Abstract
Background
Salmonella enterica serovar Dublin is a zoonotic infection that can be transmitted from cattle to humans through consumption of contaminated milk and milk products. Outbreaks of human infections by S. Dublin have been reported in several countries including high-income countries. A high proportion of S. Dublin cases in humans are associated with invasive disease and systemic illness. The genetic basis of virulence in S. Dublin is not well characterized.
Methods
Whole genome sequencing was applied to a set of clinical invasive and non-invasive S. Dublin isolates from different countries in order to characterize the putative genetic determinants involved in the virulence and invasiveness of S. Dublin in humans.
Results
We identified several virulence factors that form the bacterial invasome and may contribute to increasing bacterial virulence and pathogenicity including mainly Gifsy-2 prophage, two different type 6 secretion systems (T6SSs) harbored by Salmonella pathogenicity islands; SPI-6 and SPI-19 respectively and virulence genes; ggt and PagN. Although Vi antigen and the virulence plasmid have been reported previously to contribute to the virulence of S. Dublin we did not detect them in all invasive isolates indicating that they are not the main virulence determinants in S. Dublin.
Conclusion
Several virulence factors within the genome of S. Dublin might contribute to the ability of S. Dublin to invade humans’ blood but there were no genomic markers that differentiate invasive from non-invasive isolates suggesting that host immune response play a crucial role in the clinical outcome of S. Dublin infection.
Similar content being viewed by others
Background
Salmonellosis is one of the most common foodborne diseases worldwide. Salmonella enterica (S. enterica) causes a huge global burden of morbidity and mortality in humans. It is estimated that Salmonella serovars responsible for typhoid fever kill over 250,000 humans each year [1] while non-typhoidal Salmonella (NTS) serovars that are responsible for diarrhoeal illness cause 155,000 deaths annually [2]. Moreover, NTS might have adapted to cause invasive disease and systemic infections in humans; children, the elderly and immunocompromised and it is estimated that 680,000 people die every year as a result of infection by invasive NTS (iNTS) [3].
The most predominant iNTS serovars associated with systemic illness in humans are S. Typhimurium, S. Choleraesuis and S. Dublin [4, 5]. S. Dublin is specifically adapted to cattle [6] thus, people can be infected through contact with infected animals or consumption of contaminated food including raw milk and raw-milk cheese. Outbreaks of human S. Dublin infection have been reported in some European countries including Ireland and France [7, 8].
Several virulence factors have been identified within the human adapted serovars Typhi and Paratyphi [9, 10]. On the other hand, little is known about the molecular basis of virulence in iNTS more specifically S. Dublin. Our understanding of the genetic basis of invasiveness in S. Dublin is skewed by the fact that most studies have focused on the most common iNTS; S. Typhimurium in particular the highly invasive multidrug-resistant (MDR) S. Typhimurium of a distinct Multilocus Sequence Type (MLST), ST313 that has been associated with severe infections and deaths in humans in sub-Saharan Africa [11, 12].
The aim of this study is to characterise the invasome of S. Dublin and the virulence factors that might enable the bacteria to invade blood causing systemic illness. We therefore applied whole genome sequencing (WGS) to a set of S. Dublin isolates from different countries all over the world.
Methods
Bacterial strains and whole genome sequencing
A set of S. Dublin isolates from different countries (Table 1) submitted to Centre National de Référence des Salmonella, Institut Pasteur were selected for WGS. The set of isolates included 22 human invasive isolates; 19 isolates from blood and 2 isolates from urine in addition to one isolate from pus. For comparison, we included 6 clinical non-invasive isolates from stool and 7 veterinary isolates. We also included the original S. Dublin isolate isolated from the stool of a patient in Dublin, Ireland (WS247) in 1929 giving the name of Dublin serovar. Furthermore, the reference S. Dublin isolate; SARB13 isolated in France from cattle in 1982 [13] was also included in this study.
WGS was carried out by the Center for Genomic Epidemiology at the Technical University of Denmark where genomic DNA was prepared for Illumina pair-end (PE) sequencing using the Illumina (Illumina, Inc., San Diego, CA) NexteraXT® Guide 150,319,425,031,942 following the protocol revision C (http://support.illumina.com/downloads/nextera_xt_sample_preparation_guide_15031942.html). A sample of the pooled NexteraXT Libraries was loaded onto an Illumina MiSeq reagent cartridge using MiSeq Reagent Kit v2 and 500 cycles with a Standard Flow Cell. The libraries were sequenced using an Illumina platform and MiSeq Control Software 2.3.0.3. All isolates were pair-end sequenced using 100 bp PE libraries. Raw sequence data have been submitted to the European Nucleotide Archive (http://www.ebi.ac.uk/ena) under study accession no.: PRJEB17616 (http://www.ebi.ac.uk/ena/data/view/PRJEB17616).
Bioinformatic analysis
The quality of the raw sequence data was evaluated using FastQC toolkit (http://www.bioinformatics.babraham.ac.uk/projects/fastqc/). Low quality reads were removed using ea.-utils package (https://expressionanalysis.github.io/ea-utils/). PE reads were assembled using Velvet [13] and the best possible assembly with the highest N50 value was annotated using RAST server [14]. The assembled sequences were analyzed to detect the sequence type (ST) of S. enterica, plasmid replicons and acquired antimicrobial resistance genes (ARGs) using MLST, PlasmidFinder and ResFinder respectively available from Center for Genomic Epidemiology (CGE) https://cge.cbs.dtu.dk//services/all.php. Ribosomal MLST (rMLST) was determined using Enterobase https://enterobase.warwick.ac.uk/
PE reads from each isolate were mapped against the reference genome of S. Dublin strain CT_02021853 (accession number: NC_011205.1) using Burrows Wheeler Aligner (BWA) [15]. Single nucleotide polymorphisms (SNPs) were identified using samtools mpileup [16]. The best-fit model for nucleotides substitution was determined by jModelTest [17] then a maximum likelihood (ML) phylogeny based on SNPs was constructed by MEGA6 software [18] using 1000 bootstrap replicates.
BLASTn [19] was used for the alignment of virulence genes and genomic regions. Blast Ring Image Generator (BRIG) was used to illustrate the presence/absence of the virulence determinants [20].
Results
Putative virulence regions and genes in S. Dublin
Vi-coding genes harboured by Salmonella Pathogenicity Island (SPI); SPI-7 were absent from all S. Dublin isolates except three isolates including the reference cattle isolate; SARB13 and two clinical isolates; 04.4663 from blood and 201,208,251 from pus (Fig. 1).
Complete genome alignment of S. Dublin isolates from France. The viaB operon is present in the reference S. Typhi str. CT18 (accession number: AL513382) but absent from all S. Dublin isolates sequenced in this study except three isolates including an isolate from human blood (04.4663), an isolate from human pus (201208251) and the reference SARB13 isolate from cattle
Interestingly, genes coding for flagellum biosynthesis were identical among invasive and non-invasive isolates.
All S. Dublin isolates except these three isolates; SARB13, 04.4663 and 201,208,251 harbour the putative virulence gene st313-td on the degraded pathogenicity island ST313-GI (Fig. 2) which is entirely absent from the Vi positive three isolates (SARB13, 04.4663 and 201,208,251).
Complete genome alignment of S. Dublin isolates from France. The novel genomic island ST313-GI harbouring the gene st313-td is present in the invasive S. Typhimurium str. D23580 (accession number: FN4244051) however they are absent from the three Vi antigen positive S. Dublin isolates (04.4663, 201,208,251 and SARB13). The other S. Dublin isolates harbour the putative virulence gene st313-td despite that the genomic island ST313-GI is degraded
On the other hand, all S. Dublin isolates sequenced in this study harbour pathogenicity islands SPI-6 and SPI-19 that encode type VI secretion system (T6SS); T6SSSPI-6 and T6SSSPI-19 respectively and they are all lysogenic for Gifsy-2 prophage (Fig. 3) that harbor the gene encoding Gifsy-2 prophage attachment and invasion protein.
Complete genome alignment of S. Dublin isolates from France. S. Dublin str. CT_02021853 (accession number: NC_011205.1) is used as a reference. Gifsy-2 like prophage (accession number: NC_010393) and the two different T6SSs present in reference S. Dublin str. CT_02021853 including T6SSSPI-6 (Locus_tag: SeD_A0289 - SeD_A0326) and T6SSSPI-19 (Locus_tag: SeD_A1212 - SeD_A1243) are present in all clinical and veterinary isolates from France. The virulence plasmid pCT02021853_74 (accession number: NC_011204.1) was detected in all S. Dublin isolates expect three clinical isolates including 93.1557 from stool and 93.3170 and 201,005,507 from blood
An accessory genome that is identical to the virulence plasmid pCT02021853_74 (accession number: NC_011204.1) that harbor the virulence spv locus was detected in all S. Dublin isolates (plasmid replicons; incX1 and incFII) expect three clinical isolates; including 93.1557 from stool and 93.3170 and 201,005,507 from blood that harbour no plasmids altogether. On the other hand, the cattle isolate 93.1086 has a similar but smaller plasmid than the virulence plasmid pCT02021853_74 that lacks the virulence spv locus as a result of internal deletion.
Interestingly, the clinical invasive isolates; 93.5462 from Mali and 05.2324 from Peru harbour another plasmid; plasmid ST4/74 of S. Typhimurium (accession number: CP002490) and plasmid pSBLT of S. Typhimurium (accession number: LN794247) respectively in addition to the virulence plasmid pCT02021853_74 of S. Dublin.
All S. Dublin isolates including clinical and veterinary isolates harbor putative virulence factors including ggt and PagN genes that encode for γ-glutamyl transpeptidase (GGT) and an outer membrane protein respectively. The distribution of the putative virulence factors among all S. Dublin isolates are provided in Additional file 1: Table S1.
Antimicrobial resistance genes present in S. Dublin isolates
No acquired ARGs were detected in S. Dublin isolates except in two clinical invasive isolates from blood including isolate 93.5462 isolated in 1993 from Mali that harbours ARGs to aminoglycoside (strA, strB, and aadA1), phenicol (catA1) and sulphonamide (sul1 and sul2) on the plasmid ST4/74 of S. Typhimurium and isolate 05.2324 isolated from Peru in 2005 that has ARGs to aminoglycoside (strA, strB, and aadA1 and aac(3)-IIa), beta-lactam (blaTEM-1B), sulfonamide (sul1 and sul2) and trimethoprim (dfrA1) on the plasmid pSBLT of S. Typhimurium.
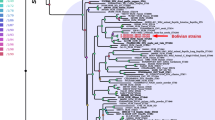
Phylogenetic relationship among S. Dublin isolates
The phylogenetic SNP analysis showed that invasive and gastroenteritis isolates were intermixed as SNPs were randomly distributed around the chromosome of S. Dublin.
All isolates except three isolates; SARB13 from cattle, 201,208,251 from human pus and 04.4663 from human blood, were very closely related (Fig. 4), showed higher divergence from the other isolates and they have a distinct MLST (ST-73) and a distinct rMLST while other S. Dublin isolates have ST-10 except one isolate; 99.5828 that have ST-2037 but they all have the same rMLST; 53 (Table 1).
Maximum-likelihood phylogenetic tree of S. Dublin strains from different countries; invasive clinical isolates are highlighted in grey, gastroenteritis human isolates are highlighted in green and veterinary isolates are highlighted in yellow. The tree is based on SNPs determined from the whole genome sequence. Tree was inferred by using a general time-reversible (GTR) model. Bootstrap support values, given as a percentage of 1000 replicates, are shown above the branches
Discussion
Human infection with iNTS represents a significant public health problem. A high proportion of S. Dublin cases in humans are characterized by bloodstream infection. Furthermore, the antibiotic resistance is increasing in S. Dublin as we detected two clinical isolates from blood that are resistant to multiple antibiotics.
The invasiveness of S. Dublin may be related to the expression of the Vi (virulence) antigen which is a capsular polysaccharide antigen commonly found in the human adapted S. Typhi and S. Paratyphi C. It has however also been detected in S. Dublin [21].
The Vi proteins are encoded within the viaB (Vi capsule biosynthesis) locus on SPI-7 [22, 23]. The viaB locus contains both Vi antigen biosynthetic genes (tviB, tviC, tviD and tviE) and export genes (vexA, vexB, vexC, vexD and vexE). The expression of Vi antigen is controlled by the rcsB-rcsC and ompR-envZ two-component regulator systems which lie outside the SPI-7 they however, interact with tviA; the first gene of the viaB gene cluster and regions upstream of the tviA promoter [24].
Experimental studies showed that Vi antigen is antiopsonic and antiphagocytic as it reduces the level of S. Typhi-induced tumor necrosis factor alpha (TNFα) by human macrophages and it also increases the resistance of S. Typhi to oxidative stress [25, 26].
In this study, we screened all S. Dublin isolates from France for the viaB operon and we found that Vi-coding genes were absent from all isolates except three isolates including the reference veterinary isolate; SARB13 and two clinical isolates; 04.4663 from blood and 201,208,251 from pus. We therefore conclude that it is unlikely that Vi antigen is the main virulence determinant for S. Dublin since it is absent from other invasive isolates from blood and urine.
Although Vi capsular polysaccharide antigen was not present in all invasive isolates it is possible that S. Dublin produces a unique O-antigen capsule that plays a role in increasing bacterial virulence and pathogenicity. Further in vitro and in vivo studies using O-antigen capsule deficient mutant are required to confirm this hypothesis.
Flagellum is considered as a virulence factor for motile bacteria such as Salmonella [27]. The surface domains of the flagellin protein are highly immunogenic and play an important role in triggering host innate and adaptive immune responses therefore, motile bacteria have evolved several mechanisms to overcome flagellin recognition by host receptors [28] however we detected no diversity among invasive an non-invasive S. Dublin strains in flagellar biosynthesis genes including fliC gene coding for flagellin, fliD coding for the flagellum capping protein and fliA coding for flagellum-specific sigma factor.
Although the three S. Dublin isolates; 04.4663, 201,208,251 and SARB13 are positive for the Vi antigen they lack the novel pathogenicity island ST313-GI that harbours the putative virulence gene st313-td. On the other hand, all other S. Dublin isolates harbour the st313-td gene on a degraded ST313-GI.
Although the exact role of st313-td in increasing bacterial virulence is not known experimental studies showed that st313-td is associated with the virulence and systemic infection in invasive S. Typhimurium of a distinct MLST, ST313, that has emerged recently in Africa [12]. It has been shown that virulence of S. Typhimurium in the mouse model was reduced in the absence of st313-td therefore, it is hypothesised that st313-td might help in bacterial evasion from host’s immune system through decreasing the binding of the bacteria to specific antibodies causing less uptake by macrophages or through decreasing the susceptibility to complement mediated lysis [11, 28].
We hypothesise that it is likely that st313-td plays a role in the virulence of S. Dublin hence, we detected it in all isolates (except the three isolates that are positive for Vi antigen; 04.4663, 201,208,251 and SARB13) however further experimental work is required to test its role in the virulence of S. Dublin.
There are other mobile genetic elements (MGEs) (excluding SPI-7 harbouring Vi antigen and genomic island ST313-GI encoding the putative virulence gene st313-td) that might also contribute to the virulence of S. Dublin in humans including SPI-6 and SPI-19 which harbour two different types of T6SS including T6SSSPI-6 and T6SSSPI-19 respectively.
It has been shown that T6SSs play a significant role in bacterial pathogenesis as they function as contractile nanomachines to puncture human cells and deliver virulence and lethal factors [29]. Experimental studies showed that T6SSSPI-6 plays a crucial role in the invasiveness and the systemic spread of S. Typhimurium [30] while T6SSSPI-19 has been reported to contribute to the survival of the poultry adapted serovar S. Gallinarum within infected macrophages [31].
All S. Dublin isolates harbour SPI-6 and SPI-19 that encode T6SSSPI-6 and T6SSSPI-19 respectively. Interestingly, SPI-6 and SPI-19 harbouring the two different T6SS have been also detected in clinical human isolates from Ireland including invasive and gastroenteritis isolates [32] suggesting that they contribute to the ability of S. Dublin to cause invasive disease in humans.
Another MGE that might contribute to the virulence and pathogenesis of Salmonella serovars including S. Dublin is the lambdoid prophage Gifsy-2 [33] as it encodes several virulence genes including sodCI, sseI and gtgE [34].
In this study, we found that all S. Dublin isolates are lysogenic for Gifsy-2 prophage and they all harbor the gene encoding Gifsy-2 prophage attachment and invasion protein suggesting that Gifsy-2 might be associated with the predisposition of S. Dublin to cause systemic illness in humans.
Plasmids are other MGEs that have been shown to play a significant role in the acquisition of virulence and antimicrobial resistance genes in several Salmonella serovars [35]. Experimental studies showed that S. Dublin plasmid encoding the virulence spv locus is involved in the dissemination and spread of bacteria to the blood [36, 37].
Interestingly, all S. Dublin isolates sequenced in this study except three clinical isolates including 93.3170 and 201,005,507 from blood and 93.1557 from stool harbour the virulence S. Dublin plasmid pCT02021853 that encodes the spv genes. Although the cattle isolate (93.1086) harbours a closely related plasmid to the virulence plasmid pCT02021853 the plasmid does not harbour the virulence spv locus. We therefore conclude that it is unlikely that the virulence plasmid is the main virulence determinant for S. Dublin and it is not critical for bacterial invasiveness since it is absent from two invasive clinical isolates from blood; 93.3170 and 05.1078.
Among the virulence factors that might contribute to the virulence of S. Dublin is γ-glutamyl transpeptidase (GGT) as it has been reported to contribute to the virulence of Helicobacter pylori [38] furthermore, it plays a significant role in inhibiting T-cell proliferation [39]. We found that the gene ggt is harboured by all S. Dublin isolates including human and animal isolates.
Another virulence gene, PagN, encodes for an outer membrane protein (PagN) that has been reported to contribute to the virulence of S. Typhimurium through mediating bacterial adhesion and invasion of mammalian cells [40, 41]. Experimental studies showed that PagN is a strong immuogen in mice and it can therefore be a potential vaccine candidate for salmonellosis [42]. Interestingly, we found that PagN is harboured by all S. Dublin isolates including invasive and non-invasive isolates suggesting its relation to bacterial virulence and invasiveness.
Although S. Dublin is adapted to cattle as a result of extensive genome decay and pseudogenes accumulation [6] S. Dublin can infect other animals [43, 44]. The phylogenetic SNP analysis showed the close relation among the veterinary isolates and human isolates as SNPs were randomly distributed around the chromosome of S. Dublin. All S. Dublin isolates were intermixed and there were no genomic differences among clinical invasive and non-invasive isolates.
Conclusions
We identified several virulence factors in S. Dublin isolates that form the bacterial invasome however, we could not detect any genomic markers that differentiate invasive from non-invasive disease suggesting that host factors and immune response play a significant role in the disease outcome.
Abbreviations
- ARG:
-
Antimicrobial resistance gene
- iNTS:
-
Invasive nontyphoidal Salmonella
- MGE:
-
Mobile genetic element
- NTS:
-
Nontyphoidal Salmonella
- S. Dublin:
-
Salmonella Dublin
- S. Typhimurium:
-
Salmonella Typhimurium
- SPI:
-
Salmonella pathogenicity islands
- T6SS:
-
Type VI secretion system
References
Crump JA, Mintz ED. Global trends in typhoid and paratyphoid fever. Clin Infect Dis. 2010;50(2):241–6.
Majowicz SE, Musto J, Scallan E, Angulo FJ, Kirk M, O'Brien SJ, Jones TF, Fazil A, Hoekstra RM. The global burden of nontyphoidal salmonella gastroenteritis. Clin Infect Dis. 2010;50(6):882–9.
Ao TT, Feasey NA, Gordon MA, Keddy KH, Angulo FJ, Crump JA. Global burden of invasive nontyphoidal Salmonella disease, 2010(1). Emerg Infect Dis. 2015;21(6)
Gordon MA. Invasive nontyphoidal salmonella disease: epidemiology, pathogenesis and diagnosis. Curr Opin Infect Dis. 2011;24(5):484–9.
Okoro CK, Kingsley RA, Connor TR, Harris SR, Parry CM, Al-Mashhadani MN, Kariuki S, Msefula CL, Gordon MA, de Pinna E, et al. Intracontinental spread of human invasive salmonella typhimurium pathovariants in sub-Saharan Africa. Nat Genet. 2012;44(11):1215–21.
Langridge GC, Fookes M, Connor TR, Feltwell T, Feasey N, Parsons BN, Seth-Smith HM, Barquist L, Stedman A, Humphrey T, et al. Patterns of genome evolution that have accompanied host adaptation in salmonella. Proc Natl Acad Sci U S A. 2015;112(3):863–868.
Vaillant V, Haeghebaert S, Desenclos JC, Bouvet P, Grimont F, Grimont PA, Burnens AP. Outbreak of salmonella dublin infection in France, November - December 1995. Euro Surveill. 1996;1(2):9–10.
Mohammed M, Delappe N, O'Connor J, Mc KP, Garvey P, Cormican M. Whole genome sequencing provides an unambiguous link between salmonella Dublin outbreak strain and a historical isolate. Epidemiol Infect. 2015:1–6.
Schadich E, Dzubak P, Hajduch M. Role of salmonella Typhi vi antigen and secretory systems on immune response. Curr Pharm Des. 2016;22(41):6251–6260.
Kaur J, Jain SK. Role of antigens and virulence factors of salmonella enterica serovar Typhi in its pathogenesis. Microbiol Res. 2012;167(4):199–210.
Herrero-Fresno A, Wallrodt I, Leekitcharoenphon P, Olsen JE, Aarestrup FM, Hendriksen RS. The role of the st313-td gene in virulence of salmonella typhimurium ST313. PLoS One. 2014;9(1):e84566.
Kingsley RA, Msefula CL, Thomson NR, Kariuki S, Holt KE, Gordon MA, Harris D, Clarke L, Whitehead S, Sangal V, et al. Epidemic multiple drug resistant salmonella typhimurium causing invasive disease in sub-Saharan Africa have a distinct genotype. Genome Res. 2009;19(12):2279–87.
Zerbino DR, Birney E. Velvet: algorithms for de novo short read assembly using de Bruijn graphs. Genome Res. 2008;18(5):821–9.
Aziz RK, Bartels D, Best AA, DeJongh M, Disz T, Edwards RA, Formsma K, Gerdes S, Glass EM, Kubal M, et al. The RAST server: rapid annotations using subsystems technology. BMC Genomics. 2008;9:75.
Li H, Durbin R. Fast and accurate short read alignment with burrows-wheeler transform. Bioinformatics. 2009;25(14):1754–60.
Li H, Handsaker B, Wysoker A, Fennell T, Ruan J, Homer N, Marth G, Abecasis G, Durbin R. The sequence alignment/map format and SAMtools. Bioinformatics. 2009;25(16):2078–9.
Posada D. jModelTest: phylogenetic model averaging. Mol Biol Evol. 2008;25(7):1253–6.
Tamura K, Stecher G, Peterson D, Filipski A, Kumar S. MEGA6: molecular evolutionary genetics analysis version 6.0. Mol Biol Evol. 2013;30(12):2725–9.
Camacho C, Coulouris G, Avagyan V, Ma N, Papadopoulos J, Bealer K, Madden TL. BLAST+: architecture and applications. BMC bioinformatics. 2009;10:421.
Alikhan NF, Petty NK, Ben Zakour NL, Beatson SA. BLAST ring image generator (BRIG): simple prokaryote genome comparisons. BMC Genomics. 2011;12:402.
Morris C, Tam CK, Wallis TS, Jones PW, Hackett J. Salmonella enterica serovar Dublin strains which are vi antigen-positive use type IVB pili for bacterial self-association and human intestinal cell entry. Microb Pathog. 2003;35(6):279–84.
Hashimoto Y, Ezaki T, Li N, Yamamoto H. Molecular cloning of the ViaB region of salmonella typhi. FEMS Microbiol Lett. 1991;69(1):53–6.
Pickard D, Wain J, Baker S, Line A, Chohan S, Fookes M, Barron A, Gaora PO, Chabalgoity JA, Thanky N, et al. Composition, acquisition, and distribution of the vi exopolysaccharide-encoding salmonella enterica pathogenicity island SPI-7. J Bacteriol. 2003;185(17):5055–65.
Parkhill J, Dougan G, James KD, Thomson NR, Pickard D, Wain J, Churcher C, Mungall KL, Bentley SD, Holden MT, et al. Complete genome sequence of a multiple drug resistant salmonella enterica serovar Typhi CT18. Nature. 2001;413(6858):848–52.
Hirose K, Ezaki T, Miyake M, Li T, Khan AQ, Kawamura Y, Yokoyama H, Takami T. Survival of vi-capsulated and vi-Deleted salmonella typhi strains in cultured macrophage expressing different levels of CD14 antigen. FEMS Microbiol Lett. 1997;147(2):259–65.
Looney RJ, Steigbigel RT. Role of the vi antigen of salmonella typhi in resistance to host defense in vitro. J Lab Clin Med. 1986;108(5):506–16.
Logan SM. Flagellar glycosylation - a new component of the motility repertoire? Microbiology. 2006;152(Pt 5):1249–62.
De Maayer P, Cowan DA. Flashy flagella: flagellin modification is relatively common and highly versatile among the Enterobacteriaceae. BMC Genomics. 2016;17:377.
Kapitein N, Mogk A. Deadly syringes: type VI secretion system activities in pathogenicity and interbacterial competition. Curr Opin Microbiol. 2013;16(1):52–8.
Pezoa D, Yang HJ, Blondel CJ, Santiviago CA, Andrews-Polymenis HL, Contreras I. The type VI secretion system encoded in SPI-6 plays a role in gastrointestinal colonization and systemic spread of salmonella enterica serovar typhimurium in the chicken. PLoS One. 2013;8(5):e63917.
Blondel CJ, Jimenez JC, Leiva LE, Alvarez SA, Pinto BI, Contreras F, Pezoa D, Santiviago CA, Contreras I. The type VI secretion system encoded in salmonella pathogenicity island 19 is required for salmonella enterica serotype Gallinarum survival within infected macrophages. Infect Immun. 2013;81(4):1207–20.
Mohammed M, Cormican M. Whole genome sequencing provides insights into the genetic determinants of invasiveness in salmonella Dublin. Epidemiol Infect. 2016;144(11):2430–9.
Figueroa-Bossi N, Bossi L. Inducible prophages contribute to salmonella virulence in mice. Mol Microbiol. 1999;33(1):167–76.
Ho TD, Figueroa-Bossi N, Wang M, Uzzau S, Bossi L, Slauch JM. Identification of GtgE, a novel virulence factor encoded on the Gifsy-2 bacteriophage of salmonella enterica serovar typhimurium. J Bacteriol. 2002;184(19):5234–9.
Moreno Switt AI, den Bakker HC, Cummings CA, Rodriguez-Rivera LD, Govoni G, Raneiri ML, Degoricija L, Brown S, Hoelzer K, Peters JE, et al. Identification and characterization of novel Salmonella Mobile elements involved in the dissemination of genes linked to virulence and transmission. PLoS One. 2012;7(7):e41247.
Wallis TS, Paulin SM, Plested JS, Watson PR, Jones PW. The salmonella dublin virulence plasmid mediates systemic but not enteric phases of salmonellosis in cattle. Infect Immun. 1995;63(7):2755–61.
Valone SE, Chikami GK, Miller VL. Stress induction of the virulence proteins (SpvA, −B, and -C) from native plasmid pSDL2 of salmonella dublin. Infect Immun. 1993;61(2):705–13.
Gong M, Ling SS, Lui SY, Yeoh KG, Ho B. Helicobacter pylori gamma-glutamyl transpeptidase is a pathogenic factor in the development of peptic ulcer disease. Gastroenterology. 2010;139(2):564–73.
Schmees C, Prinz C, Treptau T, Rad R, Hengst L, Voland P, Bauer S, Brenner L, Schmid RM, Gerhard M. Inhibition of T-cell proliferation by helicobacter pylori gamma-glutamyl transpeptidase. Gastroenterology. 2007;132(5):1820–33.
Lambert MA, Smith SG. The PagN protein of salmonella enterica serovar typhimurium is an adhesin and invasin. BMC Microbiol. 2008;8:142.
Lambert MA, Smith SG. The PagN protein mediates invasion via interaction with proteoglycan. FEMS Microbiol Lett. 2009;297(2):209–16.
Yang Y, Wan C, Xu H, Aguilar ZP, Tan Q, Xu F, Lai W, Xiong Y, Wei H. Identification of an outer membrane protein of salmonella enterica serovar typhimurium as a potential vaccine candidate for salmonellosis in mice. Microbes Infect/Institut Pasteur. 2013;15(5):388–98.
Burns AM, Lawlor PG, Gardiner GE, McCabe EM, Walsh D, Mohammed M, Grant J, Duffy G. Salmonella occurrence and Enterobacteriaceae counts in pig feed ingredients and compound feed from feed mills in Ireland. Prev Vet Med. 2015;121(3–4):231–9.
Liebana E, Garcia-Migura L, Clouting C, Cassar CA, Clifton-Hadley FA, Lindsay EA, Threlfall EJ, Chappell SA, Davies RH. Investigation of the genetic diversity among isolates of salmonella enterica serovar Dublin from animals and humans from England, Wales and Ireland. J Appl Microbiol. 2002;93(5):732–44.
Acknowledgments
N/A.
Funding
The sequencing was supported by the Center for Genomic Epidemiology at the Technical University of Denmark funded by grant 09–067103/DSF from the Danish Council for Strategic Research.
Availability of data and materials
Raw sequence data of isolates are available via European Nucleotide Archive (http://www.ebi.ac.uk/ena) under study accession no.: PRJEB17616 (http://www.ebi.ac.uk/ena/data/view/PRJEB17616).
Author information
Authors and Affiliations
Contributions
MM: conceived and designed the study, carried out data analyses and interpretation, conducted literature search and review, and wrote the first draft. SH, PL and RH: contributed to data interpretation, and critically revised the intellectual content of the paper. SH: isolated bacterial strains and carried out bacterial identification and serotyping. PL and RH: carried out libraries preparation and performed the whole genome sequencing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interest.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1: Table S1.
Distribution of putative virulence factors among S. Dublin isolates. (XLSX 13 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Mohammed, M., Le Hello, S., Leekitcharoenphon, P. et al. The invasome of Salmonella Dublin as revealed by whole genome sequencing. BMC Infect Dis 17, 544 (2017). https://doi.org/10.1186/s12879-017-2628-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-017-2628-x