CHK are mostly advanced HIV patients with a median CD4 of 76cells/μl [IQR, 21–200]. The hospital is currently the only advanced HIV clinic in Kinshasa, and for the context, provides a fairly “high technical platform”, with staff regularly receiving visits and technical support from HIV experts at the MSF-SAMU.
Period of study, participants and sample size
Participants included hospitalized CHK patients who meet study eligibility criteria (see Eligibility criteria). For both periods (before and after the implementation of new guidelines), a total of at least 200 patients were included in the study. Sample sizes for both periods were estimated based on the annual number of hospitalized patients with complete clinic files, a 95% confidence interval and a 5% margin of error. Two time periods were identified for both periods; February 2016 to March 2017 for periods before implementation of new guidelines, and from November 2017 to July 2018 for periods after the implementation of new guidelines.
Eligibility criteria
The following inclusion criteria were established a priori:
-
Patients with a primary diagnoses of 1 of the following 4 OIs at admission: TB, PCP, Toxoplasmosis, non-TB pneumonia.
-
a CD4 count at admission below 200 cell/μl
-
and patients with complete clinic files
Definition of correct, missed, incorrect and misclassified diagnosis:
Correct Diagnosis: Diagnosis on file follows algorithm and meets the definition criteria as set out in the guidelines
Missed Diagnosis: Diagnosis not mentioned in patient’s file despite meeting diagnostic criteria established in the guideline
Incorrect Diagnosis: Does not meet diagnostic criteria set out in the guidelines
Misclassification of diagnosis (misclassification): Incorrectly labelling a diagnosis as either a primary or secondary diagnosis for patients with comorbidities/multimorbidities.
Review of patient files
After selection of eligible patient folders by the principal investigator (FM), a committee of three experienced medical doctors at the CHK was set up to review patient files. The committee was headed by the medical team supervisor (TK). At least two out of the three committee members had to agree on a diagnosis before it could be determined as correct, incorrect, missed or misclassified. Patient files were reviewed against existing guidelines to determine accuracy of diagnosis, i.e. for each period, the guideline used at the time of diagnosis was used by the committee to determine accuracy of diagnosis. All committee members had used both guidelines, however, none of them had a direct role in the development of either guidelines.
Data entry and analysis
Data was encoded into an excel database designed specifically for the study and checked for consistency and accuracy by cross referencing information in patients’ files to those available in the electronic management system at CHK. Files with inconsistent information that could not be verified were excluded. Univariate analysis was used to analyze and compare differences between continuous and categorical variables. Multivariate statistics was used to analyze mortality risk factors. Statistically significant threshold was set at 95% and data analysis was conducted using Microsoft Excel and STATA® software version 15.
Results
Characteristics of patients before and after the implementation of new protocol
Patients included in analysis shared similar clinical backgrounds before and after the implementation of the new guidelines. Two hundred four and Two hundred thirty-one patients were included in the analysis before and after the implementation of new protocols respectively. Median age and sex distributions were similar for both periods, but median hospitalization days (after = 7[IQR2–10], before = 5[IQR4.4–13], p < 0.05%) and median CD4 counts (before = 36 cell/μl [IQR12–85], after = 52 cell/μl [IQR23–109], p < 0.05) were slightly higher after the implementation of new guidelines, see Fig. 1.
Accuracy of clinical diagnosis
We reviewed patient files for 10 major OIs and clinical conditions; lung TB, central nervous and spinal (CNS) TB, non-CNS (TB), brain toxoplasmosis, PCP, Bacterial and Non-TB Pneumonia, Cryptococcal and bacterial meningitis, and bacterial septicemia. Among those reviewed, 40.7% (83/204) of patients had a missed/incorrect diagnosis before new empirical guidelines were implemented compared to 30% (60/231) of patients after the implementation of new guidelines, p < 0.05. Most (63%) patients with a missed/incorrect diagnosis after the implementation of new guidelines had only one missed diagnosis with only 36% having two or more missed diagnosis. A reversed pattern was observed in the period before the implementation of new guidelines, with most (64%) patients having at least 2 or more missed/incorrect diagnosis and only 36% having one missed/incorrect diagnosis, see Table 1.
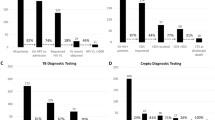
Accuracy of diagnosis for TB, toxoplasmosis, PCP, non-TB pneumonia
After the implementation of new guidelines, accuracy of diagnosis improved for TB, Toxoplasmosis, PCP and Non-TB pneumonia. However, statistically significant differences were only observed for TB and Toxoplasmosis diagnosis. Respectively, 92 and 82.7% of TB and Toxoplasmosis cases were correctly diagnosed after new guidelines were implemented compared to 63 and 62% of TB and Toxoplasmosis cases before the implementation of new guidelines, see Table 2. Among PCP diagnosis, 82% were correctly made after new guidelines compared to 65% before new guidelines (p > 0.05). For non-TB pneumonia, 54% of diagnosis were correctly made before new guidelines compared to 91.7% after implementation of new guidelines (p > 0.05). In addition, missed/incorrect or misclassification for all 4 diseases was lower after the implementation of new guidelines compared to before the implementation of new guidelines (p < 0.05).
Multivariable logistic regression of mortality and danger signs
Mortality frequency for the periods after the implementation of new guidelines were lower than those before the implementation of new guidelines (before = 57.6 and 48.7% after), with statistically significant odds using a multivariate logistic regression model that included age, sex and nine danger signs, [OR = 0.60, CI (0.38–0.97), p < 0.05], see Table 3. Significant determinants of mortality included age, inability to walk at admission, and a Glasgow score of under 15, p < 0.05.
Mortality frequency before 48 h was 19.11% before the implementations of new guidelines compared to 13.7% after the implementation of new guidelines. Mortality after 48 h was also slightly lower in the periods after the implementation of new guidelines compared to before (36% compared to 38%). After the implementation of new guidelines, significant decreases in mortality before and after 48 h were observed for patients admitted with fever, renal failure and respiratory related danger signs. Mortality before and after 48 h among patients with danger signs such as extremely low CD4 count (</=50 cell/μl), dehydration, inability to work, cardiac and neurological related danger signs were also lower after the implementation of new guidelines compared to before (Fig. 2).
Treatment turnaround times
During both periods, median treatment/turnaround times were similar for; when CD4 count results were received, Toxoplasmosis and PCP treatments were started after initial diagnosis, and when antibiotics were given to patients after prescription. However, treatment of TB after initial diagnosis improved from 2 days [IQR = 3] before new guidelines to 1 day [IQR = 1] after new guidelines, p < 0.05. In terms of when treatment was started after diagnosis, significant improvements were observed in the treatment of all three diseases in the first 24 h after the implementation of new guidelines compared to before. Also, after the implementation of new guidelines, nearly 80% of patients received their prescribed antibiotics within the first 24 h, an improvement of 24% compared to periods before the new guidelines were implemented (Table 4). In addition, after the implementation of new guidelines CD4 cell count results were only available for 63% of patients before the implementation of new guidelines compared to 99% after the implementation of new guidelines.
Discussion
Accuracy of clinical diagnosis
This study is among a few studies reporting on the effectiveness of clinical guidelines on the clinical management of OIs among advanced HIV patients. Similar studies have mostly focused on one or two principal morbidities, e.g. TB and/or pneumonia. Results from our study suggests that the introduction of an improved clinical guideline, coupled with clinician training and the installation of laboratory equipment and point of care tests potentially improved the accuracy of clinical diagnosis for the 10 OIs reviewed in this study. For the four principal OIs among advanced HIV patients, accuracy of diagnosis increased by at least 29.5, 20.4, 16.9 and 37.9% for TB, Toxoplasmosis, PCP and non-TB Pneumonia respectively, after the implementation of new guidelines. These results were not surprising as other reports and studies have also documented improvements in clinical outcomes when improved clinical guidelines are introduced to health care settings. For instance, a study by Opoka et al. (2019) on adherence to clinical guidelines and associated mortality noted lower mortality rates when clinical guidelines were effectively used by health care workers [11]. Another study by Dean et al. (2006) also reported that the implementation of a pneumonia treatment guideline was associated with improved patient’s clinical outcome [12]. Other studies on the effectiveness of new and improved guidelines for the management of sepsis, TB, and PCP also reported similar improvements in clinical decision making and patient outcomes [13]. The increase in accuracy of clinical diagnosis of OIs could also be attributed to the availability of advanced laboratory testing instruments as well as the introduction of point of care tests during the implementation of algorithms from clinical guidelines [14,15,16]. Shortly before the implementation of new clinical guidelines, the CHK introduced advanced laboratory and point of care testing packages including GeneXpert, TB-Lam and Serum Cryptococcal Antigen (CRAG) tests. The clinic also commenced periodically testing blood cultures of patients suspected of having OIs at external laboratories in Kinshasa. Thus, improvements observed in clinical diagnosis are thus consistent with expectations for accuracy of clinical diagnosis for OIs and improvement in patient outcomes [11, 12, 17].
Mortality
Mortality frequency in this study far exceeds average frequency of deaths for patients admitted at CHK. Average death frequency (based on admissions) at CHK is usually between 26 and 28% compared to 57.64 and 48.70% before and after the implementation of new guidelines respectively. These results were however expected as the eligibility criteria for the study included patients who usually have high mortality rates at the clinic. For example, mortality frequency among advanced HIV patients presenting with TB as a primary diagnosis is ~ 60%, slightly above frequency of deaths recorded in the current study. We recognize that comparing mortality rates, especially for patients presenting with complex clinical pathologies can be problematic and may lead to false conclusions. Therefore, we are careful to directly relate reduced mortality rates to changes and recommendations made in the new guidelines alone, as there could be other contributing factors not accounted for in our analysis. That being said, other studies and reports have reported reduced mortality and increased survival when new and improved guidelines were introduced. Haynes et al. (2009), for example, in their study on the use of “surgical safety checklist to reduce morbidity and mortality in a global population”, reported that after the introduction of the checklist, there was an overall reduction in complications and subsequent deaths [18]. For our study specifically, possible contributions to the overall significant reduction in mortality could be attributed to the fact that the introduction of new clinical guidelines was also followed by the installation of advanced HIV laboratory testing equipment and of point of care test packages [19]. Furthermore, significant reductions in missed/incorrect diagnosis, especially for the four principal morbidities, could provide further explanation into why reduced mortality rates were observed. Globally, TB for example, accounts for 32% of deaths among advanced HIV patients, and this is mostly because 49% patients with HIV&TB comorbidities could not access appropriate healthcare [20]. It is therefore reasonable to suggest that an increase in accuracy of clinical diagnosis could potentially improve mortality rates among patients. Furthermore, the reduction of mortality among patients presenting with almost all danger signs after the implementation of new guidelines could also provide further explanation into the overall decrease in mortality after the implementation of new guidelines. Of note, significant odds were observed for patients who at admission could not walk, those with a Glasgow score of less than 15 and patients over 45 years of age. These results are consistent with results from other studies [21], and the WHO in their 2017 advanced HIV guideline for the management of advanced HIV, also included these as principal danger signs associated with high mortality among patients needing critical care [19].
Treatment turnaround times
The main goal of the introduction of the new guidelines, point of care tests and the installation of laboratory equipment was to improve patient outcomes by providing clinicians with guidelines and resources that could improve their clinical decision making process in a timely manner. Results from this study showed that treatment turnaround times and antibiotics prescription were improved for the three main principal morbidities at CHK, especially for the first 24 h after admission. For most advanced HIV patients requiring emergency admissions, timely and appropriate care within the first 24 h after admission is critical. Guidelines for the empirical treatment of OIs recommend that patients generally receive antibiotics within 0–24 h after initial diagnosis [22, 23]. On the other hand, timing for when patients’ CD4 count test results were received by clinicians were better before the implementation of new guidelines. However, we must point out that a CD4 count point of care test, Abbott PIMA™, was introduced at CHK during the periods before the implementation of new guidelines. Another explanation for an increase in CD4 count results turnaround times after the implementation of new guidelines, could be associated to the problem of stock out of PIMA™ cartridges and FACSCount™ reagents, as there were more demands for these tests after the implementation of new guidelines. The issue of stock out in Kinshasa-DRC, was explored in a previous study on “Stockouts of HIV commodities in public health facilities in Kinshasa” [24]. Despite an increase in turnaround times for CD4 count test results after the implementation of new guidelines, almost all patients had a CD4 count done during admission (99%), compared to only 63% of patients before the implementation of new guidelines. Following current HIV protocol, this translates into improved triaging of patients and further appropriate testing including TB-LAM, CrAG, etc. [10, 19].
Limitations
The current study was a retrospective cross-sectional study and as such is prone to limitations inherent to such studies [25, 26]. For example, most patient files before the implementation of new guideline had incomplete clinical information and so we had to use a more lengthy time period in order to reach achieve our target sample size. We tried to mitigate against some of these limitations by ensuring that we establish eligibility criteria a priori, cross check and validate data from patient files, ensure review by a panel of 3 medical doctors and a final independent review by the lead author (FM), and conduct multivariate statistics with appropriate covariates. In addition, attempting to compare clinical decisions using two time periods and different guidelines could be problematic in that it could be difficult to control or adjust for other confounding variables, e.g. level of training or experience of clinicians. Furthermore, even though clinical files were reviewed by a panel of three doctors, all of which had used both guidelines, there is always a possibility that some cases might have been inaccurately classified as correct, missed/incorrect or misclassified. Another potential bias could be the fact that the review committee was not blinded to both time periods, which could have been a potential source of bias. To mitigate against these, the study team took extra precautions to ensure that most, if not all, results are correct by ensuring that the committee reviewing clinical files were provided with specific algorithms contained in both guidelines for each OI under assessment, and ensuring that FM review all clinical files for a second time before encoding.
Conclusion
The implementation of new guidelines improved the clinical management of patients with advanced HIV at the CHK, and could have potentially lead to a reduction in mortality at the hospital. Treatment turnaround times were also markedly improved especially for the commencement of treatments in the first 24 h. We therefore recommend that health ministries, departments and organizations consider developing or adapting HIV clinical guidelines so that they are apt and responsive to specific settings. Consideration should also be given to the provision of training for frontline health workers in the field on the use of and application of those guidelines. Lastly the provision of tests, e.g. point of care tests, and other clinical laboratory support could be helpful in the management of advanced HIV patients presenting with OIs.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AIDS:
-
Acquired immunodeficiency syndrome
- ART:
-
Antiretroviral therapy
- CHK:
-
Centre Hospitalier De Kabinda
- CNS:
-
Central nervous and spinal
- CRAG:
-
Serum Cryptococcal Antigen
- DRC:
-
Democratic Republic of Congo
- HIV:
-
Human immunodeficiency virus
- MSF:
-
Médecins Sans Frontières
- OIs:
-
Opportunistic infections
- PCP:
-
Pneumocystis pneumonia
- SAMU:
-
Southern African Medical Unit
- TB:
-
Tuberculosis
- TB-LAM:
-
Tuberculosis mycobacterial lipoarabinomannan
- UNAIDS:
-
Joint United Nations Programme on HIV/AIDS
- WHO:
-
World Health Organization
References
UNAIDS. Global AIDS update. 2017. [cited 2019 Nov 1]. Available from: https://www.unaids.org/sites/default/files/media_asset/Global_AIDS_update_2017_en.pdf.
Ford N, Meintjes G, Calmy A, Bygrave H, Migone C, Vitoria M, et al. Managing advanced HIV disease in a public health approach. Clin Infect Dis. 2018;66(Suppl 2):S106–SS110.
Edwards N, Kahwa E, Hoogeveen K. Results of an integrative analysis: a call for contextualizing HIV and AIDS clinical practice guidelines to support evidence-based practice. Worldviews Evid-Based Nurs. 2017;14(6):492–8.
Richardson ET, Grant PM, Zolopa AR. Evolution of HIV treatment guidelines in high and low-income countries: converging recommendations. Antivir Res. 2014;103:88–93.
Schull MJ, Cornick R, Thompson S, Faris G, Fairall L, Burciul B, et al. From PALSA PLUS to PALM PLUS: adapting and developing a south African guideline and training intervention to better integrate HIV/AIDS care with primary care in rural health centers in Malawi. Implement Sci. 2011;6(1):82.
van Schalkwyk C, Mndzebele S, Hlophe T, Calleja JMG, Korenromp EL, Stoneburner R, et al. Outcomes and impact of HIV prevention, ART and TB programs in Swaziland – early evidence from public health triangulation. PLoS One. 2013;8(7):e69437.
Ndirangu J, Newell M-L, Tanser F, Herbst AJ, Bland R. Decline in early life mortality in a high HIV prevalence rural area of South Africa: evidence of HIV prevention or treatment impact? AIDS Lond Engl. 2010;24(4):593–602.
Bor J, Herbst AJ, Newell M-L, Bärnighausen T. Increases in adult life expectancy in rural South Africa: valuing the scale-up of HIV treatment. Science. 2013;339(6122):961–5.
Diro E, van Griensven J, Mohammed R, Colebunders R, Asefa M, Hailu A, et al. Atypical manifestations of visceral leishmaniasis in patients with HIV in north Ethiopia: a gap in guidelines for the management of opportunistic infections in resource poor settings. Lancet Infect Dis. 2015;15(1):122–9.
MSF HIV/TB Guide for Hospital Level | MSF SAMU. SAMU. [cited 2019 Nov 5]. Available from: https://samumsf.org/en/resources/hiv/advanced-hiv-disease/msf-hivtb-guide-hospital-level.
Opoka RO, Ssemata AS, Oyang W, Nambuya H, John CC, Karamagi C, et al. Adherence to clinical guidelines is associated with reduced inpatient mortality among children with severe anemia in Ugandan hospitals. PLoS One. 2019;14(1):e0210982.
Dean NC, Bateman KA, Donnelly SM, Silver MP, Snow GL, Hale D. Improved clinical outcomes with utilization of a community-acquired pneumonia guideline. Chest. 2006;130(3):794–9.
Gurnani PK, Patel GP, Crank CW, Vais D, Lateef O, Akimov S, et al. Impact of the implementation of a sepsis protocol for the management of fluid-refractory septic shock: a single-center, before-and-after study. Clin Ther. 2010;32(7):1285–93.
Scott L, da Silva P, Boehme CC, Stevens W, Gilpin C. Diagnosis of opportunistic infections: HIV co-infections: tuberculosis. Curr Opin HIV AIDS. 2017;12(2):129–38.
Manoto SL, Lugongolo M, Govender U, Mthunzi-Kufa P. Point of care diagnostics for HIV in resource limited settings: an overview. Medicina (Mex). 2018;54(1) [cited 2019 Nov 1]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6037236/.
Brooks JT, Kaplan JE, Holmes KK, Benson C, Pau A, Masur H. HIV-associated opportunistic infections—going, going, but not gone: the continued need for prevention and treatment guidelines. Clin Infect Dis. 2009;48(5):609–11.
Panel on Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. 2019. [cited 2019 Dec 10]. Available from: https://aidsinfo.nih.gov/contentfiles/lvguidelines/adult_oi.pdf.
Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat A-HS, Dellinger EP, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360(5):491–9.
World Health Organization. Guidelines for managing advanced hiv disease and rapid initiation of antiretroviral therapy. 2017. [cited 2019 Nov 1]. Available from: https://apps.who.int/iris/bitstream/handle/10665/255884/9789241550062-eng.pdf.
World Health Organization. TB HIV factsheet. 2019. [cited 2019 Nov 4]. Available from: https://www.who.int/tb/areas-of-work/tb-hiv/tbhiv_factsheet.pdf?ua=1.
Griesel R, Stewart A, van der Plas H, Sikhondze W, Mendelson M, Maartens G. Prognostic indicators in the World Health Organization’s algorithm for seriously ill HIV-infected inpatients with suspected tuberculosis. AIDS Res Ther. 2018;15(1):5.
Federal HIV/AIDS Prevention and Control Office, Federal Ministry of Health, Ethiopia. 2008. [cited 2019 Dec 10]. Available from: https://www.who.int/hiv/pub/guidelines/ethiopia_art.pdf.
Seddon J, Bhagani S. Antimicrobial therapy for the treatment of opportunistic infections in HIV/AIDS patients: a critical appraisal. HIVAIDS. 2011;3:19–33.
Gils T, Bossard C, Verdonck K, Owiti P, Casteels I, Mashako M, et al. Stockouts of HIV commodities in public health facilities in Kinshasa: barriers to end HIV. PLoS One. 2018;13(1):e0191294.
Mann CJ. Observational research methods—cohort studies, cross sectional studies, and case–control studies. Afr J Emerg Med. 2012;2(1):38–46.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–9.
Acknowledgements
The authors would like to acknowledge staff and patients of the Centre Hospitalier De Kabinda (CHK) in Kinshasa, DRC for their support in the conduct of this study. The authors are also thankful to all expat and national staff of the HIV project of Médecins Sans Frontières in Kinshasa, DRC.
Funding
The authors did not receive specific funding for the conduct of this research.
Author information
Authors and Affiliations
Contributions
MF conceived, collected, encoded, analyzed data. MLD reviewed data, sought ethics approvals, analyzed and wrote the article. MR encoded, developed database, partly analyzed data and edited article. HR was part of the study conception, data encoding and initial data analysis. KT, MG & NN reviewed clinical data, contributed to the development of study database and edited article. VCG, BR and IP were part of the study conception, provided input in data collection and helped with Ethics approvals. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study received approval from the Ethics Review Board (ERB) of the School of Public Health at the University of Kinshasa and also met MSF ERB exemption criteria on ‘studies/articles based on pre-existing clinical data routinely collected in a program’.
Consent for publication
Not Applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mangana, F., Massaquoi, L.D., Moudachirou, R. et al. Impact of the implementation of new guidelines on the management of patients with HIV infection at an advanced HIV clinic in Kinshasa, Democratic Republic of Congo (DRC). BMC Infect Dis 20, 734 (2020). https://doi.org/10.1186/s12879-020-05470-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-020-05470-0