Abstract
Background
Current antiretroviral therapy (ART) used to treat human immunodeficiency virus (HIV) patients is life-long because it only suppresses de novo infections. Recent efforts to eliminate HIV have tested the ability of a number of agents to reactivate (‘Kick’) the well-known latent reservoir. This approach is rooted in the assumption that once these cells are reactivated the host’s immune system itself will eliminate (‘Kill’) the virus. While many agents have been shown to reactivate large quantities of the latent reservoir, the impact on the size of the latent reservoir has been negligible. This suggests that the immune system is not sufficient to eliminate reactivated reservoirs. Thus, there is a need for more emphasis on ‘kill’ strategies in HIV cure research, and how these might work in combination with current or future kick strategies.
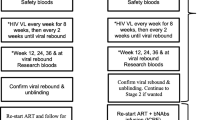
Methods
We conducted a landscape review of HIV ‘cure’ clinical trials using ‘kick and kill’ approaches. We identified and reviewed current available clinical trial results in human participants as well as ongoing and planned clinical trials. We dichotomized trials by whether they did not include or include a ‘kill’ agent. We extracted potential reasons why the ‘kill’ is missing from current ‘kick and kill’ strategies. We subsequently summarized and reviewed current ‘kill’ strategies have entered the phase of clinical trial testing in human participants and highlighted those with the greatest promise.
Results
The identified ‘kick’ trials only showed promise on surrogate measures activating latent T-cells, but did not show any positive effects on clinical ‘cure’ measures. Of the ‘kill’ agents currently being tested in clinical trials, early results have shown small but meaningful proportions of participants remaining off ART for several months with broadly neutralizing antibodies, as well as agents for regulating immune cell responses. A similar result was also recently observed in a trial combining a conventional ‘kick’ with a vaccine immune booster (‘kill’).
Conclusion
While an understanding of the efficacy of each individual component is crucial, no single ‘kick’ or ‘kill’ agent is likely to be a fully effective cure. Rather, the solution is likely found in a combination of multiple ‘kick and kill’ interventions.
Similar content being viewed by others
Introduction
Even though human Immunodeficiency virus (HIV) was identified as the cause of Acquired Immunodeficiency Syndrome (AIDS) over 30 years ago, we still do not have a general cure [1]. Of the estimated 71 million people infected to date, only one documented patient, the Berlin Patient, is believed to have been cured [2]. In this case, the cure was achieved by exploiting the radical measures required to treat the patient’s acute myeloid leukemia. While inspiring to cure enthusiasts, this approach is, however, not applicable to the broader population. Nevertheless, the case of the Berlin patient did propel new interest in curative HIV research approaches.
Most cure research efforts to date have been rooted in the so called “Kick and Kill” approach – an approach that is based on the premise the HIV virus partially ‘hides out’ in so-called latent reservoirs and that activating these latent reservoirs will result in the destruction of the reactivated cells either by attack by the immune system, or by the cytotoxic effects of HIV itself. To date, however, clinical trials employing kick and kill approaches have yet to deliver promising results.
In this article, we review what is currently known about viral transmission under antiretroviral therapy (ART) and the mechanisms underlying kick and kill approaches. We conclude that kick and kill has mainly focused on the ‘kick’ component and neglected the ‘kill’ component. We then review available strategies for the ‘kill’ component and summarize a potential approach to complete the kick and kill for effective therapy.
What is currently known about viral transmission, viral memory and ART?
Today, HIV/AIDS is a manageable, livable disease with many antiretroviral drugs available that safely and effectively suppress plasma viremia and maintain adequate peripheral blood CD4+ T-lymphocyte counts. However, effective treatment does not clear the virus infection, and its suppression requires lifelong treatment. This is because the current drugs impair the various stages of the viral lifecycle (viral entry to a target cell, reverse transcription, DNA integration, protein cleavage), but do not affect infected cells when these processes are not active. In general, when the immune system gains control over an infection, which is signalled by antigenic clearance, active inflammation and immunity diminish and a memory of specific immunity comprised of residual long-lived ‘antigenically committed’ memory T-cell remains. This memory can rapidly mount an anamnestic T-cell response upon re-exposure to familiar antigens. For HIV, the immune system never gains suppressive control of the infection or clearance of the virus. Rather, in the attempt to generate HIV-specific immunity, several of memory T-cells generated to ensure effective future immune responses remain infected because the active CD4+ T-cell from which they differentiated were already infected. Thus, a long-lived reservoir of HIV-infected memory T-cells is established. Most of these cells are not affected by current anti-retroviral therapies, and can hang around in significant numbers in an inactive, or quiescent state for decades with an estimated half-life of about 3½ years on ART [3, 4]. It has been estimated that systemically, there are somewhere in the range of 106–107 replication competent infected latent CD4+ T-lymphocytes, capable of rapidly re-establishing the viral population upon withdrawal of ART [5]. In addition, recent evidence that a significant proportion of clonally expanded memory T-cells are replication competent [4, 6, 7]. Memory T-cells are therefore considered to be the most important source of persistent infection.
From the perspective of HIV cure research, it is essential to keep in mind that other cell types can become infected by HIV. Particularly, monocytes and macrophages are thought to be of importance, as they have been shown to harbour large quantities of viral particles within intracellular endosomes [8,9,10,11]. These cells are long-lived (weeks to years), can infiltrate multiple tissue compartments including the central nervous system, are resistant to the cytolytic effects of HIV infection, can produce significant amounts of virus, and are believed be a key contributor of cell-to-cell transmission, even during ART [12,13,14,15]. In addition, the direct effects of ART treatment on macrophages is complex and not fully understood [16]. For example, a recent (April 2017) ex vivo study on 9 myeloid-only mice infected with M-tropic HIV and treated with 7 weeks of ART showed conventional viral rebound in 3 mice (33%) after interruption of ART [17]. However, this study does not explain the reason for viral rebound in 33% of the mice. Macrophage can be found in every tissue in the body as specialized subsets, and are not likely to receive uniform exposure to the drugs systemically. In the aforementioned study, there was a weak trend of a comparably lower number of macrophages in the spleen tissue and higher number of macrophages in the bone marrow among the 3 mice with viral rebound. However, larger sample sizes are required to validate this observation. Lastly, nucleoside reverse transcriptase inhibitors (NRTIs), non-nucleoside reverse transcriptase inhibitors (NNRTIs) and protease inhibitors (PIs) are less potent in these cells during chronic infection as determined by the half maximal effective concentration (EC50) and might be expected to be less suppressive.
Follicular dendritic cells, which are critical cells found in the B-cell follicles of the lymph nodes and other lymphoid tissues, are also considered to be an important viral reservoir. This is predominantly because they can shelter viral particles within endosomal compartments or carry multiple particles attached out outer membrane synapses. These particles can then be delivered to large populations of uninfected CD4+ T cells inside the lymph nodes, thus causing their infection and viral spread [18, 19]. While ART does reduce the viral titer within this reservoir, evidence suggests that viral clearance is not complete [20]. The contribution of these reservoirs to plasma viremia during natural infection or viral rebound when ART is interrupted is not known. Thus, we propose a focused evaluation of reservoirs would be important when studying cure approaches. At this point, we should acknowledge that research on viral reservoirs, whether latent memory T-cells, macrophages, or dendritic cells, presents several challenges due to the limited sensitivity of the assays and techniques currently available to quantify them. We therefore recommend this article be read in the light of this general limitation of HIV ‘cure’ research.
In the case of the Berlin patient, treatment for acute myeloid leukemia took place over several months and included lymphomyeloid ablative chemo- and radiation therapies, which are believed to have purged the patient’s T-cells [2]. As a result, two stem cell transplants were administered from a tissue compatible allogenic donor (to limit graft-versus-host disease) for immune system reconstitution. The donor of the bone marrow was electively selected to carry a homozygous delta32 deletion in CCR5 gene. During the treatment, a grade I level graft-versus-host disease was observed localized to the skin. Minor adjustments in cyclosporine modified and improved the disease and it is unclear if the graft-versus-host episode was a co-factor in the elimination of virus. While the precise mechanism by which the Berlin patient was cured is not clear, it is generally assumed that the above treatment led to the elimination of the vast majority (if not all) of this latent reservoir, as 10 years (February 2017) has not lapsed since ART was interrupted.
Kick and kill strategies to date
While there are many exciting cure strategies being pursued, the so called “Kick and Kill” approach has received the most attention. This approach is based on the premise that activating the latent reservoir will result in the destruction of the reactivated cells either by attack by the immune system, or by the activation-induced cell death associated with viral production in active CD4+ T-cells. At the same time, expansion of the infection is expected to be suppressed by concomitant administration of ART. Thus, it was believed that simply ‘kicking’ latent cells into activity might be enough to lead to the elimination of the latent reservoir. This is not a new idea. In fact, the first attempts at activating the reservoir were carried out over a decade ago and involved treatment with recombinant cytokines. For example, Interleukin 2 (IL-2) has been the subject of a number of studies in humans because of its ability to effect T-cell activation, proliferation and survival; however, the observed clinical effect at tolerable doses did not warrant further pursuit of these relatively toxic therapies [21, 22]. Since the first studies on cytokines, several sophisticated T-cell reservoir activation strategies leveraging our increasing knowledge of the mechanisms that preserve latency have been attempted. Two such approaches include: 1) treatments targeting the release of chemically sequestered cellular transcription factors essential to the initiation or propagation of viral transcription (e.g. NF-αB, NFAT, P-TEF, AP-1) and 2) epigenetic modulation of the HIV promotor site to favour HIV transcription. Below, the evidence on individual agents that fall within these two strategy categories are outlined. Further Table 1 presents and overview of ‘kick’ strategies that have been tested in clinical trials in humans to date.
Agents for targeting cellular transcription factors
With respect to ‘kick’ agents targeting cellular transcription factor, studies have included Protein Kinase C agonists (e.g. prostratin, bryostatins), which activate the canonical NF-αB pathway ultimately resulting in initiation of viral transcription [15, 23, 24]. However, these agents are generally toxic and clinical studies involving human participants have shown very little effect at tolerable doses [25]. Hexamethylene bisacetamide (HMBA) and Disulfram have been identified as affecting latency reversal by stimulating the release of positive transcription elongation factor b (P-TEFb) (from Hexim-1 and 7SK snRNA) via the Akt pathway [26,27,28,29]. P-TEFb catalyses phosphorylation of a number of transcriptional regulators at the HIV promotor site which support transcriptional initiation and elongation. Experiments with these pharmaceuticals in vitro showed promise, but two clinical trials of Disulfram in humans have yielded only a modest activation of the latent reservoir with indeterminate evidence of a reduction in the T-cell latent reservoir [30, 31]. To our knowledge, no future trials on disulfram are planned [32]. Interleukin (IL)-7 is required to stimulate homeostatic proliferation of resting memory T-cells, and it has therefore been hypothesized that IL-7 could potentially act as a latency reversing agent for resting infected CD4+ T-cells. To date, results in humans have been conflicting. One randomized placebo controlled dose-response trial adding recombinant human IL-7 to current ART in 32 patients with with low CD4+ T-cell counts (101–400 cells/mcg) showed an increase in thymic output, improved T-cell receptor repertoire, and increased cell cycling and bcl-2 expression [33]. By contrast, another randomized clinical trial combining IL-7 with raltegravir and maraviroc in 29 patients with CD4+ T-cell counts >350cells/mcg did not show any change in HIV DNA in peripheral blood mononuclear cells [34]. This negative finding is not surprising since other studies have shown that IL-7 contributes to viral persistence, leading to proliferation of infected cells and is not sufficient in reversing latency in quiescent T cells [35, 36]. Currently, one future IL-7 clinical trial is planned in which IL-7 will be combined with LIPO 5 DC, an experimental dendritic cell based therapeutic vaccine. Another class of agents, toll-like receptor (TLR) agonists, have been shown induce HIV expression and HIV specific immunity in patients receiving ART [32]. The latency reversing properties associated with the TLRs comprise activation via the NF-κB, NFAT, or AP-1 pathways [37, 38]. In addition, stimulation of TLR-7 have been shown effective as an adjuvant to therapeutic vaccination in SIV-infected rhesus monkeys [39]. Currently, one single arm (phase I) clinical trial has investigated TLR-agonists, namely the novel MGN1703 TLR-9 agonist in 15 virologically suppressed HIV infected individuals [40]. In this trial, CD8+ T-cells and natural killer (NK) cells significantly increased during treatment, thus suggesting enhanced immune response to the virus. In 6 of the 16 participants viral RNA copies also increased from <20 to >1500 copies/mL, potentially suggesting re-activation of the latent reservoir. Two more clinical trials are being planned to investigate the latency reversing effects of TLR agonists [32].
Epigenetic modulation agents
In the case of epigenetic modulation, the histone deacetylase (HDAC) inhibitors are the most studied pharmaceutical agents to reactivate the latent reservoir. These studies have received comprehensive review by others [41, 42]. Briefly, in the latent state, HDAC enzymes accumulate around the HIV promotor site favouring deacetylation of the associated nucleosomes and hence restricting HIV replication. Researchers have demonstrated a number of different HDAC inhibitors (e.g. valproic acid, vorinostat, panobinostat, Romidepsin, suberoyl bis-hydroxamic acid) stimulate transcription, thus activating the latent cells both in vitro and in vivo. In clinical trials, however, treatment with these agents resulted in no significant reduction of the latent viral reservoir of memory T-cells although there was evidence that infected cells were being activated (see Table 1). Despite disappointing results in these early clinical trials, a total of nine trials examining these agents, either alone or in combination with immune boosters, are planned or ongoing [32].
Another class of compounds that have been examined as latency reversing agents include Histone methyl transferase inhibitors (chaetocin and BIX-01294) [43, 44]. These agents affect histone methylation and/or demethylation stimulating or repressing transcription in a manner akin to the deactylase inhibitors. Also, the DNA cytosine demethylation agent 5-aza-2-deoxycytidine (Aza-CdR) can reverse latency by demethylating CpG islands Regions of DNA usually found near gene promotor sites with high density of cytosine-phosphate-guanine (CpG) clusters in the HIV transcription initiation site [45]. All these agents have been shown to reverse latency in vitro and/or ex vivo, but have not been tested in vivo as far as we are aware [43,44,45].
The missing ‘kill’ in ‘kick and kill’
While there are a number of factors that might explain the failure of the latency reversal agents to meaningfully impact the T-cell reservoir in initial studies, it is important to recognize that the entire kick and kill paradigm is based on the premise that latently infected cells will either expire due to virus induced lysis/apoptosis or be destroyed by cytotoxic T-cell (CTL) response soon after activation. Recent evidence, however, suggests that this may not be the case [35, 46, 47]. For example, in one study of latency reversal in CD4+ T-cells obtained from HIV-infected donors, Shan and colleagues found that reactivation of latent infected cells by the HDAC inhibitor vorinostat did not affect the reservoir [47]. Furthermore, the addition of CD8+ T cells from patients on suppressive ART did not induce cell death. Another study suggested that the HDAC inhibitors in general may suppress the CTL response. In particular, it was observed that vorinostat, panobinostat and romidepsin impaired the ability of HIV-specific CTL to eliminate infected CD4+ T-cells ex vivo [46]. Other data suggest that the vigorous CTL response observed during acute infection may be lost during chronic infection, and thus, that CTL response might be impaired independent of administration of HDAC inhibitors [48]. Collectively, these observations suggest that ‘Kicking’ alone is likely insufficient to eliminate the latent T-cell reservoir.
Another limitation of current kick and kill clinical studies is the almost ubiquitous focus on T-cell reservoirs. By now, it has been well-document that several other secondary reservoirs may be a key contributor to the persistence of the HIV virus. To this end, we have already discussed the likely significant role that monocytes and macrophages play in the persistence of the HIV virus. As these cells are known to be relatively resistant to the cytopathic effect of the HIV infection, stimulating them may only serve to increase the production of virions and/or associated viral proteins. Another latent reservoir that is believed to sustain viral transmission during ART are the dendritic cells. Dendritic cells can shelter viral particles within endosomal compartments or carry multiple particles attached out outer membrane synapses. Dendritic cells can live for several years, during which they can slowly gather increasing amounts of viral particles [49]. To our knowledge, interaction of latency reversing agents and dendritic cells has not been explored. However, since dendritic cells generally do not integrate or replicate viral RNA, latency reversing agents are not expected to affect dendritic cells. Although controversy still exists on the importance of dendritic cells as a component of the latent reservoir, with our current understanding, one could argue a feasible and efficient kill strategy targeting dendritic cells might be essential in attaining a cure.
Kill strategies
With recent results suggesting the simple reversal of latency (kick) strategy to be insufficient for purging the latent reservoir, it is time to look more closely at approaches that focus on killing reactivated cells. Such agents might have the potential to act directly on latent cells removing the need for the latency reversing drug. Here, we look at some approaches that focus on ‘the Kill.’
Broadly neutralizing monoclonal antibodies
Application of broadly neutralizing monoclonal antibodies (mAb) for prevention, post exposure prophylaxis and the treatment of HIV have has been increasingly pursued since the advent of single cell based cloning methods has made isolation of mAb against the virus mainstream [50,51,52,53]. These proteins target the virus envelope proteins composed of multiple HIV gp120 surface proteins coupled to gp41 transmembrane proteins. For treatment purposes, there are numerous mAb being studied; some exhibiting significant breadth and potency against hundreds of HIV variants [54, 55]. Fig. 1 illustrate the general mechanism of action associated with broadly neutralizing monoclonal antibodies for the treatment of HIV. To date, two of these have advanced to clinical trials in human participants. In the first case, administration of a single dose (30 mg/kg) of 3BNC117 (which targets the CD4+ binding site of the viral spike) to viremic subjects (N = 17, 2 on ART) resulted in a 0.8–2.5 log10 decrease in viremia which persisted for 28 days [56]. Similarly, six of eight subjects treated with the CD4+ blocking monoclonal VRC01 (40 mg/kg, IV) experienced a 1.1 to 1.8 log10 reduction in plasma viremia. In this latter case, the two non-responders were shown to be infected with resistant variants prior to treatment. This observation highlights the importance that resistance avoidance will be critical if these therapies are to be successful. In both trials, resistant viral variants emerged in at least some patients after clearance of the antibodies. Further, studies in animal models indicate changes in just one to three target protein residues is enough to allow for viral escape [54]. Thus, as it is with ART, combinations of mAbs targeting different epitopes will likely be required for clinical application and early studies both in vitro and in animal models suggest that this could be a viable approach [57, 58].
Until recently, the primary focus of studies around the therapeutic use of mAb for HIV has been on active infection and the ability of mAbs to block viral infiltration into cells. However, these agents also have potential to orchestrate the destruction of the latent reservoir via antibody-dependent cell-mediated cytotoxicity (ADCC) [59]. ADCC is mediated by the antibody Fc chain which can recruit natural killer (NK) cells, macrophages, polymorphonuclear phagocytes or complement. Recent studies suggest that some of the broadly neutralizing mAb appear to direct ADCC in latent HIV-infected T-cells [60]. This has been demonstrated in vitro with multiple broadly neutralizing mAbs (including 3BNC117 and VRC01) where research demonstrated varying degrees of ADCC in laboratory strains (CD4+ lymphoid cells (MT4) infected with the prototypic R5-tropic NLAD8 or X4-tropic NL4.3) and primary HIV isolates. Of the mAbs tested in laboratory strains, 5 strongly induced ADCC (NIH45–46, 3BNC117, 10–1074, PGT121, 10E8), two less so (PG16, VRC01) with the balance being inactive. With respect to primary HIV isolates obtained from infected patients, the effect was somewhat attenuated requiring a combination of 5 mAbs (NIH45–46, 3BNC117, 10–1074, PG16 and 10E8, each at 1.5 mg ml) to induce cell death in some but not all strains. The reduced activity was associated with a reduced number of available binding sites in the infected cells. Interestingly, the same combination of five mAbs induced cell death ex vivo in reactivated (by phytohemagglutinin PHA) latent CD4+ isolates obtained from 5 out of 6 ART suppressed HIV infected subjects.
Direct in vivo studies of mAb induced ADCC are limited to animal models [60, 61]. In a study of HIV infected (HIV-1YU2) humanized mice, researchers found that animals treated with mAb mixture (3BNC117, 10–1074, and PG16) were slower to rebound upon withdrawal of treatment relative to ART treated mice (74–107 days vs 28–84 days) [60]. This finding was interpreted as an indication of a reduced latent reservoir mediated via Fc mediated ADCC [54]. This was supported using the same combination of mAb, but with the Fc effector function removed. Here, nine of 15 of the mice on the knock out regimen rebounded within 44 days after cessation of therapy relative to 1 of 21 mice receiving the unmutated mAb (p = 0.0004). Further, rebound viremia was 50-fold higher in the mice on the knock out mAb (p = 0001).
In humans, evidence of ADCC is indirect. Results from the RV144 trial vaccine trial showed a 31% reduction in HIV acquisition (P = 0.04), however, the antibodies induced by the vaccine did not suppress primary HIV isolates and it was therefore theorized that the observed effect might be associated with ADCC [62]. Modelling studies of passively administered 3BNC117 also suggest that the observed results cannot be attributed to clearance of free virus alone and that Fc mediated ADCC likely a contributing factor [61]. Taken together all these results suggest that addition of mAbs to the kick and kill strategies deserve investigation.
Integrin receptor targeted antibody therapy
In a recent report, an antibody therapy targeting CD4+ T-cell proteins appeared to confer impressive viral control in primates recently infected with Simian immunodeficiency virus (SIV) [63]. In this study, ART-treated SIV-infected rhesus macaques received eight infusions of a primatized monoclonal antibody against the α4β7 integrin both during ART, and for a period after discontinuing ART. After cessation of ART, all eight test animals achieved viral control (low to undetectable levels) after a period of modest viral rebound (note: 2 of 8 never exhibited rebound). Virologic control was sustained for over 45 weeks after discontinuing ART. This is in contrast to the seven macaques in the control arm (which received nonspecific rhesus immunoglobulin G instead of α4β7 mAb) where all the animals rebounded to high viral loads (6 logs) within 2 weeks of stopping ART. Furthermore, CD4+ T-cell counts recovered to ‘healthy’ levels in the α4β7 mAb treated animals soon after the first administration of the antibody and remained stable for over 25 weeks off all therapy. There was no recovery in the controls.
The mechanism for the observed effect of the anti-α4β7 integrin in this study is not entirely clear. The α4β7 integrin is a CD4 cell surface protein that is instrumental in the trafficking of these cells to the gastrointestinal tissue. During acute infection, a great deal of damage occurs in the gastrointestinal tissue including a precipitous drop in CD4+ T-cells, damage to the intestinal epithelium and the rapid establishment of the viral reservoir. It was believed that limiting access of CD4+ T-cells to the gut with the anti-α4β7 might mitigate this damage. Whether that explains the results can not be determined from this study as CD4+ counts in the small intestine began to recover during the period of administration of the anti-α4β7. Another potential mechanism may be the property that anti-α4β7 monoclonal antibodies allow for the production of anti-v2 antibodies, which have been shown to mediate antibody-dependent cellular phagocytosis (ADCP), and thus contribute to the suppression of the proliferation of infected cells [64]. Collectively, the observations of this study may be important to cure research although it is not clear if they would extend to later stages of disease.
BiTEs and DARTs
Bispecific T-cell Engagers (BiTEs) and Dual-Affinity Re-targeting Molecules (DARTS) are variations of bispecific antibodies, which are engineered with the binding regions of two different antibodies such that they bind two different antigens. Both BITEs and DARTs belong to a class of these compounds which exclude the antibody Fc region. Progress in the use of these agents for the treatment of cancer has recently spurred research in their application to the treatment of HIV-1.
BiTEs are comprised of two antibody single chain variable fragments linked together by a short flexible peptide [65]. One fragment is targeted towards CD3 protein of the T-cell receptor complex which signals T-cell effector functions. In a recent study of a BiTE incorporating the light chain of the broadly neutralizing antibody VRC07, researchers found that the resulting VRC07-CD3 BiTE induced CTL elimination of latently infected cells isolated from peripheral blood mononuclear cells (PBMCs) of infected donors ex vivo [66]. Fig. 2 illustrates, in brief, the assembly process and the general mechanism of action associated with BiTEs for the treatment of HIV.
Assembly of BiTEs from two different variable regions of monoclonal antibodies and their mechanism of action. The BiTE first attaches to a CD8+ T cell before assisting the CD8+ T cell in binding to an HIV infected CD4+ T cell. Upon binding the CD4+ T cell the CD8+ T cell will release granzymes and induce death of the HIV infected CD4+ T cell
In subtle contrast to BiTEs, DARTs are constructed from the variable heavy domain of one antibody linked to the light variable domain of another [55]. DART proteins have shown to mediate CTL clearance of latently infected CD4+ T-cells both in vitro and ex vivo [67, 68]. Thus, proof-of-concept of these agents as potential kill agents seems to have been met. It will be interesting if these results can be recapitulated in vivo.
Chimeric antigen receptors (CARs)
Another class of kill agents with renewed excitement are HIV specific T-cells engineered with chimeric antigen receptors (CARs) [69]. CAR receptors are comprised of a target specific surface protein coupled to an intracellular signalling domain to activate the cytotoxic response. The first CAR was based on a soluble CD4+ receptor (intended to bind to infected cells expressing HIV gp120) coupled to an intracellular CD3 ζ signalling protein. In vitro, these designer cells were as effective at killing infected cells and CTL clones isolated from infected patients [70]. Unfortunately, when tested on HIV infected subjects, they had no effect on clinical outcomes (although they were well tolerated and persisted for years). Because of this, CAR research was abandoned. However, recent progress in treatment of cancer with CARs coupled with the discovery of broadly neutralizing antibodies (which serve as CAR receptor models) has renewed interest in their application to HIV renewed [71]. In vitro, these antibody-modelled CARs show promise, but it remains to be seen if they will be effective in vivo. Fig. 3 illustrates the assembly of a CAR engineered T cell and the general mechanism of action associated with CARs for the treatment of HIV.
Second mitochondria-derived activator of Caspases
Second Mitochondria-derived Activator of Caspases (SMAC) mimetics are small molecule drugs that show potential to induce cell death in reactivated latent cells. Caspases are proteolytic enzymes involved in apoptosis and IAPs (Inhibitors of Apoptosis Protein) are regulatory proteins that inhibit caspase activity by either binding directly to the enzyme (e.g. XIAP) or by blocking signals that lead to their activation (e.g. IAP2, IAP3). SMAC is an endogenous protein that suppresses the activity of the IAPs thus promoting cell death. Several small molecule drugs fashioned after the key binding domain of SMAC have been developed to combat apoptosis resistant cancer cells with some already entering clinical trials [72]. While studies are still in the early stages, researchers are currently exploring these agents to eliminate the HIV latent reservoir. In a recent report, in vitro treatment of HIV infected central memory T-cells with 3 SMAC mimetics (birinapant, GDC-0152 and emblin) targeting XIAP activity successfully induced a significant dose-dependent increase in apoptosis [73].
Another study of SMAC mimetics demonstrated latency reversing abilities by looking at SMAC inhibitors of IAP1 and IAP2, two proteins that are known to inhibit NF-κB inducing Kinase (NIK) by ubiquitination. In the absence of IAP1 and IAP2, NIK will accumulate, initiating a series of reactions that result in the activation of NF-κB which can translocate to the nucleus and initiate HIV transcription. Researchers tested four SMAC mimetics (SBI-0637142, LCL161, GDC-0152, TL32711) specifically targeting IAP1 and/or IAP2 and all exhibited latency reversing capacity in a Jurkat latency model [74]. SBI-0637142 and LCL161 were also tested ex vivo in CD4+ T-cells collected from HIV patients on suppressive ART, and while neither seemed to initiate activation of these cells on their own, there was a potent synergistic effect when they were used in combination with the HDAC inhibitor panobinostat. Taken together, these results suggest an exciting potential for SMAC mimetics in kick and kill strategies.
Immune checkpoint antibodies
The role of programmed cell death receptor 1 (PD-1) and PD1 ligand (PD-L1) expression in HIV patients have been investigated in several studies [75]. Elevated expression of PD1 has been demonstrated in both HIV specific CD8+ T cells and CD4+ T-cells. In particular, the interaction of PD-1 and PD-L1 are suspected to be a major contributor to the persistence of infected CD4+ T-cells [76]. High PD1 expression has been shown correlated with the exhaustion of CD8+ T-cells [77]. Antibodies for PD-L1 ligand have been developed for several late stage cancers and these have shown effective in inducing natural apoptosis and increasing overall survival. Case studies of cancer patients with HIV receiving PD-L1 antibodies have also reported promising results such as substantial lowering of viral loads [78]. Given the promise of these early results, clinical trials have been initiated. In one completed 8-person phase trial (6 patients receiving one infusion of nivolimumab 0.3 mg/kg, 2 patients receiving normal saline as placebo), two of the nivolimumab treated patients showed evidence of reversal of CD8+ T-cell exhaustion 4 weeks after the infusion [79]. Two larger trials are currently ongoing [32].
Therapeutic vaccination
While most vaccine research has focussed on prevention, numerous clinical studies of therapeutic vaccines in HIV infected subjects have been conducted [80, 81]. Some of these have shown modest drops in viral load (0.5 to 1 log drop) using various approaches to boost the immune system, and thus, can arguably be considered ‘kick’ strategies. For example, in the single arm REDUC study, subjects received multiple doses of Vacc-4× (a synthetic gag peptide) with recombinant humanized granulocyte macrophage colony-stimulating factor (rhu-GM-CSF) followed by administration of the HDAC inhibitor romidepsin [82]. The rationale for this study was based on previous data that suggested the Vacc-4×/rhu-GM-CSF vaccine induced killing of infected cells. While the results of the treatment showed a significant (p = 0.01) 40% reduction in the proviral DNA, it did not have any effect in time to rebound after treatment interruption. Researchers concluded the treatment required fine tuning. Another vaccine trial, the BCN01 trial, suggested that a combination of the ChAd.HIVconsv and the MVA.HIVconsv prime boost vaccines are efficacious in redirecting CD8+ T-cell response towards regions where HIV-1 is highly conserved [83]. Further, a recent extension study of BCN01, the BCN02 proof-of-concept study, in which another boost with MVA.HIVconsv was followed by three weekly 5 mg/m2 doses of romdepsin and a second MVA.HIVconsv boost, demonstrated highly promising results as an therapeutic strategy that encompasses both a kick and a kill component [84]. Of the 15 patients enrolled in this proof-of-concept study, the most recently presented data (CROI, February 2017) revealed that four patients have remained off ART for 7, 12, 14, and 22, weeks respectively. Longer term follow-up results cast further light on the efficacy of this therapeutic combination.
Conclusions
For patients, clinicians and healthcare funders alike, developing a sterilizing HIV cure which completely clears the virus would be the ultimate goal. However, a ‘functional cure’ that would allow the body to control the virus in the absence of other treatments (i.e. ART) for a considerable duration of time is generally considered more realistic. A functional cure would provide much needed relief to patients on rigorous daily antiretroviral regimens. Further, it would likely have a greater impact than conventional ART in settings where adherence or frequent access to medication presents a challenge. ‘Kick and kill’ cure approaches have taken the lead in cure research, but to date results have been disappointing. This may stem from the fact that previous approaches have not taken full advantage of available kill approaches, and thus missed out on the opportunity to kill a sufficient quantity of re-activated cells or even the resting cells themselves. Here we have reviewed five kill approaches that show potential to reduce or eliminate the latent reservoir. These might be used alone, in combination with each other and/or in combination with latency reversing agents. Given the complexity of HIV infection and the multiplicity of compartments (cellular and tissue) involved, it seems highly unlikely that there will be a single ‘magic cure bullet’. Instead, the cure is almost certainly going to require a multipronged approach involving new drug combinations. While an understanding of the efficacy and safety of each potential component is crucial, we believe it is paramount that future research includes an additional focus on finding the best combination of therapies to clear infected cells.
Abbreviations
- ADCC:
-
Antibody-dependent cell-mediated cytotoxicity
- AIDS:
-
Acquired Immunodeficiency Syndrome
- ART:
-
Antiretroviral therapy
- BITE:
-
Bispecific T-cell Engagers
- CAR:
-
Chimeric antigen receptors
- CTL:
-
Cytotoxic T-cell
- DARTS:
-
Dual-Affinity Re-targeting Molecules
- EC50 :
-
Half maximal effective concentration
- HDAC:
-
Histone deacetylase
- HIV:
-
Human immunodeficiency virus
- II:
-
Integrase inhibitors
- IL:
-
Interleukin
- mAb:
-
Monoclonal Antibody
- NNRTI:
-
Non-nucleoside reverse transcriptase inhibitors
- NRTI:
-
Nucleoside reverse transcriptase inhibitors
- PD1:
-
Programmed cell death receptor 1
- PD-L1:
-
PD1 ligand
- PI:
-
Protease inhibitors
- P-TEFb:
-
Positive transcription elongation factor b
- SIV:
-
Simian immunodeficiency virus
- SMAC:
-
Second Mitochondria-derived Activator of Caspases
- TLR:
-
Toll-like receptor
References
Barre-Sinoussi F, Chermann JC, Rey F, Nugeyre MT, Chamaret S, Gruest J, et al. Isolation of a T-lymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS). Science. 1983;220(4599):868–71.
Hutter G, Nowak D, Mossner M, Ganepola S, Mussig A, Allers K, et al. Long-term control of HIV by CCR5 Delta32/Delta32 stem-cell transplantation. N Engl J Med. 2009;360(7):692–8.
Siliciano JD, Kajdas J, Finzi D, Quinn TC, Chadwick K, Margolick JB, et al. Long-term follow-up studies confirm the stability of the latent reservoir for HIV-1 in resting CD4+ T cells. Nat Med. 2003;9(6):727–8.
Maldarelli F, Wu X, Su L, Simonetti FR, Shao W, Hill S, et al. HIV latency. Specific HIV integration sites are linked to clonal expansion and persistence of infected cells. Science. 2014;345(6193):179–83.
Eriksson S, Graf EH, Dahl V, Strain MC, Yukl SA, Lysenko ES, et al. Comparative analysis of measures of viral reservoirs in HIV-1 eradication studies. PLoS Pathog. 2013;9(2):e1003174.
Hosmane NN, Kwon KJ, Bruner KM, Capoferri AA, Beg S, Rosenbloom DI, et al. Proliferation of latently infected CD4+ T cells carrying replication-competent HIV-1: potential role in latent reservoir dynamics. J Exp Med. 2017;214(4):959–72.
Simonetti FR, Sobolewski MD, Fyne E, Shao W, Spindler J, Hattori J, et al. Clonally expanded CD4+ T cells can produce infectious HIV-1 in vivo. Proc Natl Acad Sci U S A. 2016;113(7):1883–8.
Hassan J, Browne K, De Gascun C. HIV-1 in Monocytes and macrophages: an overlooked reservoir? Viral Immunol. 2016;29(9):532–3.
Benaroch P, Billard E, Gaudin R, Schindler M, Jouve M. HIV-1 assembly in macrophages. Retrovirology. 2010;7:29.
Carter CA, Ehrlich LS. Cell biology of HIV-1 infection of macrophages. Annu Rev Microbiol. 2008;62:425–43.
Campbell JH, Hearps AC, Martin GE, Williams KC, Crowe SM. The importance of monocytes and macrophages in HIV pathogenesis, treatment, and cure. AIDS. 2014;28(15):2175–87.
Orenstein JM, Fox C, Wahl SM. Macrophages as a source of HIV during opportunistic infections. Science. 1997;276(5320):1857–61.
Archin NM, Espeseth A, Parker D, Cheema M, Hazuda D, Margolis DM. Expression of latent HIV induced by the potent HDAC inhibitor suberoylanilide hydroxamic acid. AIDS Res Hum Retrovir. 2009;25(2):207–12.
Archin NM, Liberty AL, Kashuba AD, Choudhary SK, Kuruc JD, Crooks AM, et al. Administration of vorinostat disrupts HIV-1 latency in patients on antiretroviral therapy. Nature. 2012;487(7408):482–5.
Kulkosky J, Culnan DM, Roman J, Dornadula G, Schnell M, Boyd MR, et al. Prostratin: activation of latent HIV-1 expression suggests a potential inductive adjuvant therapy for HAART. Blood. 2001;98(10):3006–15.
Gavegnano C, Schinazi RF. Antiretroviral therapy in macrophages: implication for HIV eradication. Antivir Chem Chemother. 2009;20(2):63–78.
Honeycutt JB, Thayer WO, Baker CE, Ribeiro RM, Lada SM, Cao Y, et al. HIV persistence in tissue macrophages of humanized myeloid-only mice during antiretroviral therapy. Nat Med. 2017;23(5):638–43.
Heesters BA, Lindqvist M, Vagefi PA, Scully EP, Schildberg FA, Altfeld M, et al. Follicular Dendritic cells retain infectious HIV in cycling Endosomes. PLoS Pathog. 2015;11(12):e1005285.
Spiegel H, Herbst H, Niedobitek G, Foss HD, Stein H. Follicular dendritic cells are a major reservoir for human immunodeficiency virus type 1 in lymphoid tissues facilitating infection of CD4+ T-helper cells. Am J Pathol. 1992;140(1):15–22.
Carroll MC. Are follicular dendritic cells a reservoir for HIV? Abstract 127 Session S-7. Boston, MA: Conference on Retroviruses and Opportunistic Infections (CROI); 2016.
Lafeuillade A, Poggi C, Chadapaud S, Hittinger G, Chouraqui M, Pisapia M, et al. Pilot study of a combination of highly active antiretroviral therapy and cytokines to induce HIV-1 remission. J Acquir Immune Defic Syndr. 2001;26(1):44–55.
Prins JM, Jurriaans S, van Praag RM, Blaak H, van Rij R, Schellekens PT, et al. Immuno-activation with anti-CD3 and recombinant human IL-2 in HIV-1-infected patients on potent antiretroviral therapy. AIDS. 1999;13(17):2405–10.
Korin YD, Brooks DG, Brown S, Korotzer A, Zack JA. Effects of prostratin on T-cell activation and human immunodeficiency virus latency. J Virol. 2002;76(16):8118–23.
Mehla R, Bivalkar-Mehla S, Zhang R, Handy I, Albrecht H, Giri S, et al. Bryostatin modulates latent HIV-1 infection via PKC and AMPK signaling but inhibits acute infection in a receptor independent manner. PLoS One. 2010;5(6):e11160.
Gutierrez C, Serrano-Villar S, Madrid-Elena N, Perez-Elias MJ, Martin ME, Barbas C, et al. Bryostatin-1 for latent virus reactivation in HIV-infected patients on antiretroviral therapy. AIDS. 2016;30(9):1385–92.
Choudhary SK, Archin NM, Margolis DM. Hexamethylbisacetamide and disruption of human immunodeficiency virus type 1 latency in CD4(+) T cells. J Infect Dis. 2008;197(8):1162–70.
Contreras X, Barboric M, Lenasi T, Peterlin BM. HMBA releases P-TEFb from HEXIM1 and 7SK snRNA via PI3K/Akt and activates HIV transcription. PLoS Pathog. 2007;3(10):1459–69.
Doyon G, Zerbato J, Mellors JW, Sluis-Cremer N. Disulfiram reactivates latent HIV-1 expression through depletion of the phosphatase and tensin homolog. AIDS. 2013;27(2):F7–F11.
Xing S, Bullen CK, Shroff NS, Shan L, Yang HC, Manucci JL, et al. Disulfiram reactivates latent HIV-1 in a Bcl-2-transduced primary CD4+ T cell model without inducing global T cell activation. J Virol. 2011;85(12):6060–4.
Elliott JH, McMahon JH, Chang CC, Lee SA, Hartogensis W, Bumpus N, et al. Short-term administration of disulfiram for reversal of latent HIV infection: a phase 2 dose-escalation study. Lancet HIV. 2015;2(12):e520–9.
Spivak AM, Andrade A, Eisele E, Hoh R, Bacchetti P, Bumpus NN, et al. A pilot study assessing the safety and latency-reversing activity of disulfiram in HIV-1-infected adults on antiretroviral therapy. Clin Infect Dis. 2014;58(6):883–90.
Delagreverie HM, Delaugerre C, Lewin SR, Deeks SG, Li JZ. Ongoing clinical trials of human immunodeficiency virus latency-reversing and Immunomodulatory agents. Open Forum Infect Dis. 2016;3(4):ofw189.
Levy Y, Sereti I, Tambussi G, Routy JP, Lelievre JD, Delfraissy JF, et al. Effects of recombinant human interleukin 7 on T-cell recovery and thymic output in HIV-infected patients receiving antiretroviral therapy: results of a phase I/IIa randomized, placebo-controlled, multicenter study. Clin Infect Dis. 2012;55(2):291–300.
Katlama C, Lambert-Niclot S, Assoumou L, Papagno L, Lecardonnel F, Zoorob R, et al. Treatment intensification followed by interleukin-7 reactivates HIV without reducing total HIV DNA: a randomized trial. AIDS. 2016;30(2):221–30.
Bosque A, Famiglietti M, Weyrich AS, Goulston C, Planelles V. Homeostatic proliferation fails to efficiently reactivate HIV-1 latently infected central memory CD4+ T cells. PLoS Pathog. 2011;7(10):e1002288.
Vandergeeten C, Fromentin R, DaFonseca S, Lawani MB, Sereti I, Lederman MM, et al. Interleukin-7 promotes HIV persistence during antiretroviral therapy. Blood. 2013;121(21):4321–9.
Novis CL, Archin NM, Buzon MJ, Verdin E, Round JL, Lichterfeld M, et al. Reactivation of latent HIV-1 in central memory CD4(+) T cells through TLR-1/2 stimulation. Retrovirology. 2013;10:119.
Tsai A, Irrinki A, Kaur J, Cihlar T, Kukolj G, Sloan DD, et al. Toll-like receptor 7 agonist GS-9620 induces HIV expression and HIV-specific immunity in cells from HIV-infected individuals on suppressive antiretroviral therapy. J Virol. 2017;91(8):e02166–16.
Borducchi EN, Cabral C, Stephenson KE, Liu J, Abbink P, Ng'ang'a D, et al. Ad26/MVA therapeutic vaccination with TLR7 stimulation in SIV-infected rhesus monkeys. Nature. 2016;540(7632):284–7.
Vibholm L, Schleimann MH, Hojen JF, Benfield T, Offersen R, Rasmussen K, et al. Short-course toll-like receptor 9 agonist treatment impacts innate immunity and plasma Viremia in individuals with human immunodeficiency virus infection. Clin Infect Dis. 2017;64(12):1686–95.
Shirakawa K, Chavez L, Hakre S, Calvanese V, Verdin E. Reactivation of latent HIV by histone deacetylase inhibitors. Trends Microbiol. 2013;21(6):277–85.
Wightman F, Ellenberg P, Churchill M, Lewin SR. HDAC inhibitors in HIV. Immunol Cell Biol. 2012;90(1):47–54.
Bouchata S, Gatota J, Kabeya K, Cardona C, Colin L, Herbein G, et al. Histone methyltransferase inhibitors induce HIV-1 recovery in resting CD4R T cells from HIV-1-infected HAART-treated patients. AIDS. 2012;26:12.
Friedman J, Cho WK, Chu CK, Keedy KS, Archin NM, Margolis DM, et al. Epigenetic silencing of HIV-1 by the histone H3 lysine 27 methyltransferase enhancer of Zeste 2. J Virol. 2011;85(17):9078–89.
Blazkova J, Trejbalova K, Gondois-Rey F, Halfon P, Philibert P, Guiguen A, et al. CpG methylation controls reactivation of HIV from latency. PLoS Pathog. 2009;5(8):e1000554.
Jones RB, O'Connor R, Mueller S, Foley M, Szeto GL, Karel D, et al. Histone deacetylase inhibitors impair the elimination of HIV-infected cells by cytotoxic T-lymphocytes. PLoS Pathog. 2014;10(8):e1004287.
Shan L, Deng K, Shroff NS, Durand CM, Rabi SA, Yang HC, et al. Stimulation of HIV-1-specific cytolytic T lymphocytes facilitates elimination of latent viral reservoir after virus reactivation. Immunity. 2012;36(3):491–501.
Walker BD. Bernard fields lecture: T cell control of HIV: implications for vaccines and cure. Boston: CROI 2016; 2016.
Zhang J, Perelson AS. Contribution of follicular dendritic cells to persistent HIV viremia. J Virol. 2013;87(14):7893–901.
Hessell AJ, Jaworski JP, Epson E, Matsuda K, Pandey S, Kahl C, et al. Early short-term treatment with neutralizing human monoclonal antibodies halts SHIV infection in infant macaques. Nat Med. 2016;22(4):362–8.
Hessell AJ, Poignard P, Hunter M, Hangartner L, Tehrani DM, Bleeker WK, et al. Effective, low-titer antibody protection against low-dose repeated mucosal SHIV challenge in macaques. Nat Med. 2009;15(8):951–4.
Scheid JF, Mouquet H, Feldhahn N, Walker BD, Pereyra F, Cutrell E, et al. A method for identification of HIV gp140 binding memory B cells in human blood. J Immunol Methods. 2009;343(2):65–7.
Tiller T, Meffre E, Yurasov S, Tsuiji M, Nussenzweig MC, Wardemann H. Efficient generation of monoclonal antibodies from single human B cells by single cell RT-PCR and expression vector cloning. J Immunol Methods. 2008;329(1–2):112–24.
Halper-Stromberg A, Nussenzweig MC. Towards HIV-1 remission: potential roles for broadly neutralizing antibodies. J Clin Invest. 2016;126(2):415–23.
Mascola JR. Harnessing antibodies for HIV-1 prevention and treatment. Boston: CROI 2016; 2016.
Caskey M, Klein F, Lorenzi JC, Seaman MS, West AP Jr, Buckley N, et al. Viraemia suppressed in HIV-1-infected humans by broadly neutralizing antibody 3BNC117. Nature. 2015;522(7557):487–91.
Horwitz JA, Halper-Stromberg A, Mouquet H, Gitlin AD, Tretiakova A, Eisenreich TR, et al. HIV-1 suppression and durable control by combining single broadly neutralizing antibodies and antiretroviral drugs in humanized mice. Proc Natl Acad Sci U S A. 2013;110(41):16538–43.
Wagh K, Bhattacharya T, Williamson C, Robles A, Bayne M, Garrity J, et al. Optimal combinations of broadly neutralizing antibodies for prevention and treatment of HIV-1 Clade C infection. PLoS Pathog. 2016;12(3):e1005520.
Bruel T, Guivel-Benhassine F, Amraoui S, Malbec M, Richard L, Bourdic K, et al. Elimination of HIV-1-infected cells by broadly neutralizing antibodies. Nat Commun. 2016;7:10844.
Halper-Stromberg A, Lu CL, Klein F, Horwitz JA, Bournazos S, Nogueira L, et al. Broadly neutralizing antibodies and viral inducers decrease rebound from HIV-1 latent reservoirs in humanized mice. Cell. 2014;158(5):989–99.
Lu CL, Murakowski DK, Bournazos S, Schoofs T, Sarkar D, Halper-Stromberg A, et al. Enhanced clearance of HIV-1-infected cells by broadly neutralizing antibodies against HIV-1 in vivo. Science. 2016;352(6288):1001–4.
Klein F, Mouquet H, Dosenovic P, Scheid JF, Scharf L, Nussenzweig MC. Antibodies in HIV-1 vaccine development and therapy. Science. 2013;341(6151):1199–204.
Byrareddy SN, Arthos J, Cicala C, Villinger F, Ortiz KT, Little D, et al. Sustained virologic control in SIV+ macaques after antiretroviral and alpha4beta7 antibody therapy. Science. 2016;354(6309):197–202.
Musich T, Li L, Liu L, Zolla-Pazner S, Robert-Guroff M, Gorny MK. Monoclonal antibodies specific for the V2, V3, CD4-binding site, and gp41 of HIV-1 mediate Phagocytosis in a dose-dependent manner. J Virol. 2017;91(8):e02325–16.
Kontermann RE, Brinkmann U. Bispecific antibodies. Drug Discov Today. 2015;20(7):838–47.
Pegu A, Asokan M, Wu L, Wang K, Hataye J, Casazza JP, et al. Activation and lysis of human CD4 cells latently infected with HIV-1. Nat Commun. 2015;6:8447.
Sloan DD, Lam CY, Irrinki A, Liu L, Tsai A, Pace CS, et al. Targeting HIV reservoir in infected CD4 T cells by dual-affinity re-targeting molecules (DARTs) that bind HIV envelope and recruit Cytotoxic T cells. PLoS Pathog. 2015;11(11):e1005233.
Sung JA, Pickeral J, Liu L, Stanfield-Oakley SA, Lam CY, Garrido C, et al. Dual-affinity re-targeting proteins direct T cell-mediated cytolysis of latently HIV-infected cells. J Clin Invest. 2015;125(11):4077–90.
Leibman RS, Riley JL. Engineering T cells to functionally cure HIV-1 infection. Mol Ther. 2015;23(7):1149–59.
Yang OO, Tran AC, Kalams SA, Johnson RP, Roberts MR, Walker BD. Lysis of HIV-1-infected cells and inhibition of viral replication by universal receptor T cells. Proc Natl Acad Sci U S A. 1997;94(21):11478–83.
Ali A, Kitchen SG, Chen IS, Ng HL, Zack JA, Yang OO. HIV-1-specific Chimeric antigen receptors based on broadly neutralizing antibodies. J Virol. 2016;90(15):6999–7006.
Bai L, Smith DC, Wang S. Small-molecule SMAC mimetics as new cancer therapeutics. Pharmacol Ther. 2014;144(1):82–95.
Campell GR, Bruckman RS, Chu YL, Spector SA. Autophagy induction by Histone Deacetylase inhibitors inhibits HIV-1 infection in macrophages. Boston: CROI 2016; 2016.
Pache L, Dutra MS, Spivak AM, Marlett JM, Murry JP, Hwang Y, et al. BIRC2/cIAP1 is a negative regulator of HIV-1 transcription and can be targeted by Smac Mimetics to promote reversal of viral latency. Cell Host Microbe. 2015;18(3):345–53.
Velu V, Shetty RD, Larsson M, Shankar EM. Role of PD-1 co-inhibitory pathway in HIV infection and potential therapeutic options. Retrovirology. 2015;12:14.
Akhmetzyanova I, Drabczyk M, Neff CP, Gibbert K, Dietze KK, Werner T, et al. PD-L1 expression on retrovirus-infected cells mediates immune escape from CD8+ T cell killing. PLoS Pathog. 2015;11(10):e1005224.
Hoffmann M, Pantazis N, Martin GE, Hickling S, Hurst J, Meyerowitz J, et al. Exhaustion of activated CD8 T cells predicts disease progression in primary HIV-1 infection. PLoS Pathog. 2016;12(7):e1005661.
Davar D, Wilson M, Pruckner C, Kirkwood JM. PD-1 blockade in advanced melanoma in patients with hepatitis C and/or HIV. Case Rep Oncol Med. 2015;2015:737389.
Gay CL, Bosch RJ, Ritz J, Hataye JM, Aga E, Tressler RL, et al. Clinical trial of the anti-PD-L1 antibody BMS-936559 in HIV-1 infected participants on suppressive antiretroviral therapy. J Infect Dis. 2017. doi:10.1093/infdis/jix191. Epub ahead of print.
Egan MA. Current prospects for the development of a therapeutic vaccine for the treatment of HIV type 1 infection. AIDS Res Hum Retrovir. 2004;20(8):794–806.
Mylvaganam GH, Silvestri G, Amara RR. HIV therapeutic vaccines: moving towards a functional cure. Curr Opin Immunol. 2015;35:1–8.
Leth S, Schleimann MH, Nissen SK, Hojen JF, Olesen R, Graversen ME, et al. Combined effect of Vacc-4x, recombinant human granulocyte macrophage colony-stimulating factor vaccination, and romidepsin on the HIV-1 reservoir (REDUC): a single-arm, phase 1B/2A trial. Lancet HIV. 2016;3(10):e463–72.
Mothe B, Manzardo C, Coll P, Sanchez-Bernabeu A, Escrig R, Perez-Alvarez N, et al., editors. Safety and immunogenicity of ChAd.HIVconsv and MVA.HIVconsv therapeutic vaccines in a cohort of early treated HIV-1 infected individuals2015. Vancouver, BC: Towards and HIV cure symposium. 2015. Abstract PE45.
Mothe B, Molto J, Manzardo C, Coll J, Puertas MC, Martinez-Picado J, et al. Editors. Viral control induced by HIVconsv vaccines and romidepsin in early treated individuals. Seattle, WA: Conference on Retroviruses and Opportunistic Infections (CROI). 2017. Abstract 119LB Session O-11.
Acknowledgements
DWC recieves a salary award from the Department of Medicine, University of Ottawa at The Ottawa Hospital.
Funding
No funding was received for this study.
Availability of data and materials
Not applicable
Author information
Authors and Affiliations
Contributions
KT and MSH conceived the conceptual framework for this study. MSH wrote the first manuscript outline. KT wrote the first manuscript draft and led all revisions of the manuscript. BTF, RL, and DWC all contributed significantly to the content and writing of this manuscript. All authors have read the last version of the manuscript and have consented to submit for publication. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Thorlund, K., Horwitz, M.S., Fife, B.T. et al. Landscape review of current HIV ‘kick and kill’ cure research - some kicking, not enough killing. BMC Infect Dis 17, 595 (2017). https://doi.org/10.1186/s12879-017-2683-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-017-2683-3