Abstract
Background
There is limited information on patterns of treatment change among new initiators of highly active antiretroviral therapy (HAART) in the regions most affected by HIV/AIDS. This makes it difficult to identify the determinants of treatment change. In this retrospective cohort study, we examined treatment change patterns over a five-year period among initiators of HAART.
Methods
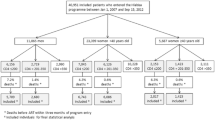
De-identified data were obtained from the Fevers’ Unit Database at the Korle-Bu Teaching Hospital. All adult treatment-naive patients who started treatment with first line HAART between 1st January, 2008 and 31st December, 2012 were followed over a minimum period of three months. The main outcome was the first treatment change, defined as the first substitution/switch in accordance with the standard treatment guidelines. Data were analyzed stratified by year of treatment initiation. Crude and adjusted hazard ratios were calculated.
Results
A total of 3933 patients were followed with almost equal numbers of initiators per year. The mean age (standard deviation) at treatment initiation was 39 (10.3) years. The most prescribed HAART combination was AZT/3TC/EFV and overall for initiators zidovudine combination therapy was about 60%. Utilization of stavudine containing HAART increased gradually until 2010 and then dropped to zero. Over the study period, 44.9% of recorded deaths were from those initiated with a stavudine backbone, 41.1% from a zidovudine backbone, and 11.5% from a tenofovir backbone. Females had a significantly higher rate of treatment change compared to males (p-value = 0.0002), and d4T/3TC/EFV and d4T/3TC/NVP recorded independent treatment change hazard ratios of 12.05 (CI 9.58 to 15.16) and 12.03 (CI 9.27 to 15.61) respectively.. Kaplan-Meier curves showed that treatment change was higher among those who started treatment later in the study period compared with those who started earlier.
Conclusion
A major treatment change in the utilization of antiretroviral medicines in Ghana occurred during the study period which was associated with type of treatment, year of treatment, gender and disease stage. The influence of a policy change during the period may have made a significant impact.. For diseases involving life-long treatment in particular, it is important to monitor and periodically evaluation treatment utilization patterns.
Similar content being viewed by others
Background
The most important intervention that delays and prevents the progression of HIV to AIDS, assuming optimum adherence, is treatment with highly active antiretroviral therapy (HAART) [1]. The first drug shown to be effective against HIV was zidovudine; currently there are at least seven classes of HAART in use, mostly in combinations of different antiviral products [2]. This has led to structured treatment strategies, virtually always under the guidance of national or institutional guidelines. Treatment of naïve patients starts with a first line HAART, but regimens may change depending on adverse effects or on inefficacy as a result of development of drug resistance (virological or immunological). Treatment guidelines are adjusted over time based on such insights and evidence. A typical case is the recommendation to phase out stavudine in the management of HIV/AIDS by the WHO from 2010, because of associated mitochondrial toxicities [3,4,5] manifested as lipodystrophy, lactic acidosis and peripheral neuropathy [6]. This underscores the importance of considering the content and revisions of treatment guidelines when studying time trends of HAART, but such studies are rare in the literature. Notwithstanding its toxicity profile, stavudine is not as expensive as other nucleoside (or nucleotide) transcriptase inhibitors [3], and there are cost-analysis studies showing that it might be cost-effective overall, in some countries [7,8,9].
In several countries, HIV/AIDS risk populations and treatment cohorts have been studied over the last decades [10,11,12]. Sub-Saharan Africa has several of such HIV/AIDS cohorts because more than three-quarters of the disease burden is from this region [13]. An example is the KwaZulu-Natal HIV/AIDS cohort nested within the Africa Centre Demographic Information System (ACDIS) cohort [14]. The existence of these cohorts notwithstanding, there is limited information on patterns and determinants of treatment change among new initiators of HAART in the regions most affected by HIV/AIDS.
About 60% of HIV patients in Ghana are female [15]. The HIV prevalence in Ghana routinely conducted by the HIV Sentinel Surveys (HSS) has gradually reduced since 2003. In 2003, 2008, 2013 and 2014, the median HIV prevalence was 3.6%, 2.2% 1.9% and 1.6% respectively [15]. The estimated final transmission rate decreased from 20.3% to 15.9% between 2011 and 2015 [15].
A well-organized government sponsored HIV/AIDS treatment began in the year 2003 following a period of dominance by private retailers who kept no structured records. As of December 2003, HAART for Ghana’s HIV/AIDS population was being managed by only three treatment centers in the country, including the Korle-Bu Teaching Hospital (KBTH) treatment center in Accra. Treatment of HIV/AIDS has since been decentralized, increasing the number of treatment centers from just 3 in 2003 to 197 by December 2014 [15]. The situation has improved over the years but more work is on-going. This study involves the HIV/AIDS cohort at the KBTH. It is a retrospective cohort study that examined HAART initiation and changes per individual inception year over a five-year period (2008–2012).
Methods
Study site
The Fevers Unit of the KBTH was the study site. The Fevers Unit is one of many units of the Department of Medicine and Therapeutics. The Unit is responsible for the registration and management of all cases diagnosed as HIV/AIDS at the KBTH, as well as those referred from other health institutions in Ghana. Provision of antiretroviral therapy in the Unit started in December 2003. As of 2015, nearly 10,000 clients have been put on HAART at the treatment site. There are three major out-patient clinic days per week, each with an average clinic attendance of about 120 patients per day.
Subjects
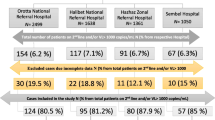
This was a retrospective cohort study. All treatment naive patients who started treatment with first line HAART between 1st January, 2008 and 31st December, 2012 were eligible for this study if they were 15 years or older, enrolled at the Fevers Unit of KBTH and received HAART at the hospital’s pharmacy. The date of exposure was the first date the patient received HAART and each patient was followed over a minimum period of three months. Patients were followed and analyzed per individual inception year. All patients receiving treatment for prevention of maternal to child transmission (PMTCT) of HIV/AIDS were excluded from the study if they were not on full HAART. PMTCT patients who started on full HAART and those who resumed full HAART were enrolled on the date this occurred.
Data source
De-identified and anonymous data for this study were obtained from the Fevers Unit's Database at the KBTH. Diagnostic and treatment records of all newly registered HIV/AIDS patients at the KBTH are captured in this database. Variables in this study included patient age, sex, inception treatment type and date of inception, date of next treatment appointment and treatment change, and WHO disease stage at treatment initiation. Reason for treatment change was not captured in the database.
Study outcome
The main outcome was the first treatment change after inception; each person had at least 3 months of follow-up. First treatment change was defined as the first substitution with another first-line drug or a first switch to a second-line drug as recommended by the treatment guidelines for HAART in Ghana during the study period. In this setting most patients on d4T with good haemoglobin and/or high creatinine levels had their treatment replaced with AZT, while those with acceptable creatinine levels and/or poor haemoglobin levels had a replacement with TDF. Death was defined as any case captured as such in the database. A loss to follow-up was defined as any patient who missed a refill appointment and had no information in the database until 60 days after the next appointment date. For patients who did not change treatment, follow-up was censored at the death date (as captured in database), loss to follow-up, date of transfer to another treatment site, or end of study period, whichever occurred first.
Data analysis
Frequency distributions of baseline variables were calculated. Age was divided into six categories and treatment initiation and treatment change were captured using the HAART combination. Proportions of those who initiated treatment and those with change were calculated for each type of initial HAART by calendar year. Kaplan-Meier plots of year of treatment initiation and HAART combinations (for nucleoside/nucleotide reverse transcriptase inhibitors (NRTI) and non-nucleoside reverse transcriptase inhibitors (NNRTI) during follow-up were made, and corresponding log-rank test was done for each inception year to compare HAART use patterns for the treatment combinations. Rates of treatment change were calculated for different variables and crude and adjusted hazard ratios and corresponding p-values were presented using Cox proportional hazard analysis.
During the study period, HAART guidelines in Ghana were revised two times, the third edition in 2008 and the fourth in 2011 [16]. In the fourth edition, a major amendment was made replacing stavudine (d4T) with an appropriate nucleoside/nucleotide reverse transcriptase inhibitor due to drug-induced side effects of the former. The effects of this event on treatment change was captured in this study. SAS software version 9.3 (SAS Institute, Cary, NC, USA) was used for all analysis.
Results
Over the 5-year period a total of 3933 patients were followed with almost equal numbers of initiators per year. The mean age (and standard deviation) of females at treatment initiation was 37 (10.0) years and 42 (9.9) years for males, but overall the mean age at treatment initiation was 39 (10.3) years with most patients falling between ages 25 and 54 years (Table 1). Among those patients whose WHO disease stage at baseline was known, WHO stage III was the most predominant group. The most prescribed HAART combination in this study was AZT/3TC/EFV, remaining relatively stable over the years. Overall, zidovudine combination HAART amounted to 60.2% (2366/3933) of all patients initiated on HAART, followed by about 28.4% (1117/3933) for a stavudine combination HAART, and about 10% for a tenofovir combination HAART. Treatment initiation with a stavudine containing HAART increased gradually until 2010 and dropped to zero in 2012. There was an increase in the use of tenofovir (TDF) combination HAART. Table 1 also shows that age group (p = 0.0990) and gender (p = 0.3995, were not significantly affected with the changing years of treatment..
Recorded deaths (Table 1) as a percentage of those who were initiated HAART from 2008 to 2012 were 3.8 (32/836), 8.0 (65/810), 6.5 (52/804), 5.8 (44/753), and 6.0 (44/730) respectively. Over the study period, 44.9% compared with 41.1% (p < 0.0001) of deaths were from those initiated on a stavudine and zidovudine backbone respectfull,, 11.5% from a tenofovir backbone and 2.5% were initiated with other HAART combinations. In Fig. 1 it can be seen that more than 50% of treatment changes occurred before 20 months of follow-up and the last change occurred after 54.5 months of follow-up. We can infer from Table 2 that those who had been on treatment much longer had a reduced rate of treatment change per 1000 person months of follow-up. The highest rates of treatment change were recorded in 2010 (17.9 per 1000 person-months) and 2011 (18.7 per 1000 person-months). In all there were 93.5% substitutions (from one first line to another first line HAART) and 6.5% switches (from a first line to a second line HAART).
Among those on HAART the lowest rates of treatment change was recorded by those on a tenofovir or zidovudine combination therapy. Table 2 shows that d4T/3TC/EFV and d4T/3TC/NVP recorded the highest rates of treatment change of 36.16 per 1000 person months and 35.04 per 1000 person-months respectively, and compared with the reference treatment, these changes were significant (p < 0.0001). A tenofovir combination HAART (especially with efavirenz) in this study looked more protective against treatment change compared to the reference HAART (independent p-value of 0.013 and 0.358 for TDF/3TC/EFV and TDF/3TC/NVP respectively). Females had a significantly higher rate of treatment change compared to males (p-value = 0.0002). There was no difference in treatment change among different age groups. This is clear from the overlaps of the confidence intervals of the groups. Those with WHO stage IV at baseline had the highest rate of change of treatment (14.55 per 1000 person months).
Kaplan-Meier curves show that treatment change was higher among those who started treatment later in the study period compared to those who started earlier (see Fig. 2). Figure 3A shows that by the end of the study period 91.1%, 97.7%, and 92.0% of those on a zidovudine combination therapy, tenofovir combination therapy, and those on “other” combination therapy respectively, were censored compared with only 34.6% of those on a stavudine combination therapy (p < 0.0001); Fig. 3B shows that there was no difference between the two non-nucleoside reverse transcriptase inhibitors (log rank test p-value = 0.869). Adjusted hazard rations in Table 2 shows that compared to 2008, changes in 2009, 2010 and 2011 were significantly different, but that of 2012 was not. There was no treatment change difference between the reference age group of less than 25 years and all other age groups in this study. Females had a 19% higher treatment change ratio compared with males.
Discussion
This study showed that Zidovudine based combination therapy was the most prescribed HAART over time in all the five inception cohorts. By the end of the study period, most patients on stavudine based combination therapy had their treatment replaced with another nucleoside (or nucleotide) reverse transcriptase inhibitor.. Death rates were higher among those initiated on a stavudine combination backbone compared to those on zidovudine or tenofovir combinations. Independent hazard ratios showed that apart from age group, all other variables had a role to play concerning treatment change in this study.
Death rates in this study were significantly higher among those on stavudine compared to zidovudine. In a study by Laurent et al. in Cameroun using ZVD/3TC/NVP and d4T/3TC/NVP [17], a similar observation was made. Most antiretroviral medicines are associated with documented side effects, hence the need for continuous monitoring. Although this study did not look at risks of HAART, it is recommended that databases should capture such occurrences to promote further studies. The low number of switches in this study compared to substitutions show that most of the treatment changes were not as a result of treatment failure. In a previous study on treatment change at the same study site during the period 2004 to 2009, Ankrah et al. [18] observed that treatment switching accounted for about 20% of the changes compared to just over 6% in this study.
In the first three years during follow-up treatment change was initially gradual. This was followed by a period of increased treatment change and then it ended with another gradual phase. Those who started treatment from 2011 missed the initial gradual phase but experienced a steep phase followed by a gradual treatment changing phase. This implies that something may have triggered the treatment change after 2010. In particular, in the 2010 revision of the antiretroviral therapy for HIV infection for adults and adolescents [19], the WHO made a general recommendation of a progressive replacement of stavudine in HIV/AIDS treatment centers, and gave directions on how less endowed health systems should roll out these changes in order to avoid wastage and contain cost. The need to change was as a result of empirical evidence of toxicity associated with the use of stavudine [3,4,5,6, 20, 21]. The actual change however, depended on how such countries adopted and adapted to the recommendations. In Ghana patients suspected to be at increased risk of toxicity were the first to be affected, and gradually, all those on stavudine had their treatment replaced with either a first or a second line treatment depending on the presenting situation.
It was evident that most patients in this cohort, originally on stavudine, had a replacement with tenofovir over time. These changes were made based on well informed reasons. Stavudine-related dyslipidemia was reduced significantly after replacement with tenofovir [22]. This was due to improvement in total cholesterol, low density lipoprotein cholesterol and triglyceride levels [22]. In a randomized double blind study, Gallant et al. [23] reported that tenofovir was as efficacious as stavudine but the former had better lipid profiles and reduced lipodystrophy compared to the latter. Results from this study show that a tenofovir combination HAART (especially a combination with efavirenz) may have a slight edge over a zidovudine combination HAART. In a systematic review and meta-analysis, a tenofovir combination HAART showed superior viral load suppression, and was better tolerated by patients [24]. However, emtricitabine, instead of lamivudine was the supporting drug. Normally tenofovir combination HAART is given as a single daily dose compared to a twice daily dose for zidovudine. This may lead to better adherence with a tenofovir HAART. Furthermore, tenofovir is the drug of choice among HIV patients co-infected with hepatitis. While tenofovir can easily replace zidovudine if there is a toxicity among patients on the latter drug, the vice-versa cannot be easily done where patients co-infected with hepatitis are concerned. All that said, the use of tenofovir in this setting is not as established as that of zidovudine. It will take us some time to make a final decision on which combination is the better of the two medicines. Changes from stavudine to zidovudine as observed in this study were moderate, in line with what we know about the differential profiles of these products [25]. These activities form part of the commitment of HIV policy makers and health care workers to ensure that HIV/AIDS patients attain optimum quality of life during treatment.
Our results underscore how timely the Ghanaian health system adhered to WHO’s new treatment policy intervention. This was similar to the situation in Botswana [26] where the authorities did not wait for stavudine associated signs and symptoms to occur before considering to change. Approaches of this nature have been described as very good [27] because of the progressive nature of stavudine related symptoms [28]. Data capture also improved during the period. This was particularly reflective by the fact that in the 2008 cohort almost two-thirds of the cohort had no recording of WHO disease stage, however, in the 2012 cohort WHO disease classification was almost complete.
The observation of low frequencies of deaths in this study may be due to various reasons. These include our inability to determine the causes of loss to follow-up (discharges, abscondees, unreported deaths) from the database. It may also be due to conscientious treatment offered at the treatment center. This is because the study site is a national referral site with an increased probability of having the sickest HIV/AIDS patients in the country. The large numbers of missing values, for example, data on WHO stage was a limiting factor that calls for further reinforcement in the data capture at the treatment site. Another limitation was the parsimonious nature of the variables in our dataset. This may have led to a number of unmeasured confounders, the presence of which may have better explained the reasons for treatment change in this study.
Conclusion
This study has shown that between 2008 and 2012, utilization of antiretroviral medicines in Ghana went through a major transition. In this period, stavudine was replaced with tenofovir, another nucleoside (or nucleotide) reverse transcriptase inhibitor. Stavudine has since been phased out of HIV/AIDS treatment among adults in Ghana. This study shows that these changes were as a result of several factors including the type of treatment, year of treatment, gender and WHO disease stage. International policy changes firmly grounded on empirical evidence may have also contributed to this study’s findings.. During the period HIV/AIDS data capture also showed some improvement. For diseases involving life-long treatment, it is important to monitor and periodically evaluate treatment utilization.
Abbreviations
- 3TC:
-
Lamivudine
- ACDIS:
-
Africa Center for Demographic Information Systems
- AIDS:
-
acquired immunity deficiency syndrome
- AZT:
-
Zidovudine
- EFV:
-
Efavirenz
- HAART:
-
highly active antiretroviral therapy
- HIV:
-
human immune virus
- KBTH:
-
Korle-bu. Teaching Hospital
- PMTCT:
-
prevention of maternal to child transmission
- TDF:
-
Tenofovir
- WHO:
-
World Health Organization
References
Health Topics, HIV/AIDS. http://www.who.int/topics/hiv_aids/en/. Accessed 15/10/2016.
de Clercq E. Antiretroviral Drugs. Curr Opin Pharmacol. 2010;10(5):507–15.
Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. Recommendations for a public health approach 2013. http://apps.who.int/iris/bitstream/10665/85321/1/9789241505727_eng.pdf Accessed 27/06/2017.
Policy brief. AIDS medicines and diagnostic service: Transition to new HIV treatment regimens - Procurement and supply chain management issues. March 2014. UNITAID, PEPFAR, The Global Fund .
Lewis W, Day BJ, Copeland WC. Mitochondrial toxicity of NRTI antiviral drugs: An integrated cellular perspective. Nat Rev Drug Discov. 2003;2(10):812-822.
Boulle A, Orrell C, Kaplan R, Cutsem GV, McNally M, Hilderbrand K, et al. Substitutions due to antiretroviral toxicity or contraindications in the first three years of antiretroviral therapy in a large South African cohort. Antivir Ther. 2007;12:753–60.
Bender MA, Kumarasamy N, Mayer KH, Wang B, Walensky RP, Flanigan T, et al. Cost-effectiveness of tenofovir as first-line antiretroviral therapy in India. Clin Infect Dis. 2010;50(3):416–25.
Jouquet G, Bygrave H, Kranzer K, Ford N, Gadot L, Lee J, et al. Cost and cost-effectiveness of switching from d4T or AZT to a TDF-based first-line regimen in a resource-limited setting in rural Lesotho. J Acquir Immune Defic Syndr. 2011;58(3):e68–74.
Rosen S, Long L, Fox M, Sanne I. Cost and cost-effectiveness of switching from stavudine to tenofovir in first-line antiretroviral regimens in South Africa. J Acquir Immune Defic Syndr. 2008;48(3):334–44.
Coutinho RA. Amsterdam cohort studies on HIV and AIDS. J Acquir Immune Defic Syndr. 1998;17(1):S4–8.
Elamin W, Bibby DF, Clark DA, Anderson J, Deayton JR. HIV-2 in the United Kingdom-the North East London Cohort. HIV MEDICINE. 2013;14:53.
Staehelin C, Rickenbach M, Low N, Egger M, Ledergerber B, et al. Migrants from Sub-Saharan Africa in the Swiss HIV Cohort Study: access to antiretroviral therapy, disease progression and survival. AIDS. 2003;17:2237–44.
UNAIDS. Global AIDS epidemic facts and figures, 2012: Geneva, Switzerland; UNAIDS; 2012.
Tanser F, Hosegood V, Barnighausen T, Herbst K, Nyirenda M, et al. Cohort Profile: Africa Centre Demographic Information System (ACDIS) and population-based HIV survey. Int J Epidemiol. 2008;37:956–62.
Ghana National HIV and AIDS Strategic Plan 2016–2020. Ghana AIDS Commission, Ghana.
Guidelines for antiretroviral therapy in Ghana.Ministry of Health, Ghana Health Service. 2002, 2005, 2008 and 2011.
Laurent C, Bourgeois A, Mpoudi-Ngolé E, Ciaffi L, Kouanfack C, Mougnutou R, et al. Tolerability and effectiveness of first-line regimens combining nevirapine and lamivudine plus zidovudine or stavudine in Cameroon. AIDS Res Hum Retrovir. 2008;24(3):393–400. https://doi.org/10.1089/aid.2007.0219
Ankrah D, Lartey M, Agyepong I, Leufkens HGM, Mantel-Teeuwisse AK. Adherence and treatment change among HIV/AIDS patients in Ghana: A nested case-control study. J AIDS Clin Res. 2015;6:10.
Antiretroviral therapy for HIV infection and adults and adolescents: recommendations for a public health approach. 2010 rev. WHO 2010.
Subbaraman R, Chaguturu SK, Mayer KH, Flanigan TP, Kumarasamy N. Adverse effects of highly active antiretroviral therapy in developing countries. Clin Infect Dis. 2007;45(8):1093–101.
McComsey G, Lonergan JT. Mitochondrial dysfunction: patient monitoring and toxicity management. J Acquir Immune Defic Syndr. 2004;37(Suppl 1):S30–5.
Llibre JM, Domingo P, Palacios R, Santos J, Pe’rez-Elı’as MJ, la Rosa SR, et al. Sustained improvement of dyslipidaemia in HAART treated patients replacing stavudine with tenofovir. AIDS. 2006;20:1407–14.
Gallant JE, Staszewski S, Anton L, Pozniak AL, DeJesus E, Suleiman JMAH, et al. Efficacy and Safety of Tenofovir DF vs Stavudine in Combination Therapy in Antiretroviral-Naive Patients: A 3-Year Randomized Trial. JAMA. 2004;292:191–201.
Dadi TL, Kefali AT, Mega TA, Kedir MS, Addo HA, Biru TT. Efficacy and tolerability of tenofovir disoproxil fumarate based regimen as compared to zidovudine based regimens: a systematic review and meta-analysis. AIDS Research and Treatment. 2017;2017:5792925.
Spaudling A, Rutherford GW, Siegfield N. Stavudine or zidovudine in three-drug combination therapy for initial treatment of HIV infection in antiretroviral naïve individuals. (Review) Copyright © 2011. The Cochrane Collaboration. Published by JohnWiley & Sons, Ltd.
Botswana National HIV/AIDS Treatment Guidelines 2012. Botswana Ministry of Health.
Franzeck FC, Letang E, Mwaigomole G, Jullu B, Glass TR, et al. cART prescription trends in a prospective HIV cohort in rural Tanzania from 2007 to 2011. BMC Infect Dis. 2014;14:90. https://doi.org/10.1186/1471-2334-14-90.
Phan V, Thai S, Choun K, Lynen I, van Griensven J. Incidence of treatment limiting toxicity with stavudine-based antiretroviral therapy in Cambodia: a retrospective cohort study. PLoS One. 2012;7(1):e30647.
Acknowledgements
The authors are thankful to Mr. Ekow Wiah of the National AIDS Control Program, Accra, Ghana, for making available the data for this project, and to Mr. Francis Turkson for his help with cleaning of the data prior to data analysis.
Funding
This research was not sponsored.
Availability of data and materials
The dataset analysed during the current study is not publicly available due to the sensitivity of the subgroup (HIV/AIDS patients) studied, but is available from the corresponding author on reasonable request. No materials whatsoever, were used for this study.
Author information
Authors and Affiliations
Contributions
DNAA is the lead author of the study. He was involved with the data acquisition, analysis, and data interpretation. ML was involved with the data acquisition, interpretation, revision of manuscript for intellectual content and final approval for version to be published. HGML and AKM conceptualized the study and played an important role in the design, analysis, data interpretation, revision for intellectual content and final approval for version to be published. All authors agreed to be accountable for all aspects of the work after reading the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Authors’ information
DNAA: Is a pharmacist with an MSc degree in epidemiology and a PhD degree in pharmaceutical policy and access to medicines. He currently works with the Korle-Bu Teaching Hospital as the acting deputy director of pharmacy. DNAA is an HIV/AIDS adherence counselor and is interested in HIV/AIDS outcomes research. All the co-authors were his supervisors during his PhD studies.
Ethics approval and consent to participate
Anonymous data, with no identifiable information on participants were obtained from the data administrator. Permission to use data on HIV/AIDS patients in this facility was obtained from the Ethical and Protocol Review Committee of the University of Ghana Medical School in a related study by the same lead author. In particular, this was a PhD thesis and multiple studies were carried out using the same data. The studies did not involve any contact with patients and so there was no need to ask for patients’ consent to participate.
Consent for publication
Not applicable. We used only de-identified information. No identifiable details, no images or videos relating to any participant was used in this study.
Competing interests
The lead author and all the co-authors have nothing to declare with regards to this study.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Ankrah, D.N.A., Lartey, M., Mantel-Teeuwisse, A.K. et al. Five-year trends in treatment changes in an adult cohort of HIV/AIDS patients in Ghana: a retrospective cohort study. BMC Infect Dis 17, 664 (2017). https://doi.org/10.1186/s12879-017-2752-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-017-2752-7