Abstract
Background
It is well established that the controlling nutritional status (CONUT) score was correlated with long-term outcomes in gastric cancer (GC), but the significance of CONUT for postoperative short-term outcomes remains unclear. The study aimed to characterize the relationship between CONUT and short-term complications following gastrectomy of GC.
Methods
We collected data on 1479 consecutive GC patients at Nanjing Drum Tower Hospital between January 2016 and December 2018. Univariate and multivariate analyses of predictive factors for postoperative complications were performed. The cutoff value of the CONUT score was determined by Youden index.
Results
Among all of the patients, 431 (29.3%) patients encountered postoperative complications. Multivariate analyses identified CONUT was an independent predictor for postoperative short-term complications (OR 1.156; 95% CI 1.077–1.240; P < 0.001). Subgroup analysis elucidated that CONUT was related to postoperative complications both in early gastric cancer and advanced gastric cancer. We further explored that patients with high CONUT score had prolonged hospital stay (12.3 ± 6.0 vs 11.1 ± 4.6, P < 0.001) and more total hospital charges (7.6 ± 2.4 vs 7.1 ± 1.6, P < 0.001).
Conclusions
The present study demonstrated that the preoperative CONUT was an independent predictor for short-term complications following gastrectomy of GC.
Similar content being viewed by others
Background
Gastric cancer (GC) is one of the most common digestive tract cancers worldwide [1]. To this day, radical gastrectomy remains the main option for resectable GC. Despite significant advance has been seen in surgical techniques in recent years, the incidence of complications after radical gastrectomy remains at 15%-25% [2, 3]. Therefore, it is necessary to accurately predict postoperative complications to help perioperative management of GC patients.
Malnutrition is common in GC patients because of a decrease in food intake and energy expenditure. The poor nutritional condition was reported to be correlated with postoperative complications and a worse prognosis [4, 5]. Moreover, immunological status was also regarded as a prognostic marker for GC patients [6, 7]. Several nutritional and inflammatory indicators were monitored routinely before GC surgery, including albumin, total cholesterol, total lymphocytes, hemoglobin, C-reactive protein, neutrophils, and platelet [8,9,10]. Furthermore, more reliable combined scoring systems were developed to accurately predict patient prognoses, such as neutrophil to lymphocyte ratio (NLR), Prognostic Nutritional Index (PNI), and platelet to lymphocyte ratio (PLR) [8, 11, 12].
Controlling nutritional status (CONUT) score is another nutritional scoring system, covering serum albumin, cholesterol, and lymphocyte counts [13]. Recently, several studies elucidated that CONUT was correlated with the long-term prognosis of different kinds of cancer [14,15,16,17,18]. However, it remains controversial whether CONUT could predict short-term outcomes following tumor resection [19, 20]. Also, little is known about the connection between CONUT and postoperative complications of GC [21]. Therefore, this study intended to characterize the significance of CONUT on short-term complications following gastrectomy of GC.
Methods
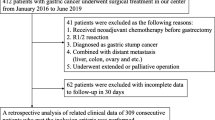
Patients
We collected data on 1479 consecutive GC patients at Nanjing Drum Tower Hospital between January 2016 and December 2018. All patients underwent curative (R0) gastrectomy and were histologically confirmed. Exclusion criteria include (1) incomplete clinical data; (2) Stage 0 cancer; (3) multi-visceral resection; (4) preoperative radiotherapy or chemotherapy; (5) previous stomach surgery.
Data collection
The following three types of parameters were extracted: preoperative, intraoperative, and postoperative characteristics. Preoperative index involved age, sex, body mass index, the American Society of Anesthesiologists (ASA) grade, comorbidities (diabetes mellitus, hypertension, and previous abdominal surgery), and laboratory data (neutrophil count, lymphocyte count, platelet count, serum albumin, C-reactive protein, and total cholesterol). The intraoperative features contained type of resection, surgical approach, operation time, and blood loss. Postoperative characteristics included tumor depth, pTNM stage (7th edition), short-term complications, postoperative stay, and hospital costs. The postoperative short-term complications were defined as morbidity that occurred during hospitalization or within 30 days after surgery. The complications were classified according to the Clavien-Dindo (CD) classification system [22].
Scoring systems of the general condition
Preoperative immune-nutritional and inflammatory scoring systems, including NLR, PLR, PNI, and CONUT, were examined. The NLR and PLR were brought out by dividing the neutrophil and platelet count by the lymphocyte count, respectively [23]. The PNI was obtained from the following formula: (10 × albumin level [g/dL]) + (0.005 × lymphocyte count [number/mm3]) [24]. The CONUT was calculated using serum albumin, total cholesterol concentrations, and total lymphocyte count (Additional file 1: Table S1) [13].
Statistical analysis
Continuous variables were summarized with means ± SD and compared using Student’s t test or Mann–Whitney U test. Categorical variables were summarized with numbers and compared using the Chi squared test or the Fisher exact test. The correlation between postoperative complications and clinicopathological factors were investigated using univariate and multivariate analysis. Variables that were statistically significant in univariate analysis were selected for further multivariate analysis. Binary logistic regression models (Forward: LR) were performed for multivariate analyses. The cut-off value of the CONUT score was determined by Youden index. All P values were two-sided and statistical differences were termed as P value < 0.05. All statistical analyses were carried out in SPSS 19.0 (Chicago, IL, USA).
Results
Patient characteristics
Details of the patient characteristics were summarized in Table 1. This study enrolled 1479 GC patients, including 1083 (73.2%) male and 396 (26.8%) female. The median age was 60 (range: 21–96 years). Diabetes mellitus and hypertension were present in 130 (8.8%) and 485 (32.8%), respectively. Most patients (n = 1403, 94.9%) underwent open gastrectomy. The number of patients who underwent distal gastrectomy, proximal gastrectomy, total gastrectomy was 613 (41.4%), 162 (11.0%), 704 (47.6%), respectively. The overall incidence of postoperative short-term complications was 29.3% (n = 431).
Risk factors correlated with postoperative short-term complications
As shown in Table 2, univariate analyses elucidated that postoperative short-term complications were associated with age, sex, low serum albumin, low total cholesterol, PLR, PNI, CONUT score, type of resection (proximal gastrectomy vs. total gastrectomy), and operation time. Multivariate analyses further revealed that age, gender, CONUT score, type of resection (proximal gastrectomy vs. total gastrectomy), and operation time were independent risk factors for postoperative short-term complications.
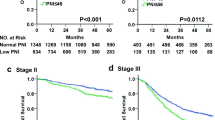
We further explored the relationship between postoperative short-term complications and CONUT score in different pathological stages. Based on the Youden index, the appropriate cut-off value was 2 for the CONUT score. Patients were categorized into two groups: high CONUT score (≥ 2), low CONUT score (< 2). As shown in Table 3, Postoperative complications were more frequent in high CONUT group in stage I/II/III. From another perspective, the CONUT score was associated with postoperative complications both in early gastric cancer and advanced gastric cancer.
Preoperative CONUT score as a predictor for postoperative complications
Of the 1479 patients, 431 (29.3%) encountered postoperative short-term complications, and 64 (4.3%) encountered major complications (grade III or more). The details of postoperative complications were presented in Table 4. Postoperative complications were more frequent in high CONUT group than low CONUT group (33.9% vs 22.6%; p < 0.001). Major complications were also more frequent in the high CONUT group (5.4% vs 2.9%; p = 0.018). Congruently, patients with high CONUT scores had prolonged hospital stay (12.3 ± 6.0 vs 11.1 ± 4.6, P < 0.001) and more hospital costs (7.6 ± 2.4 vs 7.1 ± 1.6, P < 0.001).
Discussion
In this study, we evaluated the predictive ability of various nutritional and inflammatory parameters for short-term complications following gastrectomy of GC, including NLR, PLR, PNI, and CONUT. Only CONUT was found to be statistically correlated with postoperative complications both in univariate and multivariate analyses. These findings revealed that a high CONUT score was a strong predictor for postoperative short-term complications.
CONUT was initially proposed to assess patients' nutritional conditions in 2005 by Gonzalez and colleagues [13]. It was obtained from serum albumin concentration, total cholesterol concentration, and total lymphocyte count. The easy-to-use index could provide a prompt and accurate preoperative evaluation. It has been well established that preoperative CONUT served as a prognostic factor for long-term outcomes in several cancers, including renal cell cancer, hepatocellular cancer, lung cancer, and colorectal cancer [25,26,27,28,29]. As for GC, recent studies also elucidated that CONUT was significantly related to long-term prognosis [14, 30,31,32]. However, the correlation between CONUT and short-term outcomes remained unclear because the number of relevant studies was small [4, 21]. Ryo et al. recently reported that stage II/III GC patients with high preoperative CONUT scores were more likely to suffer postoperative pneumonia [31]. Li et al. elucidated that high CONUT was related to severe postoperative complications [33]. The present study thoroughly accessed the ability of the preoperative CONUT in predicting short-term outcomes following gastrectomy. Our results suggest that the incidence of postoperative overall complications or major complications was higher in patients with high CONUT scores. Furthermore, prolonged hospital stay and more total hospital charges were also observed in patients with high CONUT scores. Therefore, the current study shed light on that the CONUT score might be a useful predictor, not only for long-term outcomes but also for short-term outcomes in GC patients.
The biological mechanism why CONUT could be a predictor for short-term outcomes in GC has not been clearly understood. Here we tried to explain the reasons from each parameter of CONUT. Firstly, serum albumin, representing protein metabolism, is a strong marker of nutritional status. Low serum albumin is not only correlated with poor prognosis in GC but also reported to be a promising predictor for short-term outcomes following gastrectomy [10, 34, 35]. Gunder et al. recently reported that albumin levels were better to predict both short-term and long-term GC patient outcomes than complex parameters (PNI, NLR, PLR, and SII) [36]. Serum albumin level was so significant that it has twice the weight of the other components in the CONUT score. Multivariate analysis revealed that the CONUT rather that albumin level was correlated with postoperative short-term complications. Secondly, total cholesterol level, representing lipid metabolism, has been found to be related to tumor progression and overall survival in various kinds of cancer [37, 38]. Several studies suggested that a low cholesterol level might affect the antioxidant reserve and inflammatory response [39, 40]. Finally, total lymphocyte, representing host immunocompetence, was also reported to be correlated with the prognosis of GC patients [41]. The combination of these three components into CONUT allows different phases of nutrition to be included, which enhances the accuracy to assess general conditions.
We acknowledged some potential limitations in this study. First, it was a retrospective, single-center study. Patients enrolled were from just one institution and were ethnically homogeneous. Second, the potential factors influencing preoperative immune-nutritional status were not accessed, such as cancer-related inflammation, chronic renal failure, and liver cirrhosis. Third, the suitable cutoff value for the CONUT score was not yet unified. Therefore, more studies are warranted for elucidating the predictive ability of CONUT for postoperative complications of GC patients.
Conclusion
In conclusion, the present study demonstrated that the preoperative CONUT was an independent predictor for short-term complications following gastrectomy of GC.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BMI:
-
Body mass index
- CRP:
-
C-reactive protein
- NLR:
-
Neutrophil-to-lymphocyte ratio
- PLR:
-
Platelet-to-lymphocyte ratio
- PNI:
-
Prognostic Nutritional Index
- CONUT:
-
Controlling Nutritional Status
- ASA:
-
American Society of Anesthesiologists
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Ca-a Cancer J Clin. 2018;68(6):394–424.
Kim W, Kim H-H, Han S-U, Kim M-C, Hyung WJ, Ryu SW, Cho GS, Kim CY, Yang H-K, Park DJ, et al. Decreased morbidity of laparoscopic distal gastrectomy compared with open distal gastrectomy for stage I gastric cancer short-term outcomes from a multicenter randomized controlled trial (KLASS-01). Ann Surg. 2016;263(1):28–35.
Lee K-G, Lee H-J, Yang J-Y, Oh S-Y, Bard S, Suh Y-S, Kong S-H, Yang H-K. Risk factors associated with complication following gastrectomy for gastric cancer: retrospective analysis of prospectively collected data based on the Clavien–Dindo system. J Gastrointest Surg. 2014;18(7):1269–77.
Takagi K, Domagala P, Polak WG, Buettner S, Ijzermans JNM. The controlling nutritional status score and postoperative complication risk in gastrointestinal and hepatopancreatobiliary surgical oncology: a systematic review and meta-analysis. Ann Nutr Metab. 2019;74(4):303–12.
Wang S-H, Zhai S-T, Lin H. Role of Prognostic Nutritional Index in patients with gastric cancer: a meta-analysis. Minerva Med. 2016;107(5):322–7.
Wang SC, Chou JF, Strong VE, Brennan MF, Capanu M, Coit DG. Pretreatment neutrophil to lymphocyte ratio independently predicts disease-specific survival in resectable gastroesophageal junction and gastric adenocarcinoma. Ann Surg. 2016;263(2):292–7.
Hsu J-T, Wang C-C, Le P-H, Chen T-H, Kuo C-J, Lin C-J, Chou W-C, Yeh T-S. Lymphocyte-to-monocyte ratios predict gastric cancer surgical outcomes. J Surg Res. 2016;202(2):284–90.
Kubota T, Shoda K, Konishi H, Okamoto K, Otsuji E. Nutrition update in gastric cancer surgery. Ann Gastroenterol Surg. 2020.
Ge X, Dai X, Ding C, Tian H, Yang J, Gong J, Zhu W, Li N, Li J. Early postoperative decrease of serum albumin predicts surgical outcome in patients undergoing colorectal resection. Dis Colon Rectum. 2017;60(3):326–34.
Liu Z-J, Ge X-L, Ai S-C, Wang H-K, Sun F, Chen L, Guan W-X. Postoperative decrease of serum albumin predicts short-term complications in patients undergoing gastric cancer resection. World J Gastroenterol. 2017;23(27):4978–85.
Luo Z, Zhou L, Balde AI, Li Z, He L, ZhenWei C, Zou Z, Huang S, Han S, Zhou MW, et al. Prognostic impact of preoperative prognostic nutritional index in resected advanced gastric cancer: a multicenter propensity score analysis. Ejso. 2019;45(3):425–31.
Zhang X, Chen X, Wu T, Zhang Y, Yan K, Sun X. Modified glasgow prognostic score as a prognostic factor in gastriccancer patients: a systematic review and meta-analysis. Int J Clin Exp Med. 2015;8(9):15222–9.
Ignacio de Ulibarri J, Gonzalez-Madrono A, de Villar NGP, Gonzalez P, Gonzalez B, Mancha A, Rodriguez F, Fernandez G. CONUT: a tool for controlling nutritional status First validation in a hospital population. Nutr Hosp. 2005;20(1):38–45.
Kuroda D, Sawayama H, Kurashige J, Iwatsuki M, Eto T, Tokunaga R, Kitano Y, Yamamura K, Ouchi M, Nakamura K, et al. Controlling Nutritional Status (CONUT) score is a prognostic marker for gastric cancer patients after curative resection. Gastric Cancer. 2018;21(2):204–12.
Takagi K, Buettner S, Ijzermans JNM. Prognostic significance of the controlling nutritional status (CONUT) score in patients with colorectal cancer: a systematic review and meta-analysis. Int J Surg. 2020;78:91–6.
Li W, Li M, Wang T, Ma GZ, Deng YF, Pu D, Liu ZK, Wu Q, Liu XJ, Zhou QH. Controlling Nutritional Status (CONUT) score is a prognostic factor in patients with resected breast cancer. Sci Rep. 2020;10(1):1–10.
Shimose S, Kawaguchi T, Iwamoto H, Tanaka M, Miyazaki K, Ono M, Niizeki T, Shirono T, Okamura S, Nakano M, et al. Controlling Nutritional Status (CONUT) score is associated with overall survival in patients with unresectable hepatocellular carcinoma treated with lenvatinib: a multicenter cohort study. Nutrients. 2020;12(4):1076.
Suzuki H, Ito M, Takemura K, Nakanishi Y, Kataoka M, Sakamoto K, Tobisu KI, Koga F. Prognostic significance of the controlling nutritional status (CONUT) score in advanced urothelial carcinoma patients. Urol Oncol Semin Orig Investig. 2020;38(3):76-e11.
Yoshida N, Baba Y, Shigaki H, Harada K, Iwatsuki M, Kurashige J, Sakamoto Y, Miyamoto Y, Ishimoto T, Kosumi K, et al. Preoperative nutritional assessment by Controlling Nutritional Status (CONUT) is useful to estimate postoperative morbidity after esophagectomy for esophageal cancer. World J Surg. 2016;40(8):1910–7.
Miyata T, Yamashita Y, Higashi T, Taki K, Izumi D, Kosumi K, Tokunaga R, Nakagawa S, Okabe H, Imai K, et al. The prognostic impact of Controlling Nutritional Status (CONUT) in intrahepatic cholangiocarcinoma following curative hepatectomy: a retrospective single institution study. World J Surg. 2018;42(4):1085–91.
Takagi K, Domagala P, Polak WG, Buettner S, Wijnhoven BPL, Ijzermans JNM. Prognostic significance of the controlling nutritional status (CONUT) score in patients undergoing gastrectomy for gastric cancer: a systematic review and meta-analysis. BMC Surg. 2019;19(1):129.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Sun X, Liu X, Liu J, Chen S, Xu D, Li W, Zhan Y, Li Y, Chen Y, Zhou Z. Preoperative neutrophil-to-lymphocyte ratio plus platelet-to-lymphocyte ratio in predicting survival for patients with stage I–II gastric cancer. Chin J Cancer. 2016;35:1–7.
Nozoe T, Ninomiya M, Maeda T, Matsukuma A, Nakashima H, Ezaki T. Prognostic nutritional Index: A tool to predict the biological aggressiveness of gastric carcinoma. Surg Today. 2010;40(5):440–3.
Elghiaty A, Kim J, Jang WS, Park JS, Heo JE, Rha KH, Choi YD, Ham WS. Preoperative controlling nutritional status (CONUT) score as a novel immune-nutritional predictor of survival in non-metastatic clear cell renal cell carcinoma of 7cm on preoperative imaging. J Cancer Res Clin Oncol. 2019;145(4):957–65.
Ohba T, Takamori S, Toyozawa R, Nosaki K, Umeyama Y, Haratake N, Miura N, Yamaguchi M, Taguchi K, Seto T, et al. Prognostic impact of the Controlling Nutritional Status score in patients with non-small cell lung cancer treated with pembrolizumab. J Thorac Dis. 2019;11(9):3757–68.
Wang XB, Chen J, Xiang BD, Wu FX, Li LQ. High CONUT score predicts poor survival and postoperative HBV reactivation in HBV-related hepatocellular carcinoma patients with low HBV-DNA levels. Ejso. 2019;45(5):782–7.
Hirahara N, Tajima Y, Fujii Y, Kaji S, Kawabata Y, Hyakudomi R, Yamamoto T, Taniura T. Controlling Nutritional Status (CONUT) as a prognostic immunonutritional biomarker for gastric cancer after curative gastrectomy: a propensity score-matched analysis. Surg Endosc. 2019;33(12):4143–52.
Ahiko Y, Shida D, Horie T, Tanabe T, Takamizawa Y, Sakamoto R, Moritani K, Tsukamoto S, Kanemitsu Y. Controlling nutritional status (CONUT) score as a preoperative risk assessment index for older patients with colorectal cancer. BMC Cancer. 2019;19(1):1–8.
Liu X, Zhang D, Lin E, Chen Y, Li W, Chen Y, Sun X, Zhou Z. Preoperative controlling nutritional status (CONUT) score as a predictor of long-term outcome after curative resection followed by adjuvant chemotherapy in stage II–III gastric Cancer. BMC Cancer. 2018;18(1):699.
Ryo S, Kanda M, Ito S, Mochizuki Y, Teramoto H, Ishigure K, Murai T, Asada T, Ishiyama A, Matsushita H, et al. The Controlling Nutritional Status score serves as a predictor of short- and long-term outcomes for patients with stage 2 or 3 gastric cancer: analysis of a multi-institutional data set. Ann Surg Oncol. 2019;26(2):456–64.
Suzuki S, Kanaji S, Yamamoto M, Oshikiri T, Nakamura T, Kakeji Y. Controlling Nutritional Status (CONUT) score predicts outcomes of curative resection for gastric cancer in the elderly. World J Surg. 2019;43(4):1076–84.
Lin J-X, Lin L-Z, Tang Y-H, Wang J-B, Lu J, Chen Q-Y, Cao L-L, Lin M, Tu R-H, Huang C-M, et al. Which nutritional scoring system is more suitable for evaluating the short- or long-term prognosis of patients with gastric cancer who underwent radical gastrectomy? J Gastrointest Surg. 2020;24(9):1969–77.
Toiyama Y, Yasuda H, Ohi M, Yoshiyama S, Araki T, Tanaka K, Inoue Y, Mohri Y, Kusunoki M. Clinical impact of preoperative albumin to globulin ratio in gastric cancer patients with curative intent. Am J Surg. 2017;213(1):120–6.
Huang Q-X, Ma J, Wang Y-S. Significance of preoperative ischemia-modified albumin in operable and advanced gastric cancer. Cancer Biomark. 2018;22(3):477–85.
Guner A, Kim SY, Yu JE, Min IK, Roh YH, Roh C, Seo WJ, Cho M, Choi S, Choi YY, et al. Parameters for predicting surgical outcomes for gastric cancer patients: simple is better than complex. Ann Surg Oncol. 2018;25(11):3239–47.
Sun HL, Huang XQ, Wang ZM, Zhang GX, Mei YP, Wang YS, Nie ZL, Wang SK. Triglyceride-to-high density lipoprotein cholesterol ratio predicts clinical outcomes in patients with gastric cancer. Journal of Cancer. 2019;10(27):6829–36.
Li B, Huang DL, Zheng HL, Cai Q, Guo ZL, Wang SS. Preoperative serum total cholesterol is a predictor of prognosis in patients with renal cell carcinoma: a meta- analysis of observational studies. Int Braz J Urol. 2020;46(2):158–68.
Wang Q, Lau WY, Zhang B, Zhang Z, Huang Z, Luo H, Chen X. Preoperative total cholesterol predicts postoperative outcomes after partial hepatectomy in patients with chronic hepatitis B- or C-related hepatocellular carcinoma. Surgery. 2014;155(2):263–70.
Oh TK, Kim HH, Park DJ, Ahn SH, Do SH, Hwang JW, Kim JH, Oh AY, Jeon YT, Song IA. Association of preoperative serum total cholesterol level with postoperative pain outcomes after laparoscopic surgery for gastric cancer. Pain Pract. 2018;18(6):729–35.
Perez JID, Fernandez G, Salvanes FR, Lopez AMD. Nutritional screening; control of clinical undernutrition with analytical parameters. Nutr Hosp. 2014;29(4):797–811.
Acknowledgements
The authors gratefully acknowledge all of the investigators for their contributions to the trial.
Funding
This work was supported by the Natural Science Foundation of Jiangsu Province (BK20200052).
Author information
Authors and Affiliations
Contributions
FS and CZ worked on the study design, collected data, and drafted the manuscript. ZL helped data collection and extraction. SA contributed to data collection. WG and SL were responsible for study design and manuscript revision. All authors have read and approved the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of Nanjing Drum Tower Hospital, Medial School of Nanjing University. Due to the retrospective nature, the requirement for informed consent was waived by the IRBs from Nanjing Drum Tower Hospital, Medial School of Nanjing University. All the experiment protocol for involving human data was in accordance to guidelines of Nanjing Drum Tower Hospital, Medial School of Nanjing University.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Definition of CONUT.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sun, F., Zhang, C., Liu, Z. et al. Controlling Nutritional Status (CONUT) score as a predictive marker for short-term complications following gastrectomy of gastric cancer: a retrospective study. BMC Gastroenterol 21, 107 (2021). https://doi.org/10.1186/s12876-021-01682-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-021-01682-z