Abstract
Background
Since 2000, substantial increases in syphilis in men who have sex with men (MSM) have been reported in many cities. Condomless anal sex (CAS) is one of the factors, along with drugs for sex and sex in group. This study identified factors and clinical manifestations as well as Treponema pallidum (T.pallidum) strains that could be related to early syphilis in Barcelona.
Methods
This prospective study was conducted in a sexually transmitted infections unit in 2015. Epidemiological, behavioral, clinical and microbiological variables were collected in a structured form. Univariate and multivariate statistical analyses were performed focusing on HIV-positive patients.
Results
Overall, 274 cases were classified as having early syphilis (27.5% primary, 51.3% secondary, and 21.2% early latent syphilis). In all, 94% of participants were MSM and 36.3% were HIV-positive. The median number of sexual contacts in the last 12 months was 10; 72.5% practiced CAS, 50.6% had sex in group, and 54.7% consumed drugs. HIV-positive cases had more anonymous sex contacts (p = 0.041), CAS (p = 0.002), sex in group (p < 0.001) and drugs for sex (p < 0.001). In the multivariate analysis, previous syphilis (adjusted odds ratio [aOR] 4.81 [2.88–8.15]), previous Neisseria gonorrhoeae infection (aOR 3.8 [2.28–6.43]), and serosorting (aOR 20.4 [7.99–60.96]) were associated with having syphilis. Clinically, multiple chancres were present in 31% of cases with no differences on serostatus, but anal chancre was most common in HIV-positive patients (p = 0.049). Molecular typing did not conclusively explain clinical presentation in relation to specific T.pallidum strains.
Conclusion
Control of syphilis remains a challenge. Similar to prior studies, HIV-positive patients were found to engage more often in sexual behaviors associated with syphilis than HIV-negative patients. Clinical manifestations were rather similar in both groups, although anal chancre was most common in HIV-positive patients. Various strain types of syphilis were found, but no clinical associations were identified.
Similar content being viewed by others
Background
Since 2000, substantial increases in cases of early syphilis have been reported in metropolitan areas of Western countries. These increases have been described particularly among men who have sex with men (MSM). In Europe, there were 28,701 cases of early syphilis reported in 2015, yielding a rate of 6.0 per 100,000 inhabitants [1]. Similarly, an increase has been described in our setting in Catalonia (Spain): in 2014, the rate of early syphilis was 12.4 per 100,000 inhabitants, a 231% increase over the figures for 2005 observed mainly in MSM [2].
One of the most important factors affecting syphilis transmission is the practice of condomless anal sex (CAS) [3]. Other factors, such as drug consumption, internet use for sexual contacts, and sex in group have also been reported [4]. In some studies, these risk factors are directly related to syphilis, whereas, other studies have found, indirect links with CAS [5, 6]. HIV coinfection has been demonstrated to be strongly associated with syphilis [3, 7].Clinically, some differences have been described between HIV-positive and HIV-negative patients, for instance, in atypical manifestations, such as multiple chancres in primary syphilis [8] or the persistence of chancres in secondary syphilis [9] in HIV-positive patients.
Molecular typing of Treponema pallidum subspecies pallidum (T. pallidum) has been used for different purposes [10,11,12]. Epidemiologically, use of the technique has identified a wide distribution of strain types depending on geographic location, with 14d/g being the most common in Europe [13, 14]. Some strains have been associated with clinical outcomes such as neurosyphilis in rabbits, although this has not been shown in humans [10].
The aim of this study was to provide updated information on syphilis in Barcelona by identifying factors associated with early syphilis and occurrence of these factors, focusing on HIV-positive patients. An additional aim was to describe the clinical characteristics of syphilis, exploring the role of specific strain types of T. pallidum. Altogether, the study was intended to gain an overview of the syphilis epidemic that affects MSM in particular.
Methods
This prospective study was conducted in the Sexually Transmitted Infections Unit Vall d’Hebron-Drassanes in Barcelona, Spain (STIUVD). The STIUVD is the main referral sexually transmitted infections (STIs) in Catalonia and is located in the downtown area of Barcelona. It provides care to patients for a total of 25000 visits per year (60% MSM) and reported around 50% of all syphilis cases seen in Barcelona during the study period.
All patients aged 18 years or older with early syphilis who came between 15 January and 15 October 15, 2015 were eligible to participate in the study. Syphilis diagnosis and management were based on the European syphilis guidelines [15]. Primary syphilis was defined as a typical ulcer (chancre) and/or a positive test using dark-field microscopy or as polymerase chain reaction (PCR) detection of T. pallidum and/or a positive serological test for syphilis. Secondary syphilis was defined based on typical clinical symptoms with positive treponemal and non-treponemal tests. Early latent syphilis was defined as positive serological treponemal and non-treponemal tests with no clinical evidence of infection, with a previous negative syphilis serology, or a four-fold increase in the titer of a non-treponemal test (i.e. two dilutions) within the past 12 months. Cured syphilis was defined as a four-fold decline in the titer of a non-treponemal test within 1 year of treatment.
Behavioral variables
Participants completed a self-administered questionnaire of demographic and sexual behavior information from the previous 12 months. Variables included how they met their partners and practices such as sex in group, drugs for sex, use of condoms, serosorting (sex between partners with same HIV status) and seropositioning (adapting sexual practices according to one’s HIV status). The self-administered questionnaire was based on the European MSM Internet Survey (EMIS) [16], which had been previously modified, piloted, and revised. An adapted version of this questionnaire was used for heterosexual participants. Drugs for sex was defined as substance use 2 h before or during intercourse; chemsex was defined as the use of crystal methamphetamine, gammahydroxybutrate (GHB), and/or mephedrone before or during sexual sessions; and poly drug use was defined as the consumption of three or more drugs, excluding alcohol or cannabis. CAS was defined as the absence of systematic use of a condom, even if used occasionally. Clinical and microbiological variables were completed by the attending physicians. Information on pre-exposure prophylaxis against (PrEP) HIV was not collected because it was not readily available at that time.
If patients had more than 1 episode of syphilis during the study period, the epidemiological and behavioral data were analyzed only once. To determine the risk factors for the acquisition of syphilis according to HIV status, HIV-positive patients were defined as patients who knew that they were HIV-positive at syphilis diagnosis, excluding patients whose diagnoses of HIV and syphilis infection coincided. However, in the clinical analysis, the latter (patients with coincident diagnoses) were included in the HIV coinfection group analysis because the clinical manifestations and course of syphilis could be influenced by HIV.
Microbiological tests
All patients were tested for syphilis following a reverse algorithm sequence screening algorithm. Initial screening consisted of a specific test for antibodies against T. pallidum with any positive results a subsequently confirmed by a non-treponemal test and another treponemal test. The tests used were the treponemal enzyme immunoassay (EIA, Siemens Healthcare Diagnostics, Germany), rapid plasma regain (RPR) test (Biokit, Spain), T. pallidum particle hemagglutination assay (TPHA, Biokit, Spain), and indirect immunofluorescence assay (FTA-abs, BioMérieux, France). Direct diagnoses were made using dark-field microscopy or in-house PCR for T. pallidum [17]. A swab was taken in the case of ulcer, with a second swab taken if there were lesions in more than one site. For typing purposes an extra swab was taken. Treponemal DNA was detected by means of a diagnostic real-time PCR (qPCR) and molecular typing was performed by the Enhanced CDC Typing, analyzing the arp, tpr and tp0548 genes. This typing is based on three regions of T. pallidum-2 first described in 1998 by the Centers for Disease Control and Prevention (CDC) [18] and extended with tp058 in 2010 by Marra et al. [10] Participants were offered screening for N. gonorrhoeae (NG), C. trachomatis (CT) and HIV, as well as hepatitis C virus (HCV) in MSM.
Statistical analysis
Categorical variables were expressed as percentages and comparisons were made using the chi-square test or Fisher’s exact test, as appropriate. The strength of the association was measured as the odds ratio (OR) with 95% confidence intervals (95% CI). Continuous variables were expressed as the mean (+/− SD) or median and interquartile range [IQR]. Comparisons were performed using a Student t test, Mann-Whitney U test, ANOVA, or Kruskal-Walls test with 95% CI if there were more than two groups. Variables identified as clinically significant at the univariate level (p < 0.01) were tested in a final regression model using the Akaike information criterion (AIC). The “R” program (R Foundation for Statistical Computing, Vienna, Austria), version 3.3.1, was used for all analyses.
Ethical approval was granted by the Hospital Vall d’Hebron Ethics Committee (PR(AG)297/2014) and all patients provided written informed consent obtained by the attending physician.
Results
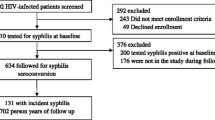
Among patients diagnosed with early syphilis during the study period, 33 patients declined to participate while another 3 were < 18 years old. In total, 270 patients with 274 episodes (4 patients had 2 episodes during this period) were included. In terms of episodes, 76 (27.7%) were primary syphilis, 140 (51.1%) were secondary syphilis and 58 (21.2%) were early latent syphilis. Most patients (257 [95%]) were MSM including bisexuals; there were 2 (0.75%) women and 11 (4.0%) heterosexual men. The median age was 36 [30–44] years, 60.5% were autochthonous, 65.0% had university-level education, 73.5% were employed, and 7.0% were students. A total of 95 (36.0%) patients knew they were HIV-positive at the time of syphilis diagnosis. Four patients had never undergone an HIV test (these patients were excluded from the comparative study). In HIV-positive patients, the median CD4 count was 653 cells/μl [517–810] and 85 (89.5%) were on antiretroviral therapy (ART). Among all patients, 42.8% (110) had a previous history of syphilis.
A total of 266 patients completed the questionnaire answering more than 85% of the questions (2 cases were excluded from the behavioral analysis due to incompleteness). Overall, in the past 12 months, the median number of contacts was 10 and CAS was practiced in 72.5% of cases. Half (50.6%) of them engaged in sex in group and 54.7% used drugs for sex- 25.0% practiced chemsex and 22.6% engaged in poly drug use. Two-thirds of patients searched for sexual partners through apps and 34.5% through the internet (Table 1).
Clinically, in primary syphilis, genital chancre was the most common manifestation in 73.7% (56/76) of cases followed by anal chancre in 22.4% (17/76). Others locations (such as oral or urethral) were uncommon, less than 4% (3/76). All (except 2 cases) were confirmed by positive dark-field microscopy or PCR positive for T. pallidum. Oral chancre was found in 2 patients. Notably, 31.1% had more than one chancre and 2 patients had genital and anal chancres simultaneously. Coexistent chancres in secondary syphilis were observed in 38 (28.5%) of patients. The most frequent secondary lesions were syphilides in the genital area (70.7%) and skin rash (62.1%) affecting the soles (45.0%) more often than the palms of the hands (40.7%). The most common systemic manifestations were asthenia (27.1%), sore throat (22.1%), lymph node enlargement (10.7%), and malaise (10.7%) (Table 2).
The median RPR titre at diagnosis was 1/32 [1/8; 1/64]. Among patients offered STI screening, 257 (94.0%) of them received NG and CT / lymphogranuloma venereum tests, with a prevalence of 9.3 and 16.0%, respectively. HIV was tested in 148 patients with 8.8% (13/148) being newly diagnosed while 5 (2.7%) of 189 patients tested positive for HCV (Table 3).
The majority of patients were treated with benzathine penicillin G 2.4 million units IM as a single dose (93.0%) and 14 (5.2%) were treated with oral doxycycline 100 mg twice daily for 14 days. About a year after treatment, a four-fold decrease in the non-treponemal test titre was observed in all but 14 patients (2 patients were reinfected, 1 had a serological failure and 11 were missing). Five patients became HIV-positive and 4 new cases of HCV occurred during the first year after syphilis diagnosis. Furthermore, 14 new syphilis reinfection cases occurred, 5 of them in HIV-positive patients.
Molecular typing was performed in 78 anogenital ulcers samples (16 samples could be typed only partially): 55 were from genital ulcers and 23 from anal ulcers. A high variety of strains was found making clinical associations unreliable. The strain type distribution (compared by proportions and graphics) between genital and anal chancre was similar, with 14d/g isolated most often in both (12.7% in genital chancre; 30.4% in anal chancre), followed by 14f/g (9.0% in genital chancre; 17.3% in anal chancre). In multiple chancres, 14d/g was also most common (20.0%). One patient with concomitant genital and anal chancres had different types in anal chancre (14f/g) compared with genital chancre (−p/g partial result).
Comparative study by HIV status
All HIV-positive patients were MSM. Compared with HIV-negative patients, HIV-positive patients were older (39 [34–44] vs 34[29–43] years, p = 0.01), and were more likely to have had previous episodes of NG, CT, and syphilis, as well as HCV coinfection (Table 4). They also had more anonymous contacts in the past 12 months (87.0% vs 91%) with a median of 10 [5.75–32.8],3 [1-7]of which were CAS. There was no difference between the group in insertive anal sex; however, HIV-positive patients had more receptive anal sex (82.8% vs. 67.3%; p = 0.011) (Table 1). Concerning condom use for anal sex, HIV-positive patients were more likely to practice CAS (84.3%) than HIV-negative patients (65.5%; p = 0.002). Remarkably, 43.1% of HIV-positive patients practiced serosorting and 25.4% practiced seropositioning, while HIV-negative patients more frequently had CAS after having been tested for HIV (Table 1). Other risk factors were also more common in HIV-positive patients, such as having sex in group (69.4%), use of toys (46.4%), and drugs for sex (71.0%), mainly involving cocaine, GHB, mephedrone, sildenafil, and crystal methamphetamine. Poly drug use was reported by 34 HIV-positive patients (35.7%) and chemsex by 40 (42.1%). Among HIV-negative patients, 27 (16.1%) reported poly drug use (p = 0.05), and 26 (15.5%) reported chemsex (p = 0.001). Four patients, all HIV-positive, reported IV drug use. The final regression model showed that HIV-positive patients with syphilis were more likely to have previous syphilis (adjusted-OR, (ad-OR) 4.81 [2.88–8.15)] and previous NG infection (ad-OR 3.8 [2.28–6.43)]. Although mainly related with people with HIV, serosorting (ad-OR 20.4 [7.99–60.96)] was strongly associated with syphilis in HIV-positive patients.
Clinically, in HIV-positive patients, secondary syphilis was the most common stage (61.9%). Primary syphilis was seen less often (15.2%), with a similar proportion to early latent syphilis (22.6%) compared with HIV-negative patients (early latent syphilis in 20.2%,secondary syphilis in 44.5%, primary in 35%; p = 0.002). After stratifying for previous syphilis as a possible confounding factor, the difference was still significant, secondary syphilis occurred more often in HIV-positive patients without a previous history of syphilis. Anal chancres were more common in HIV-positive patients than in HIV-negative patients (41.2% vs. 17.0%; p = 0.04). In secondary syphilis, there were no significant difference between these two groups (Table 2), even in terms of coexistent chancres. Median RPR titers were higher in HIV-positive patients at 1/64 [1/32–1/64] than in HIV-negative patients at 1/16 [1/4–1/64] p < 0.001 (Table 3). RPR titres stratified by previous history of syphilis showed that this difference persisted among patients without a previous history of syphilis. When RPR titers were stratified by stage the difference disappeared in secondary syphilis, in contrast with primary and early latent syphilis where RPR titers were higher in HIV-positive patients. There were no differences between the two groups in treatment received, evolution of RPR or cure of syphilis after 1 year of treatment (p = 0.2).
Discussion
In our study the dominant profile of the epidemic was MSM. Globally in high-income settings, MSM accounts for a disproportionate burden of syphilis infections [19]. This study shows that this cohort of patients with early syphilis, especially HIV-positive patients, engage in high-risk sexual behaviors. At our clinic we had previously found an HIV coinfection rate of 30% in a study conducted between 2003 and 2013 [20]. In this study, we show that this relationship has persisted over time, as we have now found that 36% of patients with syphilis were HIV-positive and 8.5% were newly diagnosed concomitantly with syphilis. HIV and syphilis are related to each other [21, 22], and syphilis itself could increase the risk of HIV infection [23]. However, this increased risk could also be associated with sexual behavior, as HIV-positive patients engage in more high-risk behaviors than HIV-negative patients as we report here, similarly to others researches [24,25,26,27]. Factors such as sex in group, multiple sex partners, CAS and use of drugs for sex, could also each raise the risk of syphilis [3, 7]. However, these factors are mutually linked, a fact that might increase the probability of infection. An example of this interrelationship is chemsex, a growing global phenomenon which has been associated with a higher number of partners and CAS, situations in which patients more likely to be diagnosed with acute rectal or bacterial STIs, and HCV [28].
From a clinical perspective, HIV may modify the clinical presentation [22] and course of syphilis. After adjusting for a previous history of syphilis, we found that there were still differences in the stage depending on HIV status, with secondary syphilis being more common among HIV-positive patients, similar to the findings of Hutchinson et al. [9] An atypical presentation of syphilis, such as multiple chancres and concurrent primary chancres in secondary syphilis, had been described more often in HIV-positive patients [8, 22]. In our study we found no such differences with the exception that HIV-positive patients had more anal chancres. This could be explained by seropositioning, in addition to the fact that HIV-positive patients practiced receptive anal sex more often than HIV-negative patients. When taking into account T. pallidum typing, molecular studies have associated some strain types with clinical outcomes, such as neurosyphilis [10], ocular involvement [11], or serofast status [12]. Following this methodology, we explored whether or not multiple chancres and other clinical manifestations of early syphilis could be related to a specific strain. We found a high diversity of strains in a limited sample size, precluding any associations. More refined molecular methods such as multilocus sequence typing (MLST) or whole genome sequencing could perhaps be more conclusive [29]. We speculate that HIV could influence the clinical presentation of syphilis in a way similar to how immunological factors affect the manifestation of syphilis in patients with a history of syphilis [30].
Factors that influence the natural course of an infection include host susceptibility, bacterial characteristic and transmissibility, and host immunity [31]. Rekart et al. [32] suggested that ART could increase the susceptibility to syphilis due to changes in the innate and adaptive immune responses to T. pallidum by suppressing mitochondrial function, proinflammatory response, and macrophage activation. They concluded that the immunological effects of ART and ART-induced behavioral changes could act synergistically to increase susceptibility to syphilis. Could this be the reason why HIV-positive patients are more likely to have secondary syphilis than HIV-negative patients? In view of our findings on risk behaviors in HIV-positive patients compared with HIV-negative patients, we suggest that sexual behavior probably has a much greater effect than other factors, as Tuddenhem et al. [33] argued.
This study did have several limitations. First, it was carried out at a single center in Barcelona and, therefore, the findings could not be generalized. Nevertheless, the clinic is a known referral center attending a large number of patients with high-risk sexual behaviors and the main findings are in line with those reported by others elsewhere. Another limitation is the use of self-reporting, sometimes with partial information, an approach that could have influenced some of the results. Apart from the inherent constraints of this method, the limited number of samples for molecular typing made it impossible to gather relevant information on the clinical manifestations of syphilis. Further results on microbiological typing in syphilis obtained in this study will be published elsewhere (Fernandez-Naval C. et al, submitted). Last, the sample size is underpowered to make multiple comparisons between groups but the results are consistent with those of other studies.
Conclusion
In conclusion, HIV-positive MSM patients are more likely than HIV-negative patients to have risk factors for syphilis, such as anonymous contacts, CAS, and chemsex. These factors facilitate syphilis acquisition and and have been found to contribute to the syphilis epidemic in Western countries. HIV-positive patients practicing receptive anal sex and seropositioning may cause them to have anal chancres more often than HIV-negative patients. HIV could influence the natural course of syphilis as secondary syphilis has been found to be more common in HIV-positive patients. These findings are an updated report on syphilis in Barcelona and provide important information to be considered for public health interventions, including STI screening and, access to health services and risk-reduction programs targeting high-risk groups.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to the sensitivity of the topic and hence to ensure confidentiality of the information but are available from the corresponding author on reasonable request.
Abbreviations
- ART:
-
Antiretroviral therapy
- CAS:
-
Condomless anal sex
- CI:
-
Confidence interval
- CT:
-
Chlamydia trachomatis
- GHB:
-
Gammahydroxybutrate
- HCV:
-
Hepatitis C virus
- HIV:
-
Human immunodeficiency virus
- IQR:
-
Interquartile range
- MSM:
-
Men who have sex with men
- NG:
-
Neisseria gonorrhoeae
- OR:
-
Odds ratio
- PCR:
-
Polymerase chain reaction
- RPR:
-
Rapid plasma reagin
- SD:
-
Standard deviation
- STIs:
-
Sexually transmitted infections
References
European Centre for Disease Prevention and Control. Syphilis. In: ECDC Annual Epidemiological Report for 2015. Stockholm: ECDC; 2017. [Accessed 5 Feb 2018]. Available from: https://ecdc.europa.eu/sites/portal/files/documents/AER_for_2015-syphilis.pdf.
Centre d'Estudi Epidemiològics sobre Infeccions de Transmissió Sexual i Sida de Catalunya (CEEISCAT). CEEISCAT Epidemiological Report 2015.Integrated Surveillance System for STI and HIV in Catalonia (SIVES) Technical Document N° 22. Barcelona: CEEISCAT; 2015. [Accessed 5 Feb 2018]. Available from https://scientiasalut.gencat.cat/bitstream/handle/11351/3418/informe_SIVES_2015_informe_epidemiologic_CEEISCAT_2015.pdf.pdf?sequence=1.
Paz-Bailey G, Meyers A, Blank S, Brown J, Rubin S, Braxton J, et al. A case–control study of syphilis among men who have sex with men in new York City association with HIV infection. Sex Transm Dis. 2004;31:581–7.
Wong W, Chaw KJ, Kent CK, Klausner JD. Risk factors for early syphilis among gay and bisexual men seen in an STD clinic: San Francisco, 2002-2003. Sex Transm Dis. 2005;32:458–63.
Taylor MM, Aynalem G, Smith LV, MontoyaJ KP. Methamphetamine use and sexual risk behaviours among men who have sex with men diagnosed with early syphilis in Los Angeles County. Int J STD AIDS. 2007;18:93–7.
Lewnard JA, Berrang-Ford L. Internet-based partner selection and risk for unprotected anal intercourse in sexual encounters among men who have sex with men: a meta-analysis of observational studies. Sex Transm Infect. 2014;90:290–6.
Simms I, Fenton KA, Ashton M, Turner KM, Crawley-Boevey EE, Gorton R, et al. The re-emergence of syphilis in the United Kingdom: the new epidemic phases. Sex Transm Dis. 2005;32:220–6.
Rompalo M, Lawlor J, Seaman P, Quinn TC, Zenilman JM, Hook EW 3rd. Modification of syphilitic genital ulcer manifestations by coexistent HIV infection. Sex Transm Dis. 2001;28:448–54.
Hutchinson CM, Hook EW 3rd, Shepherd M, Verley J, Rompalo AM. Altered clinical presentation of early syphilis in patients with human immunodeficiency virus infection. Ann Intern Med. 1994;121:94–100.
Marra CM, Sahi SK, Tantalo LC, Godornes C, Reid T, Behets F, et al. Enhanced molecular typing of Treponema Pallidum: geographical distribution of strain tupes and association with neurosyphilis. J Infect Dis. 2011;202:1380–8.
Oliver S, Sahi SK, Tantalo LC, Godornes C, Neblett Fanfair R, Markowitz LE, et al. Molecular typing of Treponema pallidum in ocular syphilis. Sex Transm Dis. 2016;43:524–7.
Zhang RL, Wang QQ, Zhang JP, Yang LJ. Molecular subtyping of Treponema pallidum and associated factors of serofast status in early syphilis patients: identified novel genotype and cytokine marker. PLoS One. 2017;12:e0175477.
Salado-Rasmussen K, Cowan S, Gerstoft J, Larsen HK, Hoffmann S, Knudsen TB, et al. Molecular typing of Treponema pallidum in Denmark: a Nationwide study of syphilis. Acta Derm Venereol. 2016;96:202–6.
Grange PA, Allix-Beguec C, Chanal J, Benhaddou N, Gerhardt P, Morini JP, et al. Molecular subtyping of Treponema pallidum in Paris, France. Sex Transm Dis. 2013;40:641–4.
Janier Á, Hegyi V, Dupin N, Unemo M, Tiplica GS, Potočnik M, et al. 2014 European guideline on the management of syphilis. J Eur Acad Dermatol Venereol. 2014;28:1581–93.
The EMIS Network. EMIS 2010: The European Men-Who-Have-Sex-With-Men Internet Survey. Findings from 38 countries. Stockholm: European Centre for Disease Prevention and Control; 2013. [Accessed 14 June 2017]. Available from: http://ecdc.europa.eu/en/publications/Publications/EMIS-2010-european-men-who-have-sex-with-men-survey.pdf.
Orle KA, Gates CA, Martin DH, Body BA, Weiss JB. Simultaneous PCR detection of Haemophilus ducreyi, Treponema pallidum, and herpes simplex virus types 1 and 2 from genital ulcers. J Clin Microbiol. 1996;34:49–54.
Pillay A, Liu H, Chen CY, Holloway B, Sturm AW, Steiner B, Morse SA. Molecular subtyping of Treponema pallidum subespecies pallidum. Sex Transm Dis. 1998;25:404–14.
Abara WE, Hess KL, Neblett Fanfair R, Bernstein KT, Paz-Bailey G. Syphilis trends among men who have sex with men in the United States and Western Europe: a systematic review of trend studies published between 2004 and 2015. PLoS One. 2016;11(7):1–19. https://doi.org/10.1371/journal.pone.0159309.
Arando M, Caballero E, Curran A, Armengol P, Barberá MJ, Vall-Mayans M. The epidemiological and clinical characteristics of the epidemic of syphilis in Barcelona. Actas dermato-sifiliográficas. Accepted.
Hook EW 3rd. Syphilis. Lancet. 2017;389:1550–7.
Lynn WA, Lightman S. Syphilis and HIV: a dangerous combination. Lancet Infect Dis. 2004;4:456–66.
Fleming DT, Wasserheit JN. From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Infect. 1999;75:3–17.
Klitzman RL, Pope HG, Hudson JI. MDMA (“ecstasy”) abuse and high-risk sexual behaviors among 169 gay and bisexual men. Am J Psychiatry. 2000;157:1162–4.
Hirshfield S, Schrimshaw EW, Stall RD, Margolis AD, Downing MJ Jr, Chiasson MA. Drug use, sexual risk, and syndemic production among men who have sex with men who engage in group sexual encounters. Am J Public Health. 2015;105:1849–58.
Grov C, Rendina HJ, Breslow AS, Ventuneac A, Adelson S, Parsons JT. Characteristics of men who have sex with men (MSM) who attend sex parties: Results from a national online sample in the U.S. Sex Transm Infect. 2014;90:26–32.
Friedman SR, Bolyard M, Khan M, Maslow C, Sandoval M, Mateu-Gelabert P, et al. Group sex events and HIV/STI risk in an urban network. J Acquir Immune Defic Syndr. 2008;49(4):440–6. https://doi.org/10.1097/QAI.0b013e3181893f31.
Pakianathan M. 2nd European Chem Sex Forum Report. Panel 1. Berlin; 2018. [Accessed 28 May 2019]. Available from: https://es.slideshare.net/Checkpoints14/european-chemsex-forum-report-2018
Grillová L, Bawa T, Mikalová L, Gayet-Ageron A, Nieselt K, Strouhal M. Molecular characterization of Treponema pallidum subsp. pallidum in Switzerland and France with a new multilocus sequence typing scheme. PLoS One. 2018;13(7):e0200773.
Courjon J, Hubiche T, Dupin N, Grange PA, Del Giudice P. Clinical aspects of syphilis reinfection in HIV-infected patients. Dermatology. 2015;230:302–7.
Stoltey JE, Cohen SE. Syphilis transmission: a review of the current evidence. Sex Health. 2015;12:103–9.
Rekart ML, Ndifon W, Brunham RC, Dushoff J, Park SW, Rawat S, et al. A double-edged sword: does highly active antiretroviral therapy contribute to syphilis incidence by impairing immunity to Treponema pallidum? Sex Transm Infect. 2017;93:374–8.
Tuddenham S, Shah M, Ghanem KG. Syphilis and HIV: is HAART at the heart of this epidemic? Sex Transm Infect. 2017;93:311–2.
Acknowledgements
Not applicable.
Funding
This research received no specific grant from any funding agency, whether commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
MA and MV contributed to the study design and conduct and to manuscript preparation. MM contributed to the statistical analysis MA, CF, DM, PA, MJB, JE and MV contributed to the acquisition of clinical and microbiological data of patients. MM, CF, DM, PA, MJB and JE reviewed the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was granted by the Hospital Vall d’Hebron Ethics Committee. All patients provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Arando, M., Fernandez-Naval, C., Mota-Foix, M. et al. Early syphilis: risk factors and clinical manifestations focusing on HIV-positive patients. BMC Infect Dis 19, 727 (2019). https://doi.org/10.1186/s12879-019-4269-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-019-4269-8