Abstract
Background
Hepatitis B virus (HBV) infection is one of the major public health problems worldwide. Limited information exists about the epidemiology of HBV infection in Ethiopia. This study aimed to assess sero-prevalence of HBV markers and associated factors in children living in Hawassa City, southern Ethiopia.
Methods
A community-based cross-sectional study was conducted among 471 children in Hawassa City, southern Ethiopia from May to September, 2018. A total of 471 children were included in the study using a multistage sampling technique. Data on demographic and risk factors were gathered using structured questionnaires. Blood samples were collected and sera were screened for hepatitis B surface antigen (HBsAg), antibody to core antigen (anti-HBc), and antibody against surface antigen (anti-HBs) using enzyme-linked immunosorbent assay.
Results
The sero-prevalence of HBsAg, anti-HBc, and anti-HBs markers among children were 4.4, 19.5 and 20.0%, respectively. Children at higher risk of having HBsAg marker were those who had a history of injectable medications (AOR 5.02, 95% CI: 1.14, 22.07), a family history of liver disease (AOR 6.37, 95% CI: 1.32, 30.74), a HBsAg seropositive mothers, (AOR 11.19, (95% CI: 3.15, 39.67), and had no vaccination history for HBV (AOR, 6.37, 95% CI: 1.32, 30.74). Children from families with low monthly income, who were home delivered, unvaccinated for HBV or with HBsAg seropositive mother had increased risk of having anti-HBc.
Conclusions
The study findings showed an intermediate endemicity of HBV infection in the study setting. The observed rate of residual HBV infection with low rate of immunized children after HBV vaccination was high. Hence, introducing birth dose vaccine, safe injection practice and improving immunization coverage during pregnancy as part of the antenatal care package should be considered. Furthermore, governmental and non-governmental organizations should give attention on timely measures for the prevention of ongoing vertical transmission from mother to child as well as early horizontal transmission of HBV in Hawassa City, Ethiopia.
Similar content being viewed by others
Background
Hepatitis B virus (HBV) is a deoxyribonucleic acid (DNA) virus classified under the hepadnaviridae family [1, 2]. About 257 million people globally had chronic HBV infection in 2015 [3, 4]. It was estimated that, annually, about 4.5 million new cases occurred, and 887, 000 people die globally from chronic sequelae of HBV infection including cirrhosis (52%) and liver cancer (38%) [5]. Africa has the second largest number of chronic HBV carriers after Asia and is considered as a region of highly endemicity [6]. About 60 million people in Africa are chronically infected with HBV and an estimated prevalence of 6.1% in adult population [7, 8].
HBV transmission occurs through sexual exposure, transfusion of infected blood, and use of unsterilized equipment for medical procedures and sharing of sharp materials [9]. However, perinatal exposure to HBV is the most common mode of transmission in areas of medium to high endemicity [10]. Babies born to a mother who is positive for HBsAg and HBeAg markers have ≥90% chance of contracting the infection and becoming chronic carrier [11]. Of these children, 15 to 25% have risk of dying from cirrhosis or liver cancer during adulthood [12, 13].
HBV is an important public health problem in Ethiopia, and the epidemiology varies with geographical area, population practice, age and mode of acquisition [10, 14, 15]. A previous national survey showed that 10.8% of young men had HBsAg, and 73.3% had at least one HBV marker [16]. A 7% sero-prevalence of HBsAg was also reported in a community-based study conducted in Addis Ababa [10].
The World Health Organization (WHO) set a strategy to reduce HBV incidence in children under-five to below 1% by 2020, and decreasing the prevalence to 0.1% by 2030 [3]. In Ethiopia, HBV vaccination has been introduced to the national Expanded Program for Immunization (EPI) since 2007 [17]. The current immunization schedule for children under one year of age in the country includes; BCG, measles, DPT-HepB-Hib or penta-valent vaccine, OPV. The HBV vaccination as (DPT3/PENTA 3) coverage was 73 and 86% in 2007 and 2011, respectively in Ethiopia [18]. To assess the progress of interventions, understanding the epidemiology of HBV infection and vaccination status would be important. However, there have been limited data on HBV infection in Ethiopia. Therefore, this study aimed to determine sero-prevalence of HBV markers (HBsAg, anti-HBc and anti-HBs) among children at Hawassa City, Southern Ethiopia.
Methods
The study was conducted in Hawassa City in Southern Ethiopia. Hawassa City has 8 sub-cities and located 272 km south of Addis Ababa, Ethiopia (Hawassa city administration, 2011). The city administration is divided into 7 urban sub-cities, containing 20 kebeles (smallest administrative unit) and one rural sub-city with 12 kebeles. According to the report of housing and population census (CSA, 2009), the population size of Hawassa City Administration in 2018 was 374,034; of which 190,757 were males and 183,277 were females [19]. The total children aged 5–8 years old were 56,252 and the total number of households were 78,124.
A community based cross-sectional study was conducted from May to September, 2018. The study population consisted of children aged 5–8 years and who were found at home during the study period. Mothers and/or children who were sick or on antiretroviral therapy or unwilling to participate in the study were excluded. Further, children who had not received full dose vaccine were considered to have no history of vaccination and were excluded from the study.
The sample size was determined using a single population proportion formula with assumptions of 5.3% HBsAg sero-prevalence among children [20], 95% confidence interval, and 3% marginal of error (d). The sample size calculated was 471 after considering a 10% non-response rate and design effect of 2.
Where.
n = Sample size.
Z = Standard normal distribution value at the 95% CI, which is 1.96.
P = The prevalence of HBV infections 5.3% and.
D = The margin of error, taken as 0.03%. Hence.
\( \mathrm{n}=\frac{(1.96)^2(0.053)(0.953)}{(0.30)^2}=214 \) . The final sample size was adjusted as follows:
Sample size = n (sample size) + (10% non-respondent) X Design effect (2). Thus, final sample size (n) was calculated as n = (214+ 21.4) X 2 = 470.85 ~ 471.
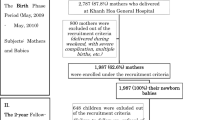
A multistage random sampling technique was used. Two sub-cities were selected using a simple random sampling technique in the first stage, and four kebeles were selected in the second stage. In the third stage, the total sample size was proportionated to the four kebeles. In the last stage, households of eligible study participants were selected using systematic random sampling technique, and study participants were selected using lottery method (Fig. S1).
Pre-tested and structured questionnaires were used to collect information on socio-demographic characteristics and other associated factors. The vaccination status of children was collected from immunization cards and/or by asking mothers. Health workers conducted face-to-face interviews with mothers and gathered the data. Training on data collection and sample drawing and transportation were given, and pretest was done to validate the questionnaire prior to actual work.
Serological analysis
About 5 ml of blood sample was drawn from every child and mother. Samples were transported within 6 h of collection to the laboratory of the Hawassa University Comprehensive Specialized Hospital using cold box. Separated sera were stored at -80 °C and then transported to the Armauer Hansen Research Institute (AHRI) in Addis Ababa for analyses. Sera were tested for HBsAg, anti-HBc, and anti-HBs using enzyme-linked immunosorbent assay (ELISA) (Monolisa PLUS, BIO-RAD, France). Testing was performed according to the instructions of the manufacturer.
Data quality assurance
The questionnaire was prepared in English language and translated to Amharic language and then back to English. One week prior to data collection, the questionnaire was pre-tested on 5% of the calculated sample size at Adare Hospital other than the actual study sites to ensure questions were unambiguous. Prior to the beginning of data collection, all data collectors were trained by the principal investigator. The collected data were checked daily for consistency and accuracy. Standardized procedures were strictly followed during sample collection, storage and analytical process. The quality of test results was maintained using known negative and positive samples as external quality controls.
Operational definitions
-
HBV infected: whose blood is serologically positive for HBsAg
-
HBV immune following a resolved infection: whose blood is serologically HBsAg negative, anti-HBc positive and anti-HBs positive
-
HBV immune following vaccination: anti-HBs positive after vaccination with anti-HBs titer ≥10mIU/ml.
-
HBV susceptible: HBsAg negative, anti-HBc negative and anti-HBs negative
Data analysis
Data entry, cleaning and analysis was done using SPSS version 23.0 software. Frequencies and percentages were calculated to summarize results of categorical variables. Bivariate logistic regression analysis was conducted to compute crude odds ratio (COR). Variables with a p-value < 0.25 in bivariate analysis were candidates for multivariable logistic regression. Adjusted odds ratios (AOR) with 95% confidence intervals (CI) were used to measure strength of the association between HBV infection and its determinant factors. A p-value < 0.05 was considered as a significant association.
Results
Socio-demographic characteristics
A total of 471 study participant were enrolled, of which, 451 (95.8%) were included in the analysis. The mean age of the children was 6.56 years (standard deviation SD), 1.22; range, 5–8 years), and 232 (51.4%) were boys. Among the study participants, 147 (32.6%) were from Alamura, 119 (26.4%) from Hogane-Wacho, and the remaining were from Dume and Wukiro kebeles. (Table 2).
Sero-prevalence of hepatitis B virus markers (HBsAg, anti-HBc and anti-HBs)
The overall sero-prevalence of HBsAg, anti-HBc, and anti-HBs among children was 4.4% [95% confidence interval (CI): 2.8–6.6], 19.5% [95% CI: 16.1–23.4] and 20.0% [95% CI: 16.5–23.8], respectively. All children with HBsAg were also positive for anti-HBc, and 37 (8.4%) participants were positive for both anti-HBs and anti-HBc markers. Of the children, 53 (11.6%) had HBV immunity following vaccination (anti-HBs+) (Table 1). In addition, the prevalence of HBsAg among paired mothers was 7.1% [95% confidence interval (CI): 4.7–9.8] (Table 2).
Associated factors for hepatitis B virus infection among children
Of the study participants, 32 (7.1%) had a history of hospital admission and 36 (8%) had history of injectable medications. The number of children born at home was181 (40.1%), and 215 (47.7%) children were not vaccinated (Table 2).
In multivariable analysis, children who had history of injectable medications were 5 times (AOR 5.02: 95% CI: 1.14, 22.1) more likely to have HBV infection. Children who had a family history of liver disease were 6 times more likely to be exposed to HBV infection (AOR 6.37, 95% CI: 1.32, 30.7). In addition, children born to mothers with HBsAg were at higher risk of HBV infection than children whose mothers were negative for HBsAg (AOR 11.2, (95% CI: 3.15, 39.67). Moreover, children who had no history of vaccination were 6 times more likely to have HBV infection (AOR, 6.36, 95% CI: 1.32, 30.74) as compared to their counterparts (Table 2).
Associated factors for hepatitis B virus exposure among children
After further analysis for those significantly associated variables in multivariable logistic regression analysis, children with family monthly income < 2000 ETB (AOR 2.15, 95% CI:1.25, 3.72), home delivered (AOR 2.82, 95% CI:1.58, 5.06), a history of vaccination (AOR 2.45, 95% CI:1.41, 4.27) or with a HBsAg sero-positive mother (AOR 2.59, 95% CI: 1.13, 5.96) had higher sero-positivity for anti-HBc compared to their counterparts. There was no statistically significant association between self-reported risk factors including average monthly income, history of hospital admission, age and history of day care with HBV infection (Table 3).
Discussion
To reduce the morbidity and mortality related to HBV infection, WHO recommended that all countries should introduce the vaccine in routine immunization programs by 1995 [21]. Ethiopia introduced HBV vaccine to the national EPI program in 2007. However, no data are available on epidemiology of HBV infection in children born after the introduction of the vaccine. We assessed the sero-prevalence of HBV markers among children in Hawassa City, Ethiopia.
The sero-prevalence of HBsAg, anti-HBc, and anti-HBs positivity among children aged 5–8 years was 4.4% [95% CI: 2.7–6.4], 19.5% [95% CI: 16.1–23.4] and 20.0% [95% CI: 16.5–23.8], respectively. According to the criteria of WHO, the observed prevalence of HBsAg showed an intermediate endemicity of HBV infection in the study area [22]. The prevalence of HBsAg in this study was in agreement with results reported in similar study population in Gambia (2.8%) [23]. However, a higher prevalence was reported in Ghanaian rural children (21%) [24], and a lower prevalence was reported from Senegal (2.0%) [25] and Lao People’s Democratic Republic (2.1%) [26]. Further, the prevalence of anti-HBc in this study was lower than results from Gambia (31%) [23], Senegal (27%) [25] and Ghana (75%) [24]. A higher prevalence of anti-HBs was reported in studies conducted in Egypt (57.7–67%) [27] and Senegal (58%) [25]. The difference in prevalence of HBsAg, anti-HBc and anti HBs might be due to variability of study methods employed and diverse risk factors involved in various geographical regions.
Children who had history of using injectable medications were more likely to have HBV infection. Even though direct comparison is difficult because of difference in study population, consistent finding was reported in China [28] and Saudi Arabia [29]. This may be due to proper usage of universal precautions, sharing needle and using unsterilized equipment’s for medical purpose, which increase the risk of infection. Home delivered children had high seropositivity of anti-HBc, as also reported in studies conducted in Addis Ababa, Ethiopia [10] and Saudi Arabia [29]. This may be due to the use of unsterilized or inadequately sterilized instruments. A higher risk of HBV infection in children from family with a history of liver disease compared with those with no family history of liver disease. This result was similar with the study conducted in China [28], Saudi Arabia [29] and USA [30]. This may be due to increased chance of coming in contact with an infected person’s blood and other body fluids.
Children with history of vaccination had lower risk of having HBV infection compared to their counterparts. This result was similar with the study conducted in Papua New Guinea [31], Uganda [32], Pakistan [33] and Nigeria [34]. The study result emphasizes the importance of receiving full HBV vaccination to protect against the infection. It was also observed that the prevalence of residual HBV infection was higher among children with lower rate of immunization (53.4%). According to the Ethiopian demographic health survey report, the coverage of DPT-HepB-Hib3 and all vaccine in urban area of Ethiopia were 60.5, and 48.1%, respectively [35]. This may be explained by absence of HBV birth dose and low maternal education. This study revealed that children who were not vaccinated showed a higher sero-positivity of anti-HBc compared to their counter parts. Similar findings were reported from Uganda [32] and Nigeria [34], indicating a higher risk of exposure to HBV infection among non-vaccinated children.
Maternal HBsAg seropositivity also increased the risk of HBV infection among children. This result was similar with the study conducted in Pakistan [33], Taiwan [36] and Iran [37]. This may be due to a higher risk of HBV transmissibility from infected mother to child during birth, intrauterine transmission in HBeAg-positive mothers with high HBV viral load (> 200,000 IU/ml), and horizontal transmission through sharing sharp materials (like razor blade, and needle) and body fluid exposure [38, 39]. The observed association between mothers HBsAg positivity and child anti-HBc positivity was also shown in studies in Pakistan [33], Taiwan [36] and Iran [37]. This may be due to the fact that HBV infected mothers transmit the virus to their child vertically during birth or horizontally afterwards. Children from family with low monthly income had a higher prevalence of anti-HBc, which was consistent with results from low and middle income countries [40]. In relation to economic situations, an increased risk of exposure to share sharp materials and having lower health care utilization might occur.
Our study had some limitations. First, we did not include testing for HBeAg, anti-HBe and HBV viral load, which are also important determinants of the HBV transmission. Second, the study was done in urban populations and may underestimate the true burden of the disease in the rural community. Third, we did not screen children for HIV infection, which might be considered as missed opportunity to assess the influence of HIV on response to HBV vaccine. Despite these shortcomings, this study provides relevant epidemiological information about HBV infection in children in the study area.
Conclusions
The study findings showed an intermediate endemicity of HBV infection in the study setting. Histories of injectable medication, family liver disease, lack of vaccination and maternal HBsAg sero-positivity were independent predictors of HBV infection. The observed rates of residual HBV infection with low rate of immunized children after HBV vaccination was high. Therefore, introducing hepatitis B vaccine and possibly hepatitis B immunoglobulin within 12 h of birth for infants born to infected mothers and provision of treatment for high viremic pregnant mothers, as well as safe injection practice would be important interventions. Furthermore, governmental and non-governmental organizations should give attention to timely measures for the prevention of ongoing vertical transmission from mother to child as well as early horizontal transmission of HBV in Hawassa/Ethiopia.
Availability of data and materials
There is no remaining data and materials, all information is clearly presented in themain manuscript.
Abbreviations
- HBV:
-
Hepatitis B virus
- HBsAg:
-
Hepatitis B surface antigen
- Anti-HBc:
-
Antibody to core antigen
- Anti-HBs:
-
Antibodies against surface antigen
- HBIG:
-
Hepatitis B immunoglobulin
References
World Health Organization, Guidelines for the Prevention Care and Treatment of Persons with Chronic Hepatitis B Infection: Geneva: World Health Organization; 2015.
Sunbul M. Hepatitis B virus genotypes: global distribution and clinical importance. World J Gastroenterol: WJG 2014;20(18):5427.
WHO. World health statistics 2016: monitoring health for the SDGs sustainable development goals: World Health Organization; 2016.
Disease G B D, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet (London, England). 2017;390(10100):1211–59.
Global Health Estimates. Deaths by cause, age, sex, by country and by region, 2000–2015. Geneva: World Health Organization. 2015;2016.
Kim H, Shin AR, Chung HH, Kim MK, Lee JS, et al. Recent trends in hepatitis B virus infection in the general Korean population. The Korean journal of internal medicine. 2013;28(4):413.
Hwang E W, Cheung R. Global epidemiology of hepatitis B virus (HBV) infection. North American Journal of Medicine and Science. 2011;4(1).
Lemoine M, Eholié S, Lacombe K. Reducing the neglected burden of viral hepatitis in Africa: strategies for a global approach. J Hepatol. 2015;62:469–76.
Jafari S, Copes R, Baharlou S, Etminan M, Buxton J. Tattooing and the risk of transmission of hepatitis C: a systematic review and meta-analysis. Int J Infect Dis. 2010;14(11):e928–e40.
Tegegne D, Desta K, Tegbaru B, Tilahun T. Seroprevalence and transmission of Hepatitis B virus among delivering women and their new born in selected health facilities, Addis Ababa, Ethiopia: a cross sectional study. BMC research notes. 2014;7(1):239.
Bakthavatchalu S. Hepatitis B Surface Antigen Carrier State among Asymptomatic Pregnant Women and Its Correlation with Vertical Transmission. International Journal of Research in Pharmacy & Science. 2012;2(3).
Camvulam N, Gotsch P, Langan RC. Caring for pregnant women and newborns with Hepatitis B or C. Am Fam Physician. 2010;82(10):1225–9.
Lam N-C V, Gotsch PB, Langan RC. Caring for pregnant women and newborns with hepatitis B or C. Am Fam Physician. 2010;82(10):1225–9.
Howell J, Lemoine M, Thursz M. Prevention of materno-foetal transmission of hepatitis B in sub-Saharan Africa: the evidence, current practice and future challenges. J Viral Hepat. 2014;21(6):381–96.
Walle F, Asrat D, Alem A, Tadesse E, Desta K. Prevalence of hepatitis B surface antigen among pregnant women attending antenatal care service at Debre-Tabor Hospital. Northwest Ethiopia Ethiop J Health Sci. 2008;17(17):13–20.
Abebe A, Nokes D, Dejene A, Enquselassie F, Messele T, et al. Seroepidemiology of hepatitis B virus in Addis Ababa, Ethiopia: transmission patterns and vaccine control. Epidemiology & Infection. 2003;131(1):757–70.
Siddiqi N, Khan A, Nisar N, Siddiqi A. Assessment of EPI (expanded program of immunization) vaccine coverage in a peri-urban area. Jpma. 2007;57(8):391–5.
Ethiopia National Expanded Programme on Immunization: Comprehensive Multi-Year Plan 2016–2020. Federal Ministry of Health, Addis Ababa 2015:11.
Lenjiso T, Tesfaye B, Michael A, Esatu T, Legessie Z. SNNPR Hawassa city Adminstration health department. GTP assessment report booklet. 2010-2012;2013:9–65.
Berhe N, Myrvamg B, Gundersen SG. Intensity of Schisosoma mansoni, Hepatitus B, age and sex predict level of hepatic periportal thichkening/ fibrosis (PPT/F), a large scale community based study in Ethiopia. AM J Trop Med Hyg. 2007;77(6):1079–86.
WHO: Hepatitis B Fact Sheet;. 2008.
World health organization. Department of Communicable Diseases Surveillance and Response: Hepatitis B virus; . Geneva: 2002.
Peto TJ, Mendy ME, Lowe Y, Webb EL, Whittle HC, et al. Efficacy and effectiveness of infant vaccination against chronic hepatitis B in the Gambia Hepatitis intervention study (1986–90) and in the nationwide immunisation program. BMC Infect Dis. 2014;14(1):7.
Cho Y, Bonsu G, Akoto-Ampaw A, Nkrumah-Mills G, Nimo JJ, et al. The prevalence and risk factors for hepatitis B surface Ag positivity in pregnant women in eastern region of Ghana. Gut and liver. 2012;6(2):235.
Coursaget P, Leboulleux D, Soumare M, le Cann P, Yvonnet B, et al. Twelve-year follow-up study of hepatitis B immunization of Senegalese infants. J Hepatol. 2004;21(2):250–4.
Komada K, Sugiyama M, Vongphrachanh P, Xeuatvongsa A, Khamphaphongphane B, et al. Seroprevalence of chronic hepatitis B, as determined from dried blood spots, among children and their mothers in Central Lao People's Democratic Republic: a multistage, stratified cluster sampling survey. Int J Infect Dis. 2015;36:21–6.
Salama II, Sami SM, Said ZNA, El-Sayed MH, El Etreby LA, et al. Effectiveness of hepatitis B virus vaccination program in Egypt: multicenter national project. World J Hepatol. 2015;7(22):2418.
Lao TT, Sahota DS, Law L-W, Cheng YK, Leung T-Y. Age-specific prevalence of hepatitis B virus infection in young pregnant women, Hong Kong special administrative region of China. Bull World Health Organ. 2014;92:782–9.
Ageely H, Mahfouz MS, Gaffar A, Elmakki E, Elhassan I, et al. Prevalence and risk factors of Hepatitis B virus in Jazan region, Saudi Arabia: cross-sectional health facility based study. Health. 2015;7:459–65.
Hontelez JA, Hahné S, Koedijk FH, de Melker HE. Effectiveness and impact of hepatitis B virus vaccination of children with at least one parent born in a hepatitis B virus endemic country: an early assessment. J Epidemiol Community Health. 2010;64(10):890–4.
Kitau R, Datta SS, Patel MK, Hennessey K, Wannemuehler K, et al. Hepatitis B surface antigen seroprevalence among children in Papua New Guinea, 2012–2013. The American journal of tropical medicine and hygiene. 2015;92(3):501–6.
Bwogi J, Braka F, Makumbi I, Mishra V, Bakamutumaho B, et al. Hepatitis B infection is highly endemic in Uganda: findings from a national serosurvey. African health sciences. 2009;9(2).
Huma Q, Najma J, Syed EA, Khalif M. The evidence of mother to child transmission of hepatitis B virus infection in Pakistan and the need for hepatitis B immunization policy change. J Pak Med Assoc. 2014;64(4):401–5.
Tabor E, Gerety RJ. Hepatitis B virus infection in infants and toddlers in Nigeria: the need for early intervention. J Pediatr. 2009;95(4):647–50.
Central Statistical Agency, Ethiopia Demographic and Health Survey; final draft report. Addis Ababa Ethiopia. ICF International Calverton, Maryland, USA. 2011.
Lin Y-C, Chang M-H, Ni Y-H, Hsu H-Y, Chen D-S. Long-term immunogenicity and efficacy of universal hepatitis B virus vaccination in Taiwan. J Infect Dis. 2003;187(1):134–8.
Lavanchy D. Hepatitis B virus epidemiology, disease burden, treatment, and current and emerging prevention and control measures. J Viral Hepat. 2004;11(2):97–107.
Zanetti AR, Van Damme P, Shouval D. The global impact of vaccination against hepatitis B: a historical overview. Vaccine. 2008;26(49):6266–73.
Amsalu A, Ferede G, Eshetie S, Tadewos A, Assegu D. Prevalence, infectivity, and associated risk factors of hepatitis B virus among pregnant women in Yirgalem hospital. Implication of Screening to Control Mother-to-Child Transmission. Journal of pregnancy: Ethiopia; 2018.
Razavi-Shearer D, Gamkrelidze I, Blach S, Brandon S, Estes C, et al. THU-097 - the global prevalence of HBsAg by age in 2016 and the case for universal treatment in low and middle income countries. J Hepatol. 2018;68:S169.
Acknowledgements
We like to extend our deepest gratitude to the Ministry of Health for funding this study through the Clinical Research capacity Building program at the Armauer Hansen Research Institute (AHRI). The authors are also grateful to the study participants who took part in the study.
Funding
Small amount of funding was obtained from AHRI to support a postgraduate student.
Author information
Authors and Affiliations
Contributions
RH, AA, AM, BA and TS designed the study. BA, AT, and AM run the laboratory work. BA, TS, AM, SH and DW performed the statistical analyses. All authors contributed to interpretation, the write-up and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the Institutional Review Board of Armauer Hansen Research Institute and College of Medicine and Health Sciences, Hawassa University. The purpose and importance of the study were explained to each study participants. To ensure confidentiality of participant’s codes numbers was used on the questionnaire. Participant was interviewed alone to keep the privacy. All participants were not paid for the test. Informed written consent was obtained from a parent or guardian for children to participate in the study. The study incurs no cost to the study participants and interviewed free of charge. Participants who have diagnosed and suspected cases was get proper advice and referred for further diagnosis, better treatment and care to nearest public health facilities.
Consent for publication
Not applicable.
Competing interests
The authors declare there is no competing interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Fig. S1.
The sampling technique from Hawassa city, Southern Ethiopia, 2019.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Argaw, B., Mihret, A., Aseffa, A. et al. Sero-prevalence of hepatitis B virus markers and associated factors among children in Hawassa City, southern Ethiopia. BMC Infect Dis 20, 528 (2020). https://doi.org/10.1186/s12879-020-05229-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-020-05229-7