Abstract
Background
This study aimed to establish nomogram models of overall survival (OS) and cancer-specific survival (CSS) in elderly colorectal cancer (ECRC) patients (Age ≥ 70).
Methods
The clinical variables of patients confirmed as ECRC between 2004 and 2016 were retrieved from the Surveillance, Epidemiology, and End Results (SEER) database. Univariate and multivariate analysis were performed, followed by the construction of nomograms in OS and CSS.
Results
A total of 44,761 cases were finally included in this study. Both C-index and calibration plots indicated noticeable performance of newly established nomograms. Moreover, nomograms also showed higher outcomes of decision curve analysis (DCA) and the area under the curve (AUC) compared to American Joint Committee on Cancer (AJCC) tumor-node-metastasis (TNM) stage and SEER stage.
Conclusions
This study established nomograms of elderly colorectal cancer patients with distinct clinical values compared to AJCC TNM and SEER stages regarding both OS and CSS.
Similar content being viewed by others
Background
Colorectal cancer has been ranked as the second most common malignancy in women and third in men across the world. Annual global incidence is approximately 1.4 million with nearly 700,000 deaths [1, 2]. There are more than 50,000 death reports and over 130,000 newly occurred cases in the United States [2]. In European Union, 215,000 cases have been reported with colorectal cancer being listed as the second common cause of death [3]. In China, colorectal cancer is listed as one of the five most commonly malignancies both in men and women [4].
Genomic characterization of colorectal cancer has been well elucidated and the role of immunology is increasingly valued [5,6,7]. Therapeutically, surgical intervention and chemotherapy-based strategies have been widely accepted for colorectal cancer [8, 9]. Noteworthy, the impact of colorectal cancer surgery on the elder group, regarding long term survival, is similar to that of younger group [10].
Generally, elderly colorectal cancer patients (ECRC), defined by age surpass 70 years old, may naturally associate with increased mortality as age increased. However, no study did fully cover nor depict the quantified association of age and risks for prognosis of ECRC [11, 12]. Previously, tumor-node-metastasis (TNM) stage system of American Joint Committee on Cancer (AJCC) is widely used in the therapeutic and prognostic administration of colorectal cancer. Given increasing values of multiple variables, including tumor size and marital status, have been noticed [13, 14], a more comprehensive prognostic predictor is necessary for ECRC.
Of note, knowledge regarding the clinical prediction of ECRC is limited, with very few studies focusing on the nomogram implementation. In this study, a ECRC-targeting nomogram was established for prognostic prediction based on large sample size retrieved from the Surveillance, Epidemiology, and End Results (SEER) database in hopes of elucidating further prognostic insights [15].
Methods
Recruitment of patients from SEER database
The clinical variables of patients confirmed as ECRC between 2004 and 2016 were retrieved from the SEER database, a program established by National Cancer Institute aiming for comprehensively national-level clinical investigation [16, 17]. The reference number was 16,595-Nov2018. The inclusion criteria were: 1) colon and rectum (site recode, international classification of diseases for oncology (ICD-O-3)/WHO 2009); 2) age ≥ 70; 3) complete information on TNM stage; 4) only one primary tumor cases were selected; 5) surgery performed in each case. Next, all included cases were randomly divided into training and validation sets with equal sample size. In addition, x-tile software was used to determine and visualize the best cutoff points of age and tumor size variables in this study [18].
Clinical variables extracted for analysis
Age, sex, marital status, tumor site, histological grade, SEER stage, the AJCC TNM stage, distant metastasis (bone, brain, liver and lung) and tumor size were all selected for the establishment of nomogram modeling. Regarding the clinical outcome, overall survival (OS) and cancer-specific survival (CSS) were chosen as the primary and second endpoints.
Construction and validation of the nomogram
Statistically, chi-square test was used for all included categories between training and validation groups. Next, univariate and multivariate analysis were used to determine distinct variables, which were further output for the construction of nomogram model by R software 3.3.0 (R Foundation for Statistical Computing, Vienna, Austria, www.r-project.org). Then, the validation group was used for the assessment of the newly established nomogram. The comparison between the nomogram prediction and observed outcomes was assessed by the concordance index (C-index). The calibration plot was used for visualized comparison between prognosis predicted by nomogram and actual ones. Sensitivity and specificity were evaluated by receiver operating characteristics curve (ROC)-the area under the curve (AUC). Furthermore, the power of nomogram model was also compared to the TNM stage and SEER stage in both ROC and decision curve analysis (DCA). All analysis was achieved by R software 3.3.0, with p value< 0.05 considered as statistically significant.
Results
Characterization of included cases
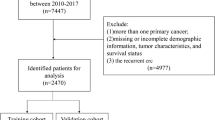
Following inclusion criteria, a total of 44,761 cases were finally included in this study with 22,381 assigned to training set and 22,380 to validation set randomly (Fig. 1). Among all patients, 44.6% were male and 55.4% female; 47.6% were unmarried and 46.8% married; 81.9% were colon cancer and 18.1% rectal cancer; 0.3% of cases had bone metastasis, 0.1% with brain metastasis, 7.0% with liver metastasis, 1.8% with lung metastasis. The cutoff points of age and tumor size were determined by x-tile (Fig. 2). Specifically, 40.9% were < =76 years old, 44.5% between 77 and 86 years old, and 14.7% > =87 years old. 29.8% were < =3.4 cm, 36.3% between 3.5–5.9 cm and 25.4% > = 6 cm (Table 1). No significant difference was identified between training and validation cohorts regarding each included variable.
The X-tile analysis of best-cutoff points of age and tumor size variables. a X-tile plot of training sets in age; b the cutoff point was highlighted using a histogram of the entire cohort; c the distinct prognosis determined by the cutoff point was shown using a Kaplan-Meier plot (low subset = blue, middle subset = gray, high subset = magenta); d X-tile plot of training sets in tumor size; e the cutoff point was highlighted using a histogram; f Kaplan-Meier plot of prognosis determined by the cutoff point (low subset = blue, middle subset = gray, high subset = magenta)
Establishment of the nomogram
Interestingly, sex, age, marital status, tumor size, grade, SEER stage, AJCC TNM stage, bone metastasis, brain metastasis, liver metastasis, lung metastasis and tumor size were all displayed high statistically difference in univariate OS analysis (Table 2). Next, sex, age, marital status, grade, AJCC TNM, bone metastasis, brain metastasis, liver metastasis and lung metastasis and tumor size were all significantly identified in OS multivariate analysis (Table 2). Meanwhile in CSS, age, marital status, tumor site, grade, SEER stage, AJCC TNM stage, bone metastasis, brain metastasis, liver metastasis, lung metastasis and tumor size were significantly identified in univariate CSS analysis. Age, marital status, tumor site, grade, SEER stage, AJCC TNM, bone metastasis, brain metastasis, liver metastasis, lung metastasis and tumor size were significantly associated with CSS in multivariate analysis (Table 3). Thus, OS and CSS nomogram models of 1-, 3- and 5-year were established, respectively (Fig. 3a, b).
Nomogram validation
The assessment was performed both internally and externally, measured by C-index and calibration plots. Specifically, C-index of OS nomogram was 0.726 (95% confidence interval (95%CI): 0.720–0.732) in training set while 0.722 (95%CI: 0.716–0.728) in validation set (Table 4. C-index of CSS was 0.791 (95%CI: 0.785–0.797) in training set while 0.789 (95%CI: 0.783–0.795) (Table 4). Meanwhile, calibration plots indicated high quality of predicted outcome of OS/CSS nomogram models (Figs. 4, 5). Next, to further compare the nomograms with other classic staging methods, including AJCC TNM stage and SEER stage, DCA and ROC were performed in both OS and CSS. In DCA, nomograms both in OS and CSS showed superior power to AJCC TNM stage and SEER stage (Fig. 6). Meanwhile, nomograms in OS and CSS also showed higher statistic power to AJCC TNM stage and SEER stage (Figs. 7, 8, Table 5).
Calibration plots of OS nomogram model. a 1-year calibration plot of OS using training set; b 3-year calibration plot of OS using training set; c 5-year calibration plot of OS using training set; d 1-year calibration plot of OS using validation set; e 3-year calibration plot of OS using validation set; f 5-year calibration plot of OS using validation set
Calibration plots of CSS nomogram model. a 1-year calibration plot of CSS using training set; b 3-year calibration plot of CSS using training set; c 5-year calibration plot of CSS using training set; d 1-year calibration plot of CSS using validation set; e 3-year calibration plot of CSS using validation set; f 5-year calibration plot of CSS using validation set
Receiver operating characteristics curve (ROC) comparison of OS nomogram, AJCC TNM stage and SEER stage. a1-year ROC of OS nomogram using train set; b 3-year ROC of OS nomogram using training set; c 5-year ROC of OS nomogram using training set; d 1-year ROC of OS nomogram using validation set; e 3-year ROC of OS nomogram using validation set; f 5-year ROC of OS nomogram using validation set
ROC comparison of CSS nomogram, AJCC TNM stage and SEER stage. a 1-year ROC of CSS nomogram using train set; b 3-year ROC of CSS nomogram using training set; c 5-year ROC of CSS nomogram using training set; d 1-year ROC of CSS nomogram using validation set; e 3-year ROC of CSS nomogram using validation set; f 5-year ROC of CSS nomogram using validation set
Discussion
Up to now, numerous studies had investigated the role of prognostic nomograms for colorectal cancer patients using SEER database for variable objects [19, 20]. In fact, increasing studies tended to focus more on the therapeutics or modified classification, with very rare highlighted the role of age in the prognostic assessment of colorectal cancer. Our previous study reported that a nomogram for early-onset colorectal cancer patients could display comparably higher C-index value and better performance than conventional variables [21]. ECRC, on the other hand, had been explored with limited studies. Li et al. reported that, with 18,937 included cases, adjuvant chemotherapy did not offer additional survival benefits to elderly patients with stage II or III [22]. Nonetheless, a general prognostic nomogram of ECRC is yet to be fully characterized. In this study, the nomograms displayed higher C-index and convinced calibration plots for OS and CSS prediction using SEER database. Moreover, they achieved higher values regarding both AUC and DCA assessment systems compared to AJCC TNM and SEER stages.
Of note, in OS, 12 variables (sex, age, marital status, grade, AJCC TNM, bone metastasis, brain metastasis, liver metastasis and lung metastasis and tumor size) out of 15 variables were determined for the construction of nomogram. Similar feature had also been noticed in CSS nomogram. It was highly possible that the prognosis of ECRC could be associated with more variables than common colorectal cancer cases. Moreover, four types of distant metastasis, for the first time, had been incorporated for nomogram of ECRC in SEER analysis.
In addition, X-tile tool was introduced for the best cutoff values of age and tumor size in this study. X-tile tool was established as a powerful graphic method to illustrate potential subsets (cutoff) with construction of a two dimensional projection [18]. It had been widely used in numerous investigations, including esophageal squamous cell carcinoma, bladder cancer and chondrosarcoma [23,24,25]. In this study, for the first time, subsets of consecutive variables, age and tumor size, were determined by X-tile tool. In fact, the role of tumor size had been intensively studied [26]. However, the cutoff points of tumor size in colorectal cancer remain largely arbitrary. Therefore, introduction of X-tile for the classification of tumor size could be both reliable and replicated.
Generally, elderly patients may naturally associate with increased mortality as age increased. However, no study did fully cover nor depict the quantified association of age and risks for prognosis, particularly when elderly patients had surpassed 70 years old. In our study, age itself was identified as a higher risk factor in OS compared to CSS nomogram, with age ≥ 87 representing nearly 90 points in OS but less than 60 points in CSS. Interestingly, female was identified as a protective factor in OS nomogram, instead of CSS nomogram. Moreover, marriage is also identified as a protective factor in both OS and CSS nomogram. By comparing OS and CSS nomograms, insightful clues had been noticed for further external clinical investigation.
Conclusion
This study established nomograms of elderly colorectal cancer patients with distinct clinical values compared to AJCC TNM and SEER stages regarding both OS and CSS.
Availability of data and materials
The data that support the findings of this study are available from SEER database but restrictions apply to the availability of these data, which were used under license for the current study (ID: 16595-Nov2018), and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of SEER database.
Abbreviations
- HR:
-
Hazard ratio
- 95%CI:
-
95% confidence intervals
- OS:
-
Overall survival
- CSS:
-
Cancer-specific survival
- ECRC:
-
Elderly colorectal cancer
- SEER:
-
Surveillance, Epidemiology, and End Results database
- TNM:
-
Tumor-Node-Metastasis stage
- AJCC:
-
American Joint Committee on Cancer
- C-index:
-
Concordance index
- ROC:
-
Receiver operating characteristics curve
- DCA:
-
Decision curve analysis
- AUC:
-
Area under receiver operating characteristics curve
References
Arnold M, Sierra MS, Laversanne M, et al. Global patterns and trends in colorectal cancer incidence and mortality [J]. Gut. 2017;66(4):683–91.
Siegel RL, Miller KD, Fedewa SA, et al. Colorectal cancer statistics, 2017. CA Cancer J Clin. 2017;67(3):177–93.
Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JW, Comber H, Forman D, Bray F. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer. 2013;49(6):1374–403.
Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–32.
Network CGA. Comprehensive molecular characterization of human colon and rectal cancer. Nature. 2012;487(7407):330.
De Roock W, De Vriendt V, Normanno N, et al. KRAS, BRAF, PIK3CA, and PTEN mutations: implications for targeted therapies in metastatic colorectal cancer [J]. Lancet Oncol. 2011;12(6):594–603.
Lazarus J, Oneka MD, Barua S, et al. Mathematical modeling of the metastatic colorectal cancer microenvironment defines the importance of cytotoxic lymphocyte infiltration and presence of PD-L1 on antigen presenting cells [J]. Ann Surg Oncol. 2019;26(9):2821–30.
Edge SB, Compton CC. The American joint committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17(6):1471–4.
Benson AB, Venook AP, Cederquist L, Chan E, Chen YJ, Cooper HS, Deming D, Engstrom PF, Enzinger PC, Fichera A, Grem JL. Colon cancer, version 1. 2017, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2017;15(3):370–98.
Devon KM, Vergara-Fernandez O, Victor JC, et al. Colorectal cancer surgery in elderly patients: presentation, treatment, and outcomes [J]. Dis Colon Rectum. 2009;52(7):1272–7.
Kennedy AS, Ball DS, Cohen SJ, et al. Safety and efficacy of radioembolization in elderly (≥ 70 years) and younger patients with unresectable liver-dominant colorectal cancer [J]. Clin Colorectal Cancer. 2016;15(2):141–151. e6.
Feliu J, Salud A, Escudero P, et al. XELOX (capecitabine plus oxaliplatin) as first-line treatment for elderly patients over 70 years of age with advanced colorectal cancer [J]. Br J Cancer. 2006;94(7):969–75.
Suzuki C, Blomqvist L, Sundin A, et al. The initial change in tumor size predicts response and survival in patients with metastatic colorectal cancer treated with combination chemotherapy [J]. Ann Oncol. 2012;23(4):948–54.
Li Q, Gan L, Liang L, et al. The influence of marital status on stage at diagnosis and survival of patients with colorectal cancer [J]. Oncotarget. 2015;6(9):7339.
Hayat MJ, Howlader N, Reichman ME, et al. Cancer statistics, trends, and multiple primary cancer analyses from the Surveillance, Epidemiology, and End Results (SEER) Program [J]. Oncologist. 2007;12(1).
Hankey BF, Ries LA, Edwards BK. The surveillance, epidemiology, and end results program: a national resource. Cancer Epidemiol Prev Biomarkers. 1999;8(12):1117–21.
Hayat MJ, Howlader N, Reichman ME, Edwards BK. Cancer statistics, trends, and multiple primary cancer analyses from the surveillance, epidemiology, and end results (SEER) program. Oncologist. 2007;12(1):20–37.
Camp RL, Dolled-Filhart M, Rimm DL. X-tile: a new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin Cancer Res. 2004;10(21):7252–9.
Kong X, Li J, Cai Y, et al. A modified TNM staging system for non-metastatic colorectal cancer based on nomogram analysis of SEER database [J]. BMC Cancer. 2018;18(1):50.
Zhang Z, Luo Q, Yin X, et al. Nomograms to predict survival after colorectal cancer resection without preoperative therapy [J]. BMC Cancer. 2016;16(1):658.
Yu C, Zhang Y. Development and validation of a prognostic nomogram for early-onset colon cancer [J]. Biosci Rep. 2019;39(6).
Li D, Zhong C, Tang X, et al. Competing nomograms help in the selection of elderly patients with colon cancer for adjuvant chemotherapy [J]. J Cancer Res Clin Oncol. 2018;144(5):909–23.
Tan Z, Zhang M, Han Q, et al. A novel blood tool of cancer prognosis in esophageal squamous cell carcinoma: the fibrinogen/albumin ratio [J]. J Cancer. 2017;8(6):1025.
Zhou H, Tang K, Xiao H, et al. A panel of eight-miRNA signature as a potential biomarker for predicting survival in bladder cancer [J]. J Exp Clin Cancer Res. 2015;34(1):53.
Song K, Shi X, Wang H, et al. Can a nomogram help to predict the overall and cancer-specific survival of patients with chondrosarcoma?[J]. Clin Orthop Relat Res. 2018;476(5):987.
Kornprat P, Pollheimer MJ, Lindtner RA, et al. Value of tumor size as a prognostic variable in colorectal cancer: a critical reappraisal [J]. Am J Clin Oncol. 2011;34(1):43–9.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
ZY and CY carried out data analysis. ZY and CY drafted the manuscript; ZY and CY participated in study design and data collection. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable. This article does not contain any studies with human participants or animals performed by any of the authors.
Consent for publication
Not applicable.
Competing interests
All authors declare no conflict of interest in this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yu, C., Zhang, Y. Establishment of prognostic nomogram for elderly colorectal cancer patients: a SEER database analysis. BMC Gastroenterol 20, 347 (2020). https://doi.org/10.1186/s12876-020-01464-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-020-01464-z