Abstract
Background
Hip fractures are a common injury in older people. Many studies worldwide have identified various risk factors for hip fracture. However, risk factors for hip fracture have not been studied extensively in New Zealand. The interRAI home care assessment consists of 236 health questions and some of these may be related to hip fracture risk.
Methods
The cohort consisted of 45,046 home care clients aged 65 years and older, in New Zealand. Assessments ranged from September 2012 to October 2015. Hip fracture diagnosis was identified by linking ICD (International Classification of Diseases) codes from hospital admissions data (September 2012 to December 2015) to the interRAI home care data. Unadjusted and adjusted competing risk regressions, using the Fine and Gray method were used to identify risk factors for hip fracture. Mortality was the competing event.
Results
The cohort consisted of 61% female with a mean age of 82.7 years. A total of 3010 (6.7%) of the cohort sustained a hip fracture after assessment. After adjusting for sociodemographic and potentially confounding variables falls (SHR (Subhazard Ratio) = 1.17, 95% CI (Confidence interval): 1.05–1.31), previous hip fracture (SHR = 4.16, 95% CI: 2.93–5.89), female gender (SHR = 1.38, 95% CI: 1.22–1.55), underweight (SHR = 1.67, 95% CI = 1.39–2.02), tobacco use (SHR = 1.56, 95% CI = 1.25–1.96), Parkinson’s disease (SHR = 1.45, 95% CI: 1.14–1.84), and Wandering (SHR = 1.36, 95% CI: 1.07–1.72) were identified as risk factors for hip fracture. Shortness of breath (SHR = 0.80, 95% CI: 0.71–0.90), was identified as being protective against hip fracture risk. Males and females had different significant risk factors.
Conclusions
Risk factors for hip fracture similar to international work on risk factors for hip fracture, can be identified using the New Zealand version of the interRAI home care assessment.
Similar content being viewed by others
Background
Hip fractures cause significant disability for many older adults, with some of the worst outcomes for those aged 65 years or older [1]. Having a hip fracture in later life can lead to long recovery periods, a decreased quality of life, higher mortality rates and increased likelihood of entry into aged residential care (ARC) compared to those without a hip fracture [1,2,3].
Improving health outcomes using health data is a priority for the New Zealand government [4]. Since 2012, all community dwelling older New Zealanders requiring home health care services undergo a standardised assessment using the interRAI home care (interRAI-HC) assessment. At that time, New Zealand became one of the first countries in the world to mandate a standardised comprehensive medical and functional assessment for all older people who are seeking home care services. The interRAI-HC assessment is a comprehensive clinical assessment with questions on 20 health and social domains including disease diagnoses, cognitive function and social relationships. The interRAI-HC assessment is used to assess the health needs of frail older people and people with complex needs, living within the community. Typical home health care services being sought include visiting nurses, access to falls prevention programmes, and meals. In 2013 there were approximately 607,032 adults aged 65+ years in New Zealand [5]. A large number of these people have undergone a home care assessment, and as the ageing population increases many more people will also require health services. Using health data to identify individuals at greatest risk for hip fracture may facilitate prevention and delay adverse outcomes.
There have been many studies conducted identifying hip fracture risk in older adults. These include a variety of different cohorts including those recently admitted to hospital, those living in ARC facilities, and those living within the community. Each cohort has different risk profiles as they are subject to different environments and have differing health needs [6,7,8,9]. Stolee et al. (2009) identified risk factors for hip fracture in community dwelling older people requiring home care [7]. Their work used the Minimum Dataset (MDS), a precursor to the interRAI homecare assessment, and was based on 40,279 Canadian participants. Risk factors identified by Stolee et al. for a home care population were older age, females, osteoporosis, falls, unsteady gait, tobacco use, malnutrition and cognitive impairment [7]. Other studies identifying hip fracture risk for older people in older cohorts found factors such as differing ethnic backgrounds, bone mineral density (BMD), previous hip fractures, reduced physical activity, body mass index (BMI), chronic health conditions, and medications to be significant [2, 8, 10,11,12,13,14,15,16].
Hip fractures are a worldwide issue and have been studied extensively, yet there has been very little research in New Zealand on hip fracture risk. There is one known paper addressing hip fracture incidence rates in Māori (New Zealand’s indigenous peoples) and non-Māori people [17]; and the study found that non-Māori were at a higher risk than Māori – but that the incidence rates were increasing over time for both ethnic groups. However, this paper was published in 1995, there has been significant population change, and changes in prevention and health service delivery since that time. It is likely the risk profile and possible risk factors have also changed. Another study explored whether urinary incontinence was an independent risk factor for falls and hip fractures in community dwelling older men and women with complex needs. After controlling for confounders, results showed that urinary incontinence was not an independent risk factor for hip fracture [18]. Two further studies, identified specific medications were associated with an increased risk of fracture among older New Zealanders [14, 19]. No recent studies have specifically sought to identify the suite of risk factors associated with hip fractures amongst older adults in New Zealand as a group, and for the important ethnic groups.
There are methodological limitations with many previous studies of hip fracture risk. Studies have used an array of different statistical techniques, predominantly regression models such as Poisson, multivariate logistic regression, or Cox proportional hazards models [7, 20, 21]. However, due to the non-negligible likelihood of death amongst older adults with complex needs, more recent studies have employed competing risk regression models as they provide a less biased estimate of risk factors. [22, 23]. For example, Berry et al. (2017) recently determined risk factors for hip fracture and created a hip fracture risk score based on nursing home residents derived from a competing risk regression analysis [10].
The primary objective of this study was to determine risk factors for hip fracture in older people living in the community in New Zealand and receive home care. A secondary objective was to identify whether there were differences in risk factors for hip fracture between males and females.
Methods
Study design
This study used a time-to-event analysis from a national cohort.
Participants
People aged 65+ years living in the community with an interRAI-HC assessment undertaken between 1 September 2012 and 31 October 2015, who consented to their data being used for planning and research purposes. Only the first assessment for all participants were used, any subsequent assessments were removed from analysis. Individuals with end-stage disease, six or fewer months to live, as noted in the interRAI-HC assessment were excluded. Within the interRAI-HC assessment there is a question on living arrangements at time of assessment and a small number of participants had indicated living in a long-term care facility at time of assessment. These people were excluded from analysis along with anyone admitted to an ARC facility within 30 days of their assessment as this study was looking only at those living in the community in non-residential care. Similar to the work carried out by Berry et al. [10], 22,291 participants were randomly omitted from this study, as forthcoming work will build a prediction model based on these results and validate it against those randomly excluded.
Instruments/variables
The interRAI-HC version 9.1 (© interRAI corporation, Washington, D. C., 1994–2009) assessment tool is a comprehensive geriatric assessment record consisting of 236 questions across 20 domains such as cognitive function, nutrition, disease diagnoses and psychosocial well-being [24, 25]. The home care assessment is used for all older people requiring publically funded long-term home care services or aged residential care admission. Patients are referred by health practitioners to have their needs assessed by a trained interRAI assessor. Assessors visit the person in their own home and use a variety of sources to complete each assessment, including observations, interviews with the individual and their family members, and medical records. Assessors undergo rigorous training and are reassessed annually to ensure each assessor meets interRAI standards. All data are entered into an electronic database, which are collected and maintained by New Zealand’s Technical Advisory Services (TAS). Participant consented data (approximately 93% of all assessments undertaken) are released by TAS with the approval of the Ministry of Health. The assessment is also used to aid in the planning of home support and health care [24]. All questions are recorded electronically and assessments are linked with the National Health Index (NHI) number. The NHI is a unique identifier given to anyone in New Zealand receiving health services. The NHI can be encrypted and linked with other health datasets such as mortality information and hospital admissions within New Zealand. Variables of interest were identified from the literature and recoded within the interRAI-HC data. Variables were obtained from several domains within the interRAI dataset such as: Demographics, Cognitive/Functional, Falls and Fractures, Neuropsychiatric, Pain, Nutrition, Co-morbidities. A full list of the variables of interest, used for analysis can be found in Additional file 1: Table S1. Previous studies have highlighted age, sex and ethnicity as known demographics relating to hip fracture risk. Ethnicity was classified as Māori, Pasifika, Asian, European and Other. Participants were given the option to choose up to three ethnic identities and priority coding was used during the data cleaning process to reduce this to a single ethnicity. Where participants indicated more than one ethnicity priority was given to Māori, then Pasifika, and then Asian ethnicities. Age, sex, and ethnicity were employed as potential confounders when creating the adjusted model.
Hip fracture data were obtained from the National Minimum Dataset (NMDS) [26], released from the Ministry of Health with encrypted NHI numbers for all interRAI-HC participants who consented. Hip fractures were identified using ICD-10-AM (International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Australian Modification) diagnostic codes S720, S721, S722, S723, S724, S728, and S729. The first instance of hip fracture after an individual’s assessment was used. All hip fractures occurred before or on the 31 October 2015.
Mortality data were obtained from the Mortality Collection (MORT) [27], and were released from the Ministry of Health with encrypted NHI numbers for all interRAI-HC participants who consented. All deaths occurred before or on the 31 October 2015.
Statistical analysis
Reporting of analyses conformed to STROBE STrengthening the Reporting of OBservational studies in Epidemiology and RECORD (REporting of Studies Conducted using Observational Routinely collected Data) guidelines [28] to ensure this study reports results accurately and clearly. Basic frequency distributions of each variable of interest were examined as a total of the population. Competing risk regression models, using the Fine and Grey method [29], were utilised where hip fracture was the failure event and death was the competing event. Crude models were individually conducted for variable of interest and then a fully adjusted model which included age, sex and ethnicity was undertaken. All variables in the unadjusted models were included in the adjusted model. Subhazard ratios (SHRs) and 95% confidence intervals (CIs) were reported for each variable of interest. The data was stratified by sex to assess risk profiles for both males and females and adjusted competing risk models were undertaken. IBM SPSS version 23 [30] was used for general analyses and data cleaning, and Stata SE version 14.1 [31] was used to run competing risk regressions, and α = 0.05 defined statistical significance.
Ethics
Permission for this study was approved by the Ministry of Health’s Health and Disability Ethics Committees (14/STH/140) and only includes anonymised data provided by individuals who consented to their information being used for planning and research purposes.
Results
Participants
After applying the exclusion criteria, the sample consisted of 45,046 participants. Figure 1 below, details the exclusion criteria. Note, 22,291 were randomly omitted for this study, as forthcoming work will build a prediction model based on these results and validate it against those randomly excluded.
Demographics
The mean age at assessment was 82.7 years (range: 65 to 106 years). Overall, there were 27,705 (61.5%) females and 17,339 (38.5%) males. Comparatively, according to the New Zealand 2013 census of those aged 65+ years in New Zealand there were 54.1% female and 45.9% males [5]. Within the cohort 88.2% of people identified as European these are similar to 2013 census information. However, Pasifika make up 3.2% (1430) and Asians make up 2.3% (1037) of the cohort compared to 2.3 and 4.7%, respectively, of New Zealanders aged 65+ years [5]. Approximately, 2% (918) of individuals had no medications prescribed to them, compared to 98% (44,125) individuals who stated they had some medications prescribed by a physician. Adherence to medications varied with 83.7% of people stating they always adhered to the medications prescribed, 11.5% were adherent 80% of the time, and 2.7% were adherent less than 80% of the time, including failing to purchase prescribed medications. 47.5% (21,739) of individuals had a cognitive performance scale (CPS) of 2 or higher indicating they had some degree of cognitive impairment. A CPS from 2 to 6 indicates mild to very severe cognitive impairment [32].
Fractures and deaths
Of the test cohort 3010 (6.7%) sustained a hip fracture, 12,654 (28.1%) had died and 29,382 (65.2%) had not encountered either event by the end of the study period. Median follow-up time after the interRAI-HC assessment was 13.9 months (25th percentile 5.3 months, 75th percentile 23.8 months) from assessment, with a total person-time of 55,444 years.
Unadjusted and adjusted analyses
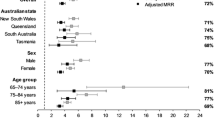
The SHR for females, in the adjusted model is 1.38 suggesting that females have a higher risk of hip fracture than males. The 85–94 year-old age group had the highest percentage of hip fractures (50.1% of all hip fractures) and there was a slight increase in hip fracture incidence rates with age. The SHR for each age group shows that as age increases the risk of sustaining a hip fracture increases (as shown in Table 1). The majority of the cohort are European ethnicity (88.2%) and most hip fractures were sustained by those of European ethnicity (94.1%). Table 1 below, outlines basic descriptive information for each of the demographic variables and shows the crude and adjusted SHRs.
Table 2 presents frequency distributions for each variable of interest, and unadjusted and adjusted SHR for each variable. Risk factors for hip fracture identified in the adjusted model from the variables listed in Additional file 1: Table S1 are sex, age, ethnicity, previous falls, previous hip fracture, wandering, low BMI, smoking tobacco, and Parkinson’s disease. Having shortness of breath, and, high BMI were related to a reduced risk of hip fracture. Having a previous hip fracture appeared to have the highest risk of sustaining a hip fracture with an adjusted SHR of 4.16.
Sex differences
Table 3 provides a comparison of the adjusted models between males and females. Significant risk factors for each group are marked in bold. There were differences in significant risk factors for males and females. The significant risk factors identified in the model for females were age, ethnicity, falls, previous hip fractures, wandering, BMI, tobacco use and shortness of breath. The significant factors identified for males were age, previous hip fracture, Parkinson’s disease and shortness of breath.
Discussion
Key findings
This study identified risk factors for hip fracture within a community dwelling cohort, and stratified by sex. To our knowledge this is the first study in New Zealand that has examined a large suite of risk factors associated with hip fractures amongst older adults in New Zealand. Risk factors identified in this study were age, female sex, ethnicity, falls, previous hip fracture, wandering, tobacco use, low BMI, shortness of breath and Parkinson’s disease.
Sex differences in risk were found between males and females. Significant risk factors for males were age, previous hip fracture, and Parkinson’s disease. Females had more significant risk factors than males including age, previous hip fracture, ethnicity, falls, wandering, BMI, tobacco use, and shortness of breath. For the female group a diagnosis of chronic obstructive pulmonary disease (COPD) was associated with a reduced risk of hip fracture.
Findings within the literature
Several of the findings within this study are consistent with previous research. For example, falls are consistently deemed a significant risk for hip fracture. Most hip fractures in older people occur from a fall [33]. Similarly, prior studies on hip fracture risk have found previous hip fractures to be a significant risk factor [21, 34, 35]. Within this study, previous hip fractures have been identified as having the largest risk of sustaining a hip fracture (SHR 4.16, p < 0.001). People who have had a previous hip fracture are around four times more likely to have a second hip fracture compared to individuals who have not had a prior fracture. This suggests emphasis should be placed on preventing a subsequent hip fracture in people who have already had a previous hip fracture. Additionally, those with a low BMI are more likely to have a hip fracture than those who have a normal BMI, and those overweight or obese had a lowered risk for hip fracture. These findings are consistent with the literature [11, 36,37,38]. Our study did not find gait speed to be a significant risk factor for hip fracture, however a recent study by Harvey et al. found greater walking speed significantly reduced the risk of hip fracture [39].
Demographic differences such as age, gender and ethnicity are all commonly known risk factors for hip fracture [2]. As age increases the likelihood of a hip fracture increases. Females are known to have a higher risk of hip fracture than males as they are more likely to develop osteoporosis and have lower bone mineral density. In this study, females had a higher number of significant risk factors than did men, suggesting there are more risks common to females. People with different ethnic backgrounds have differing risks for hip fracture in the current study and in previous hip fracture risk studies [6, 40, 41]. The level of risk for hip fracture in Māori and Pasifika people has not been researched recently, however, an earlier New Zealand study noted that Māori males are less likely to have a hip fracture than non-Māori and female Māori [17]. In the current study after adjusting for age and sex, Māori (SHR 0.37, p < 0.001) and Asian (SHR 0.38, p < 0.001) participants had the lowest risk of hip fracture, followed by Pasifika (SHR 0.48, p < 0.001) participants; individuals who were classified as other ethnicities had the highest risk of fracture but the group was small and diverse therefore, no substantial conclusions can be made about that group. Earlier research on ethnic differences for hip fracture found that individuals of Polynesian descent, including Pasifika people, tend to be less at risk of hip fracture than European individuals due to a higher BMD [16]. Reid et al. found there was no difference in BMD between Māori and Polynesian individuals [42]. This is consistent with our study, which found that Māori and Pasifika have a lower risk of hip fracture than European individuals. In addition to ethnic differences in BMD, there may be differences in other parameters of bone strength that contribute to the observed ethnic variation in fracture rates. For example, prior literature shows that Asian people tend to have a reduced risk of hip fracture as compared with people of European descent despite having lower BMI on average [41], which may be explained by shorter femoral necks among Asian people [16]. Further research to identify ethnic-specific risk factors may be beneficial.
Tobacco use has been associated with hip fracture risk in previous studies [7, 43, 44]. A study by Kanis et al. determined that non-smokers had the lowest risk of sustaining a hip fracture and current smokers had a higher risk of hip fracture than people who no longer smoke [43]. Research conducted around recovery after hip fracture suggests that smokers have longer recovery times and more complications after a fracture [45, 46].
Literature on hip fracture risk suggests that Parkinson’s disease is a potential risk for hip fracture [47]. Our study found that, Parkinson’s disease was significantly associated with hip fracture risk. People with a diagnosis of Parkinson’s disease were more likely to sustain a hip fracture than those with no diagnosis (SHR 1.45, p < 0.05). Individuals with Parkinson’s disease have a higher risk of falling and thus are more likely to have an increased risk of hip fracture [2, 47, 48].
Shortness of breath was associated with a reduced risk of hip fracture. This variable has not explicitly been studied in the literature. People who have shortness of breath are potentially less likely to be involved in activities that can lead to hip fracture.
There have been three other known studies identified that look specifically at hip fracture risk in a home care population. The first paper, from Canada, found risk factors for hip fracture to be female gender, older age, osteoporosis, falls, unsteady gait, use of ambulation aid, tobacco use, severe malnutrition and cognitive impairment. Arthritis and morbid obesity were found to be protective factors [7]. Our study also found female gender, older age, falls and tobacco use to be significant. Risk factors that were significant in our model but not in the Canadian model were prior hip fracture, shortness of breath, BMI, and wandering. Differences between the models could be due to the different statistical techniques used, the different version of assessment or the different nationalities of the cohorts. Canada uses the MDS, an older version of the assessment used in New Zealand, and so not all questions are the same. For instance, osteoporosis is not assessed in the New Zealand interRAI-HC so its associated risk could not be determined. The other two studies, from New Zealand, looked at specific variables, the first study found that urinary incontinence was an independent risk factor for falls but not for hip fractures [18]. Our study also found urinary incontinence was non-significant. The second study, found that medications specific to the drug burden index (DBI) were significant for hip fracture risk [14]. While the interRAI-HC contains some medications, the list is not comprehensive and medications were omitted from this analysis.
Limitations of the study
There are well-known risk factors for hip fracture that could not be explored using the interRAI -HC assessment. For example, the interRAI version used for this study does not contain osteoporosis as a diagnosis, therefore those with osteoporosis may be at a higher risk of hip fracture but they are unable to be identified within the cohort. Osteoporosis is a known-risk factor for hip fracture as it causes weakening of the bones, leading to a higher probability of fracture [2]. Another common risk factor for hip fracture is low BMD, however, determining the level of BMD in a person requires them to undergo testing in a hospital [49]. As those requiring a home care assessment are usually more frail than the typical population of older adults, measuring BMD can be burdensome [10]. Identifying risk factors within the interRAI-HC assessment initially, for people who are frail can be used as a way of identifying people at an elevated risk of fracture. The FRAX [50] and Garvan [51, 52] scores are commonly used in assessing a person’s hip fracture risk. However, both scores are calculated in a clinical setting which would require the individual to visit their general practitioner to carry out the assessment. As those undergoing a home care assessment are generally frailer than the general population of older people, it may be easier to estimate fracture risk as part of their interRAI assessment.
Within the interRAI-HC BMI recordings are low with around 40% of individuals having no recorded BMI [24]. This is largely due to it being difficult to measure height and weight data for some of the more frail older people, particularly those who are bed or wheelchair bound. However, the results from the known BMI’s were significant which suggests BMI is an important factor in determining a person’s hip fracture risk.
This study was conducted using New Zealand data and may not be generalizable to a wider international audience, however the results may be generalizable to other home care audiences. The interRAI-HC assesses the health needs of people who have complex issues and may not be generalizable to a healthier cohort of people aged 65+ years.
Summary of the implications of the work for practice and research
The New Zealand healthy ageing strategy aims to support people with high and complex needs, such as those using home care services, to ensure they can live as independently as possible [53]. The interRAI-HC is useful for assessing the needs of these people to ensure appropriate care is implemented. Individuals receiving home care have different needs to a general population of older adults [7]. Hip fractures cause significant disability for many older adults, with some of the worst outcomes for those aged 65 years or older. Now that risk factors for hip fracture have been identified for community-dwelling older people; further work can be done to create a risk score to identify those who are at a relatively high risk of hip fracture using the questions within the interRAI-HC assessment. Further work will be done using these variables to develop a prediction model to the randomly omitted data to determine their psychometric utility in screening for hip fracture risk.
Conclusions
Falls, previous hip fractures, being underweight, older age, female gender, prone to wandering, a diagnosis of Parkinson’s disease, and being a smoker all contribute to hip fracture risk. Being overweight, and having shortness of breath can decrease the risk of hip fracture. Individuals who are not of European ethnicity were found to have a reduced risk of hip fracture. These risk factors agree with international work on risk factors for hip fracture and in the future this information could be used to predict hip fracture risk in older people as a routine part of their health assessment.
Abbreviations
- ARC:
-
Aged Residential Care
- BMD:
-
Bone Mineral Density
- BMI:
-
Body Mass Index
- CI:
-
Confidence Interval
- COPD:
-
Chronic Obstructive Pulmonary Disease
- CPS:
-
Cognitive Performance Scale
- DBI:
-
Drug Burden Index
- ICD-10 AM:
-
International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Australian Modification
- interRAI-HC:
-
international Residential Assessment Instrument, Home Care
- MDS:
-
Minimum Dataset
- MORT:
-
Mortality Collection
- NHI:
-
National Health Index
- NMDS:
-
National Minimum Dataset
- RECORD:
-
REporting of Studies Conducted using Observational Routinely collected Data
- SHR:
-
Subhazard Ratio
- STROBE:
-
STrengthening the Reporting of OBservational studies in Epidemiology
- TAS:
-
Technical Advisory Services
References
Keller JM, Sciadini MF, Sinclair E, O'toole RV. Geriatric trauma: demographics, injuries, and mortality. J Orthop Trauma. 2012;26(9):e161–5.
Marks R. Hip fracture epidemiological trends, outcomes, and risk factors, 1970–2009. Int J Gen Med. 2010;3:1–17.
Ariza-Vega P, Jiménez-Moleón JJ, Kristensen MT. Change of residence and functional status within three months and one year following hip fracture surgery. Disabil Rehabil. 2014;36(8):685–90.
English B: Social investment analytics layer launch. In.; 2016.
People aged 65+ living in New Zealand [https://www.stats.govt.nz/infographics/people-aged-65-plus-living-in-new-zealand].
Berry SD, Lee Y, Zullo AR, Kiel DP, Dosa D, Mor V. Incidence of hip fracture in US nursing homes. J Gerontol Ser A: Biomed Sci Med Sci. 2016;71(9):1230–4.
Stolee P, Poss J, Cook RJ, Byrne K, Hirdes JP. Risk factors for hip fracture in older home care clients. J Gerontol Ser A: Biomed Sci Med Sci. 2009;64(3):403–10.
Hippisley-Cox J, Coupland C. Predicting risk of osteoporotic fracture in men and women in England and Wales: prospective derivation and validation of QFractureScores. Bmj. 2009;339:b4229.
Pisani P, Renna MD, Conversano F, Casciaro E, Di Paola M, Quarta E, Muratore M, Casciaro S. Major osteoporotic fragility fractures: risk factor updates and societal impact. World J Orthop. 2016;7(3):171.
Berry SD, Zullo AR, Lee Y, Mor V, McConeghy KW, Banerjee G, D’Agostino Sr RB, Daiello L, Dosa D, Kiel DP. Fracture risk assessment in long-term care (FRAiL): development and validation of a prediction model. The J Gerontol: Ser A. 2017;73(6):763–69.
Margolis KL, Ensrud KE, Schreiner PJ, Tabor HK. Body size and risk for clinical fractures in older women. Ann Intern Med. 2000;133(2):123–7.
Kanis JA, Borgstrom F, De Laet C, Johansson H, Johnell O, Jonsson B, Oden A, Zethraeus N, Pfleger B, Khaltaev N. Assessment of fracture risk. Osteoporos Int. 2005;16(6):581–9.
Marks R. Physical activity and hip fracture disability: a review. J Aging Res. 2011;2011.
Jamieson HA, Nishtala PS, Scrase R, Deely JM, Abey-Nesbit R, Hilmer SN, Abernethy DR, Berry SD, Mor V, Lacey CJ, et al. Drug burden index and its association with hip fracture among older adults: a national population-based study. J Gerontol: Ser A. 2018:gly176.
Cauley JA, Chalhoub D, Kassem AM, Fuleihan GE-H. Geographic and ethnic disparities in osteoporotic fractures. Nat Rev Endocrinol. 2014;10(6):338–51.
Chin K, Evans M, Cornish J, Cundy T, Reid I. Differences in hip axis and femoral neck length in premenopausal women of Polynesian, Asian and European origin. Osteoporos Int. 1997;7(4):344–7.
Barber J, Mills H, Horne G, Purdie G, Devane P. The incidence of hip fractures in Maori and non-Maori in New Zealand. N Z Med J. 1995;108(1007):367–8.
Schluter PJ, Arnold EP, Jamieson HA. Falls and hip fractures associated with urinary incontinence among older men and women with complex needs: a national population study. Neurourol Urodyn. 2018;37(4):1336–43.
Nishtala PS, T-y C. Zopiclone use and risk of fractures in older people: population-based study. J Am Med Dir Assoc. 2017;18(4):368. e361–8.
Grundstrom AC, Guse CE, Layde PM. Risk factors for falls and fall-related injuries in adults 85 years of age and older. Arch Gerontol Geriatr. 2012;54(3):421–8.
Kanis JA, Oden A, Johnell O, Johansson H, De Laet C, Brown J, Burckhardt P, Cooper C, Christiansen C, Cummings S, et al. The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int. 2007;18(8):1033–46.
Berry SD, Ngo L, Samelson EJ, Kiel DP. Competing risk of death: an important consideration in studies of older adults. J Am Geriatr Soc. 2010;58(4):783–7.
Szychowski JM, Roth DL, Clay OJ, Mittelman MS. Patient death as a censoring event or competing risk event in models of nursing home placement. Stat Med. 2010;29(3):371–81.
Schluter PJ, Ahuriri-Driscoll A, Anderson TJ, Beere P, Brown J, Dalrymple-Alford J, David T, Davidson A, Gillon DA, Hirdes J. Comprehensive clinical assessment of home-based older persons within New Zealand: an epidemiological profile of a national cross-section. Aust N Z J Public Health. 2016;40(4):349–55.
Hirdes JP, Ljunggren G, Morris JN, Frijters DH, Soveri HF, Gray L, Björkgren M, Gilgen R. Reliability of the interRAI suite of assessment instruments: a 12-country study of an integrated health information system. BMC Health Serv Res. 2008;8(1):277.
National Minimum Dataset (hospital events) [https://www.health.govt.nz/nz-health-statistics/national-collections-and-surveys/collections/national-minimum-dataset-hospital-events].
Mortality Collection [https://www.health.govt.nz/nz-health-statistics/national-collections-and-surveys/collections/mortality-collection].
Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, Sørensen HT, von Elm E, Langan SM, Committee RW. The REporting of studies conducted using Observational routinely-collected health data (RECORD) statement. PLoS Med. 2015;12(10):e1001885.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496–509.
Corporation I. IBM SPSS statistics for windows. In., 22.0 edn. Armonk, NY: IBM Corporation; 2013.
StataCorp: Stata version 15.0. College Station, TX: StataCorp LP 2017.
Morris JN, Fries BE, Mehr DR, Hawes C, Phillips C, Mor V, Lipsitz LA. MDS cognitive performance scale©. J Gerontol. 1994;49(4):174–82.
Hayes WC, Myers E, Robinovitch S, Van Den Kroonenberg A, Courtney AC, McMahon T. Etiology and prevention of age-related hip fractures. Bone. 1996;18(1):S77–86.
Hamdy RC. Fracture risk assessment in postmenopausal women. Rev Endocr Metab Disord. 2010;11(4):229–36.
Pluijm SM, Koes B, de Laet C, Van Schoor NM, Kuchuk NO, Rivadeneira F, Mackenbach JP, Lips P, Pols HA, Steyerberg EW. A simple risk score for the assessment of absolute fracture risk in general practice based on two longitudinal studies. J Bone Miner Res. 2009;24(5):768–74.
De Laet C, Kanis J, Odén A, Johanson H, Johnell O, Delmas P, Eisman J, Kroger H, Fujiwara S, Garnero P. Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int. 2005;16(11):1330–8.
Armstrong ME, Spencer EA, Cairns BJ, Banks E, Pirie K, Green J, Wright FL, Reeves GK, Beral V. Body mass index and physical activity in relation to the incidence of hip fracture in postmenopausal women. J Bone Miner Res. 2011;26(6):1330–8.
Prieto-Alhambra D, Premaor MO, Fina Avilés F, Hermosilla E, Martinez-Laguna D, Carbonell-Abella C, Nogués X, Compston JE, Díez-Pérez A. The association between fracture and obesity is site-dependent: a population-based study in postmenopausal women. J Bone Miner Res. 2012;27(2):294–300.
Harvey NC, Odén A, Orwoll E, Lapidus J, Kwok T, Karlsson MK, Rosengren BE, Ribom E, Cooper C, Cawthon PM. Measures of physical performance and muscle strength as predictors of fracture risk independent of FRAX, falls, and aBMD: a meta-analysis of the osteoporotic fractures in men (MrOS) study. J Bone Miner Res. 2018.
Wright NC, Saag KG, Curtis JR, Smith WK, Kilgore ML, Morrisey MA, Yun H, Zhang J, Delzell ES. Recent trends in hip fracture rates by race/ethnicity among older US adults. J Bone Miner Res. 2012;27(11):2325–32.
Barrett-Connor E, Siris ES, Wehren LE, Miller PD, Abbott TA, Berger ML, Santora AC, Sherwood LM. Osteoporosis and fracture risk in women of different ethnic groups. J Bone Miner Res. 2005;20(2):185–94.
Reid I, Mackie M, Ibbertson H. Bone mineral content in Polynesian and white New Zealand women. Br Med J (Clin Res Ed). 1986;292(6535):1547–48.
Kanis JA, Johnell O, Odén A, Johansson H, De Laet C, Eisman J, Fujiwara S, Kroger H, McCloskey E, Mellstrom D. Smoking and fracture risk: a meta-analysis. Osteoporos Int. 2005;16(2):155–62.
Melhus H, Michaëlsson K, Holmberg L, Wolk A, Ljunghall S. Smoking, antioxidant vitamins, and the risk of hip fracture. J Bone Miner Res. 1999;14(1):129–35.
Sloan A, Hussain I, Maqsood M, Eremin O, El-Sheemy M. The effects of smoking on fracture healing. Surgeon. 2010;8(2):111–6.
Scolaro JA, Schenker ML, Yannascoli S, Baldwin K, Mehta S, Ahn J. Cigarette smoking increases complications following fracture: a systematic review. J Bone Joint Surg. 2014;96(8):674–81.
Sato Y, Kaji M, Tsuru T, Oizumi K. Risk factors for hip fracture among elderly patients with Parkinson’s disease. J Neurol Sci. 2001;182(2):89–93.
Boonen S, Dequeker J, Pelemans W. Risk factors for falls as a cause of hip fracture in the elderly. Acta Clin Belg. 1993;48(3):190–4.
Bensen R, Adachi JD, Papaioannou A, Ioannidis G, Olszynski WP, Sebaldt RJ, Murray TM, Josse RG, Brown JP, Hanley DA. Evaluation of easily measured risk factors in the prediction of osteoporotic fractures. BMC Musculoskelet Disord. 2005;6(1):47.
Frax W: Fracture risk assessment tool. In.; 2008.
Nguyen ND, Frost S, Center JR, Eisman JA, Nguyen T. Development of a nomogram for individualizing hip fracture risk in men and women. Osteoporos Int. 2007;18(8):1109–17.
Nguyen ND, Frost SA, Center J, Eisman JA, Nguyen TV. Development of prognostic nomograms for individualizing 5-year and 10-year fracture risks. Osteoporos Int. 2008;19(10):1431–44.
Health NZMo: Healthy Ageing Strategy: New Zealand Government - Ministry of Health; 2016.
Acknowledgements
Technical Advisory Services (TAS) for providing access to the interRAI-HC data and to the Ministry of Health (MoH) for providing mortality and hospital admissions data.
Funding
Not applicable.
Availability of data and materials
The data that support the findings of this study are available from Technical Advisory Services (TAS) but restrictions apply to the availability of these data, which were used under license for the current study, and are not publicly available. Data are however available from the authors upon reasonable request and with permission of Technical Advisory Services (TAS).
Author information
Authors and Affiliations
Contributions
R A-N Wrote draft manuscript and conducted statistical analyses. PS Assisted with analysis of results and made substantive revisions to the manuscript. TW Provided clinical advice and made substantive revisions to the manuscript. JT Conducted an initial literature review and provided clinical advice and manuscript feedback. SB Made substantive revisions to the manuscript and assisted with the analysis design. HJ Made substantive contributions to the conception and design of the study and provided manuscript feedback. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Permission for this study was approved by the Ministry of Health’s Health and Disability, Ethics Committee (14/STH/140) and only includes anonymised data provided by those who verbally consented as part of their interRAI-HC assessment to their information being used for planning and research purposes. Only those who agreed for their data being used in this way will have their data released for research purposes. The ethics committee agrees with this procedure.
Consent for publication
Not applicable.
Competing interests
The author’s declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Supplementary Materials for Risk Factors for hip fracture in New Zealand older adults seeking home care services – A national population cross-sectional study. Table S1. is a record of the variables used for analysis from questions based on the interRAI-HC version 9.1 with New Zealand specifications. The table contains information on the question number and how the questions were recoded for the purposes of analysis. (DOCX 21 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Abey-Nesbit, R., Schluter, P.J., Wilkinson, T. et al. Risk factors for hip fracture in New Zealand older adults seeking home care services: a national population cross-sectional study. BMC Geriatr 19, 93 (2019). https://doi.org/10.1186/s12877-019-1107-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-019-1107-1