Abstract
Backgrounds
The purpose of this study was to examine, in a sample of Japanese older adults, the associations of objectively-assessed sedentary behavior (SB) and physical activity (PA) with performance-based physical function. The isotemporal substitution (IS) approach was used to model simultaneously the effects of the specific activity being performed and the activity being displaced, in an equal time-exchange manner.
Methods
Among 287 older adults (65–84 years), we used accelerometers to identify the daily average time spent on SB (≤1.5 METs); light-intensity PA (LIPA) (>1.5 to <3.0 METs); and moderate- to vigorous-intensity PA (MVPA) (≥3.0 METs). Physical function was assessed using five performance-based measures: hand grip strength, usual and maximum gait speeds, timed up and go, and one-legged stance with eyes open. We employed three linear regression models – a single-activity model, a partition model, and an IS model – to assess the associations of SB, LIPA, and MVPA with each of the five measures of physical function.
Results
There were significant positive associations in the single-activity and partition models between MVPA and the measures of physical function (with the exception of hand grip strength). The IS models found that replacing SB or LIPA with MVPA was significantly and favorably associated with physical function measures.
Conclusions
These findings indicate that replacing small amounts of SB and LIPA with MVPA (such as 10 min) may contribute to improvements in older adults’ physical function.
Similar content being viewed by others
Background
Physical function is a key component of health for older adults. Decline in physical function has been found to be closely related to disability and mortality [1, 2]. With the progression of aging in the world, extending healthy life expectancy, which is defined as the length of time an individual lives without limitations in their daily activities, is increasingly seen as a top priority in public health (e.g., Healthy People 2020 in the U.S.A., World Report on Aging and Health by WHO, and the National Health Promotion Movement in the twenty-first century in Japan) [3,4,5]. Therefore, more research to better understand factors that can help older adults maintain their physical function is needed to contribute to this priority [6].
Moderate- to vigorous-intensity physical activity (MVPA) is favorably associated with older adults’ physical function [7, 8]. Recent studies have shown that light-intensity physical activity (LIPA: e.g., some household work and slow walking) and sedentary behavior (SB: e.g., television viewing, computer use, and sitting in cars) are related to physical function in older adults [9,10,11,12]. For example, a longitudinal study examining associations of physical activity (PA) levels with functional status among older women found those who kept being active during a 14-year period had the best functional status [13]. Another study examining the cross-sectional associations of objectively-measured PA with physical health (including physical function) found LIPA to be positively associated with physical health among older adults [14]. Another cross-sectional study found older adults with lower levels of SB and a greater number of breaks in sitting time had significantly better physical function adjusting for MVPA [11].
However, there is a methodological concern in previous studies examining the relationships between PA levels and physical function. Since the total hours in a day are fixed; SB, LIPA, and MVPA are inter-related: increasing one behavior results in a reduction of other behaviors. Such substitutional relationships between behaviors need to be considered when research examines how a particular activity is associated with health outcomes. Nevertheless, there is only one previous study examining the potential benefits on older adults’ physical health when SB is replaced with LIPA or MVPA [9]. Buman et al. [9] found replacing 30 min/day of SB with LIPA to be positively associated with physical health, including physical function, among older adults. However, physical health in their study was assessed using a self-reported questionnaire, which has several limitations in terms of accuracy, validity, and reproducibility [15, 16]. There is thus the need to examine how performance-based physical function among older adults is associated with SB, LIPA and MVPA, considering their complementary relationships.
The aim of this study was to examine the associations of objectively-assessed SB, LIPA, and MVPA with performance-based physical function in a sample of Japanese older adults, using an isotemporal substitution (IS) approach to model simultaneously the effects of the specific activity being performed and the activity being displaced, in an equal time-exchange manner.
Methods
Participants and procedures
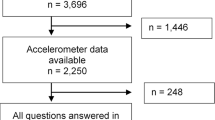
Participants were drawn from a larger epidemiological study conducted in Matsudo city, Chiba Prefecture, Japan. Matsudo city is located 20 km north of Tokyo with approximately half a million residents in 2016. To recruit the participants, first a randomly-selected 3000 people aged 65 to 84 years from the registry of residential addresses were contacted by an invitation letter. Of these, 951 agreed to participate in the main study, and 349 took part in a sub-study, in which PA and physical function were assessed objectively. Participants received a book voucher as compensation. All participants provided written informed consent. The study was approved by the Waseda University Institutional Committee on Human Research (2013–265) and the Institutional Review Board of Chiba Prefectural University of Health Sciences (2012–042).
Physical activity and sedentary behavior
The participants’ PA was assessed using an accelerometer (Active style Pro HJA-350IT, Omron Healthcare, Kyoto, Japan). The detailed algorithm and validity of the accelerometer device have been described elsewhere [17,18,19]. Briefly, the device (74 × 34 × 46 mm; 60 g) measures anteroposterior (x-axis), mediolateral (y-axis), and vertical (z-axis) acceleration signals. The integral of the absolute value of the accelerometer output during a 60-s interval was calculated and converted into the total energy expenditure. The device estimates the intensity of activity by METs using a built-in algorithm. The CSV data files from the accelerometer were downloaded by Omron health management software BI-LINK for PA professional edition version 1.0 and then the files were processed by custom software (Custom-written Macro program for compiling data). A previous study, in which METs for household and locomotive activities were calculated, reported a linear relationship between filtered synthetic accelerations with PA intensity [18]. Participants were asked to wear the accelerometer on their waist for at least 7 days —except when sleeping or during water-based activities (e.g., bathing, showering, and swimming). To be eligible, participants needed to wear the accelerometer for ≥4 days (including 1 weekend day), with at least 10 h/day of wear time each day [20]. Non-wear time was defined as at least consecutive 60 min of 0 counts per minute (cpm), with allowance for up to 2 min of some limited movement (<50 cpm) within those periods [20]. For those who met the inclusion criteria, the daily average time spent on SB (≤1.5 METs), LIPA (>1.5 to <3.0 METs) and MVPA (≥3.0 METs) were calculated. These MET levels have been used by previous studies examining functional decline among older adults [21, 22].
Physical function
Physical function was assessed using five performance-based functional tests: hand grip strength (upper body strength), usual and maximum gait speeds (gait speed), timed up and go (TUG) (mobility), and one-legged stance with eyes open (balance). Hand grip strength was measured using a Smedley-type handgrip dynamometer (TKK5041, Takei Scientific Instruments Co., Ltd., Niigata, Japan). We chose this type of handgrip device (rather than the Jamar dynamometer), because it is the most widely used method for evaluating hand grip strength in Japanese health studies [23]. Participants stood with their arms hanging naturally at their sides holding the dynamometer with the grip size adjusted to a comfortable level. They were instructed to squeeze the handgrip as hard as possible. Participants performed one trial with the dominant hand (to the nearest 0.1 kg). Usual and maximum gait speeds were measured using an 11 m course. Participants started walking at their normal or maximum paces, and time to walk 5 m was measured, starting when the body trunk passed the 3-m mark and ending when the body trunk passed the 8-m mark. Gait speed was calculated as distance divided by walking time (m/s). Usual gait speed was measured twice, and the faster of the two results (to the nearest 0.1 m/s) was used. Maximum gait speed was measured once. TUG measured the time for participants to complete the following sequence: start from a seated position in an armless chair; stand up from the chair and walk as fast as possible toward a pole placed 3 m in front of the chair, turn around the pole; and return to the chair and sit. TUG was conducted twice, and the faster of the two results (to the nearest 0.1 s) was used. One-legged stance with eyes open was measured using a participant’s preferred leg. Participants raise one leg and stand as long as possible. They were timed until they lost their balance or reached the maximum of 60 s. Participants performed two trials, and the longer of the two results (to the nearest 0.1 s) was used.
Covariates
The following individual-level variables were considered as potential confounders: age, gender, body mass index (BMI), the number of past illnesses, complications and comorbidity, smoking status, drinking status, living arrangement, and highest educational attainment. The BMI was calculated using objectively-measured height and weight.
Statistical analysis
Three multiple linear regression models including single-activity model, partition model, and IS model were used to examine the associations of SB, LIPA, and MVPA for each of the five items of physical function. We used 10 min as a unit for activity, thus the IS models examined the effect of replacing a 10-min of one activity with the same amount of another activity. This time unit was chosen for two reasons; this is the minimum amount of time in which activities should be accrued to meet current PA guidelines [7] and Japanese official PA guidelines for health promotion recommended trying to move for an additional 10 min a day for longer healthy life expectancy [24].
The single-activity model assessed each activity component separately (e.g., SB only), without taking into account the other activity types, but adjusting for total wear time and confounders. The model (in the case of SB) is expressed as follows:
Outcome variable = (b0) SB + (b3) total wear time + (b4) covariates.
The partition model examined all the behaviors simultaneously, without adjusting for total wear time. It is expressed as follows:
Outcome variable = (b0) SB + (b1) LIPA + (b2) MVPA + (b4) covariates.
In this model, the coefficient for one type of activity represents the effect of increasing this type of activity while holding the other activities constant. Since the total wear time is not included in the model (thus is not held constant), it represents the effects of adding rather than substituting an activity type.
The IS model estimates the effect of substituting one activity type with another for the same amount of time (e.g., replacing MVPA with SB, by removing SB from the model). The IS model (in the case of omitting SB from the model) is expressed as follows:
Outcome variable = (b1) LIPA + (b2) MVPA + (b3) total wear time + (b4) covariates.
The coefficients b1 and b2 in this model represent the effect of a 10-min substitution of SB with one of the activity types (LIPA or MVPA) while holding the other activity types and total wear time constant. For instance, b1 can be interpreted as the effect of replacing SB with LIPA for 10 min while holding MVPA and total wear time constant.
All the statistical contrasts were made at the 0.05 level of significant. Analyses were conducted using IBM SPSS Statistics 20.0 (IBM Japan Corp., Tokyo, Japan).
Results
After excluding participants with missing covariates and lacking valid PA accelerometer data, the final sample consisted of 287 people (180 men, 107 women). Table 1 shows the characteristics of the study sample. The mean number of valid days of participant’s wearing accelerometer was 7.2 days (SD: 0.9). On average, participants wore accelerometer for 15 h/day, and the mean proportion of SB, LIPA, and MVPA duration to total accelerometer wear time were 58%, 36%, and 6%, respectively. These proportions were almost similar with those reported (the mean proportion of SB, LIPA, and MVPA duration were 64%, 31%, and 5% in men, and 54%, 41%, 5% in women) by the only previous study examined patterns of objective SB and PA among Japanese older adults [25]. Correlation coefficients were −0.67 between SB and LIPA, −0.36 between SB and MVPA, and 0.24 between LIPA and MVPA. Scores of performance-based functional tests (except for maximum gait speeds and TUG) were relatively high compared with the sample of Japanese community older population [26, 27].
In the single-activity model (Table 2), MVPA was significantly and favorably associated with usual (p < .001) and maximum gait speeds (p < .001), TUG (p < .001), and one-legged stance with eyes open (p < .01). SB was significantly and negatively associated with usual (p < .01) and maximum gait speeds (p < .05) and TUG (p < .01). No significant association was observed for LIPA. In the partition model (Table 3), MVPA was the only activity that was associated with physical function outcomes. It was significantly and favorably associated with usual (p < .001) and maximum gait speeds (p < .001), TUG (p < .001), and one-legged stance with eyes open (p < .001). In the IS model (Table 4), each 10-min unit of SB or LIPA replaced with MVPA were significantly and favorably associated with usual (replacing SB: p < .001, replacing LIPA: p < .01) and maximum gait speeds (replacing SB: p < .001, replacing LIPA: p < .001), TUG (replacing SB: p < .001, replacing LIPA: p < .001), and one-legged stance with eyes open (replacing SB: p < .01, replacing LIPA: p < .01).
Discussion
This study examined the associations of objectively-measured SB, LIPA, and MVPA with performance-based physical function measures among Japanese older adults. Several recent public health recommendations advocate reducing SB and increasing MVPA for maintaining better health [24, 28]. Our analysis using the IS model provides empirical evidence supporting these recommendations.
Previous studies have consistently reported that MVPA has favorable effects on various health outcomes including physical function in older adults [7, 29]. Consistent with these studies, we found MVPA to be positively and significantly associated with older adults’ physical function (except for hand grip strength) in a single-activity model (total time held constant) and a partition model (other activity variables held constant). In addition, our findings showed that replacing SB or LIPA with MVPA had beneficial effects on participants’ physical function, except for hand grip strength. These results indicated that replacing a small amount of SB or LIPA (such as 10 min) with equal time of MVPA during one day was associated with 1.4 to 2.7% better function scores. It should be noted that no significant associations were observed for hand grip strength, which is often used as an overall measure of body strength [23]. This is plausible as PA measured in this study mainly involves lower limb muscles, for which mixed associations with hand grip strength have been reported [30]. It has been also found that correlation between hand grip strength and lower limb muscle strength tends to be weaker among older adults compared with younger adults [31]. Several previous studies using the IS approach reported benefits of replacing relatively long time of SB (e.g. 30 to 60 min) with MVPA on health outcomes [32, 33]. However, replacing 30 or 60 min of SB with MVPA during one day may be practically difficult for older adults.
Recent studies have demonstrated the favorable effects of LIPA on health in older population [9, 12]. Based on these findings, it is possible to posit that replacing SB with LIPA may be beneficial to older adults’ physical function. However, our results did not show beneficial effects of replacing SB with LIPA. In addition, the regression coefficients in the IS models where SB was replaced with MVPA and that where LIPA was replaced with MVPA were almost the same for gait speeds and TUG. Several studies found MVPA to have beneficial effects on muscle strength, but not LIPA [34, 35]. Better physical function requires sufficient muscle strength, which may not be obtained by LIPA. In addition, the LIPA in our study may include household chores (e.g., cooking, washing dishes, ironing, and house cleaning). It is possible that the nature of these activities may have contributed to lack of a significant improvement in physical function when they are substituted by sitting time. This suggests that LIPA may be associated with self-reported or mental health of older adults, but may not be intense enough to be related to their physical function. Another possibility is misclassification of activity intensity in previous studies: LIPA may have included relatively strong intensity activities such as gardening [36]. Also, some previous studies classified objectively-measured LIPA into two categories: low-light intensity PA (>1.5 to <2.0 METs) and high-light intensity PA (≥2.0 to <3.0 METs), and reported that they are associated differently with health outcomes including physical function [9, 14]. Such co-existence of activities with different intensities within LIPA may have played a role in the relationships observed in the study. Further research using comprehensive health outcomes is needed to understand whether and to what extent LIPA is beneficial to older adults’ health.
This study has some limitations. First, the accelerometer did not assess activities involving only upper or lower limbs without trunk movement (e.g., some household work and cycling) and water-based PA (e.g. swimming or underwater walking). Second, as a cross-sectional study, we are unable to infer a cause-and-effect relationship between SB, PA, and physical function. This is an important issue because behavior pattern may be a reflection of functional status. Future longitudinal studies are needed to address this limitation. Third, the participants in this study were not a representative sample of Japanese older (i.e., more active and healthy). Further research using an intervention design with a large and diverse sample is needed to further understand about cause-and-effect relationship between different levels of activity and older adults’ physical function. The strength of this study was the use of objectively-measured behaviors and performance-based physical function.
Conclusions
Our findings indicated that replacing even small amounts of SB (e.g. watching TV and working at a desk) with MVPA (e.g. brisk walking and exercise/sport) may contribute to improvements in physical function in older adults. Potential favorable effects were identified for replacing only 10 min per day of SB with MVPA.
Abbreviations
- BMI:
-
Body mass index
- IS:
-
Isotemporal substitution
- LIPA:
-
Light-intensity physical activity
- MVPA:
-
Moderate- to vigorous-intensity physical activity
- PA:
-
Physical activity
- SB:
-
Sedentary behavior
- TUG:
-
Timed up and go
References
Justice JN, Cesari M, Seals DR, Shively CA, Carter CS. Comparative approaches to understanding the relation between aging and physical function. J Gerontol A Biol Sci Med Sci. 2016;71:1243–53.
Pavasini R, Guralnik J, Brown JC, di Bari M, Cesari M, Landi F, et al. Short physical performance battery and all-cause mortality: systematic review and meta-analysis. BMC Med. 2016;14:215.
The U.S. Department of Health and Human Services: Healthy People. gov. https://www.healthypeople.gov/ (2014) Accessed 8 Aug 2017.
Ministry of Health, Labour and Welfare in Japan: The second term of national health promotion movement in the twenty first century. http://www.mhlw.go.jp/seisakunitsuite/bunya/kenkou_iryou/kenkou/kenkounippon21/en/kenkounippon21/ (2013) Accessed 8 Aug 2017.
World Health Organization: World report on ageing and health. http://www.who.int/ageing/events/world-report-2015-launch/en/ (2015)Accessed 8 Aug 2017.
Vaughan L, Leng X, La Monte MJ, Tindle HA, Cochrane BB, Shumaker SA. Functional independence in late-life: maintaining physical functioning in older adulthood predicts daily life function after age 80. J Gerontol A Biol Sci Med Sci. 2016;71(Suppl 1):79–86.
Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1094–105.
Miszko TA, Cress ME, Slade JM, Covey CJ, Agrawal SK, Doerr CE. Effect of strength and power training on physical function in community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2003;58:171–5.
Buman MP, Hekler EB, Haskell WL, Pruitt L, Conway TL, Cain KL, et al. Objective light-intensity physical activity associations with rated health in older adults. Am J Epidemiol. 2010;172:1155–65.
Dunlop DD, Song J, Arnston EK, Semanik PA, Lee J, Chang RW, et al. Sedentary time in US older adults associated with disability in activities of daily living independent of physical activity. J Phys Act Health. 2015;12:93–101.
Sardinha LB, Santos DA, Silva AM, Baptista F, Owen N. Breaking-up sedentary time is associated with physical function in older adults. J Gerontol A Biol Sci Med Sci. 2015;70:119–24.
Tse AC, Wong TW, Lee PH. Effect of low-intensity exercise on physical and cognitive health in older adults: a systematic review. Sports Med Open. 2015;1:37.
Brach JS, FitzGerald S, Newman AB, Kelsey S, Kuller L, VanSwearingen JM, et al. Physical activity and functional status in community-dwelling older women: a 14-year prospective study. Arch Intern Med. 2003;163:2565–71.
Bann D, Hire D, Manini T, Cooper R, Botoseneanu A, McDermott MM, et al. Light intensity physical activity and sedentary behavior in relation to body mass index and grip strength in older adults: cross-sectional findings from the lifestyle interventions and independence for elders (LIFE) study. PLoS One. 2015;10:e0116058.
Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–94.
Nielsen LM, Kirkegaard H, Ostergaard LG, Bovbjerg K, Breinholt K, Maribo T. Comparison of self-reported and performance-based measures of functional ability in elderly patients in an emergency department: implications for selection of clinical outcome measures. BMC Geriatr. 2016;16:199.
Kurita S, Yano S, Ishii K, Shibata A, Sasai H, Nakata Y, Fukushima N, Inoue S, Tanaka S, Sugiyama T, et al. Comparability of activity monitors used in Asian and western-country studies for assessing free-living sedentary behaviour. PLoS One. 2017;12:e0186523.
Ohkawara K, Oshima Y, Hikihara Y, Ishikawa-Takata K, Tabata I, Tanaka S. Real-time estimation of daily physical activity intensity by a triaxial accelerometer and a gravity-removal classification algorithm. Br J Nutr. 2011;105:1681–91.
Oshima Y, Kawaguchi K, Tanaka S, Ohkawara K, Hikihara Y, Ishikawa-Takata K, Tabata I. Classifying household and locomotive activities using a triaxial accelerometer. Gait Posture. 2010;31:370–4.
Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003-06. Eur Heart J. 2011;32:590–7.
Blair CK, Morey MC, Desmond RA, Cohen HJ, Sloane R, Snyder DC, et al. Light-intensity activity attenuates functional decline in older cancer survivors. Med Sci Sports Exerc. 2014;46:1375–83.
Chmelo E, Nicklas B, Davis C, Miller GD, Legault C, Messier S. Physical activity and physical function in older adults with knee osteoarthritis. J Phys Act Health. 2013;10:777–83.
Kamide N, Kamiya R, Nakazono T, Ando M. Reference values for hand grip strength in Japanese community-dwelling elderly: a meta-analysis. Environ Health Prev Med. 2015;20:441–6.
Miyachi M, Tripette J, Kawakami R, Murakami H. "+10 min of physical activity per day": Japan is looking for efficient but feasible recommendations for its population. J Nutr Sci Vitaminol (Tokyo). 2015;61 Suppl:7–9.
Amagasa S, Fukushima N, Kikuchi H, Takamiya T, Oka K, Inoue S. Light and sporadic physical activity overlooked by current guidelines makes older women more active than older men. Int J Behav Nutr Phys Act. 2017;14:59.
Uritani D, Fukumoto T, Matsumoto D, Shima M. The relationship between toe grip strength and dynamic balance or functional mobility among community-dwelling Japanese older adults: a cross-sectional study. J Aging Phys Act. 2016;24:459–64.
Shinkai S, Watanabe S, Kumagai S, Fujiwara Y, Amano H, Yoshida H, et al. Walking speed as a good predictor for the onset of functional dependence in a Japanese rural community population. Age Ageing. 2000;29:441–6.
Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev. 2010;38:105–13.
Gebel K, Ding D, Chey T, Stamatakis E, Brown WJ, Bauman AE. Effect of moderate to vigorous physical activity on all-cause mortality in middle-aged and older Australians. JAMA Intern Med. 2015;175:970–7.
Visser M, Deeg DJ, Lips P, Harris TB, Bouter LM. Skeletal muscle mass and muscle strength in relation to lower-extremity performance in older men and women. J Am Geriatr Soc. 2000;48:381–6.
Samuel D, Wilson K, Martin HJ, Allen R, Sayer AA, Stokes M. Age-associated changes in hand grip and quadriceps muscle strength ratios in healthy adults. Aging Clin Exp Res. 2012;24:245–50.
Mekary RA, Lucas M, Pan A, Okereke OI, Willett WC, FB H, et al. Isotemporal substitution analysis for physical activity, television watching, and risk of depression. Am J Epidemiol. 2013;178:474–83.
Buman MP, Winkler EA, Kurka JM, Hekler EB, Baldwin CM, Owen N, et al. Reallocating time to sleep, sedentary behaviors, or active behaviors: associations with cardiovascular disease risk biomarkers, NHANES 2005-2006. Am J Epidemiol. 2014;179:323–34.
Chahal J, Lee R, Luo J. Loading dose of physical activity is related to muscle strength and bone density in middle-aged women. Bone. 2014;67:41–5.
Park H, Park S, Shephard RJ, Aoyagi Y. Yearlong physical activity and sarcopenia in older adults: the Nakanojo study. Eur J Appl Physiol. 2010;109:953–61.
Yasunaga A, Park H, Watanabe E, Togo F, Park S, Shephard RJ, Aoyagi Y. Development and evaluation of the physical activity questionnaire for elderly Japanese: the Nakanojo study. J Aging Phys Act. 2007;15:398–411.
Acknowledgements
Not applicable.
Availability of data and material
The data set supporting these findings is not publicly available due to access restrictions imposed by the Waseda University Institutional Committee on Human Research and the Chiba Prefectural University of Health Sciences Ethics Committee. Public data sharing is restricted in order to protect privacy and confidentiality. Data requests from any interested researcher may be sent to the research director (KO): koka@waseda.jp.
Funding
This work was supported by JSPS KAKENHI Grant (15 K01534 and 15K01647) and MEXT-Supported Program for the Strategic Research Foundation at Private Universities (S1511017). Koohsari was supported by the JSPS Postdoctoral Fellowship for Research in Japan (#17716) from the Japan Society for the Promotion of Science. The sponsor had no role in the study design, methods, subject recruitment, data collections, analysis and preparation of paper.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to this work. AY wrote the main paper. AS, KI KJM, and SI conducted the acquisition and analysis of data. KJM, TS and NO modified the manuscript. KO coordinated the research project. All authors discussed the results and implications and commented on the manuscript at all stages. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Waseda University Institutional Committee on Human Research (2013–265) and the Institutional Review Board of Chiba Prefectural University of Health Sciences, Japan (2012–042). All participants gave written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Yasunaga, A., Shibata, A., Ishii, K. et al. Associations of sedentary behavior and physical activity with older adults’ physical function: an isotemporal substitution approach. BMC Geriatr 17, 280 (2017). https://doi.org/10.1186/s12877-017-0675-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-017-0675-1