Abstract
Background
Hepatic angiosarcoma is a rare malignant tumor featured by highly aggressive behavior and poor prognosis. There are few reports about diffused hepatic angiosarcoma with Kasabach-Merritt syndrome till now.
Case presentation
A male patient with the chief complain of hepatic space-occupying lesion accompanied by disturbance of consciousness and jaundice. Hyperbilirubinemia, anemia, thrombocytopenia, prolonged prothrombin time, hypofibrinogenemia, decreased prothrombin activity, and increased fibrinogen degradation product and D-dimer were confirmed by blood analysis; multiple focal hypodense lesions in liver was detected by abdominal computed tomography. Liver failure and Kasabach-Merritt syndrome induced by hepatic hemangioma was diagnosed before operation and liver transplantation was performed. Hepatic angiosarcoma was finally proven by postoperative pathology. This patient died of tumor metastasis 2 months after operation.
Conclusions
Hepatic angiosarcoma which can generate Kasabach-Merritt syndrome and even liver failure has an extremely poor prognosis; liver transplantation option should not be considered in hepatic angiosarcoma regardless of the reason.
Similar content being viewed by others
Background
Hepatic angiosarcoma which is characterized by highly aggressive behavior and rapid progression is a rare tumor that originates from endothelial cells in the liver [1]. It accounts for approximately 0.1–2% of all primary liver malignancies [2]. In adults, diffuse hepatic angiosarcoma is few and far between. Although it was first reported in 1974, there is a paucity of data regarding the diagnosis, treatment and prognosis of this malignancy [3].
Kasabach-Merritt syndrome (KMS), reported by Kasabach and Merritt firstly in 1940, is a rare but potentially life-threatening condition. This syndrome presents as hemolytic anemia, thrombocytopenia, prolonged prothrombin time and hypofibrinogenemia and most often occurs in infants [4]. There have been few reports about KMS induced by diffuse hepatic angiosarcoma till now. Liver failure, induced by pharmacological toxicity and viral hepatitis most frequently, is rarely caused by primary liver tumors or liver metastasis [5]. In this report, a patient who was diagnosed with KMS and liver failure at admission received liver transplantation. Hepatic angiosarcoma was confirmed by pathology postoperatively.
Case presentation
This study was approved by the Institutional Review Board of Beijing Chaoyang Hospital. A 56-year-old male patient was admitted to our hospital with the chief complaint of disturbance of consciousness and jaundice on Oct. 12, 2018. According to his family’s description, the symptoms of asthenia, epigastric discomfort, nausea and vomiting were generated 2 weeks ago, jaundice of skin and sclera was exhibited about 1 week before referring to local hospital. The patient received laboratory test and CT (Computed Tomography) scan in local hospital. Liver failure induced by hepatic space-occupying lesions was considered, and symptomatic treatment was provided for this patient. Unfortunately, the symptoms got worse during the treatment period, and disturbance of consciousness was developed about 1 week before admitting to our hospital. Further examinations including blood test and multiphase contrast-enhanced CT were conducted when the patient was referred to our center.
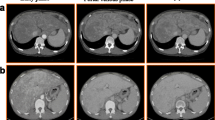
Abnormal laboratory results were as follows: total bilirubin, 449.9 μmol/L (5.0–21.0 μmol/L); direct bilirubin, 280.7 μmol/L (0–6.8 μmol/L); aspartate transaminase, 78 U/L (15-40 U/L); alanine transaminase, 27 U/L (9-50 U/L); ammonia, 204 μmol/L (18-72 μmol/L); albumin, 32.1 g/L (40-55 g/L); white blood cell, 7.28 × 109/L (4.0–10.0 × 109/L); hemoglobin, 67 g/L (120-160 g/L); platelet, 21 × 109 /L (125–350 × 109/L); prothrombin time, 28.3 s (9.6–13.0 s); prothrombin activity, 35.2% (80.0–120.0%); fibrinogen, 81.6 mg/dl (170.0–400.0 mg/dl); fibrinogen degradation product, 74.7 μg/ml (0-5 μg/ml); INR (International Normalized Ratio), 2.19 (0.8–1.2); D-dimer, 25.13 (< 0.55 mg/L FEU); α-fetoprotein, 1.1 ng/mL (< 8.1 ng/mL); carcinoembryonic antigen, 1.0 ng/mL (0–5.0 ng/mL); Carbohydrate Atigen, 19–9 65.5 (0–37 U/mL). Abdominal CT exhibited that the liver was diffusely enlarged and the surface was irregular, multiple focal hypodense liver lesions were distributed diffusely throughout the liver parenchyma (Fig. 1). The patient was diagnosed with liver failure and hepatic hemangioma with KMS based on these results.
Liver transplantation was performed for this patient. Liver came from donation after circulatory death (DCD). Technique of modified piggyback orthotopic liver transplantation was conducted. The enlarged liver could be seen during the operation (Fig. 2). There were no enlarged lymph nodes were detected in the hepatic portal area and hepatoduodenal ligament. Findings including atypical vessels and spindle-shaped cells exhibiting nuclear atypicality were observed under the microscope. Immunohistochemistry demonstrated the positive expression of endothelial cell markers including CD31, CD34 and factor VIII, and the negative expression of CK, CK8/18, CK19, Glypican 3, CD 21 and CD 68, the Ki-67 proliferative index was 30%. Hepatic angiosarcoma was finally confirmed. The patient died of tumor metastasis 2 months after operation.
Discussion and conclusions
Diffused hepatic angiosarcoma is an extremely rare malignant tumor characterized by aggressive proliferation and wide distribution of tumor cells. Despite the low incidence of hepatic angiosarcoma, it is the most common primarily malignant mesenchymal tumor of the liver in adults. It accounts for 2% of all primary hepatic malignancies [1, 6, 7]. The pathogenesis of hepatic angiosarcoma is still uncertain, exposure to polyvinyl chloride and arsenic can lead to a high incidence of hepatic angiosarcoma [8].
KMS, also known as Kasabach-Merritt phenomenon (KMP), is frequently found in children with kaposiform haemangioendothelioma or tufted angioma. A study designed by Ji Y confirmed that approximately 70% of patients diagnosed with kaposiform haemangioendothelioma showed KMP, lesions involving the trunk were more likely to have KMP than non-trunk lesions, and they found that age at discovery of the tumor lesion, morphology and tumor size were independent risk factors for KMP [9]. KMP is considered as a rare complication of vascular tumors [10]. Liver failure which is frequently caused by pharmacological toxicity and viral hepatitis is seldom induced by primary liver tumors including hepatic angiosarcoma.
Despite the hypothesis that KMP is exclusively limited to these two vascular formations in paediatric populations [11], there have been several case reports about hepatic angiosarcoma with KMS in adults recently [12]. KMS is characterized by anemia, thrombocytopenia, prolonged prothrombin time, hypofibrinogenemia, and obviously increased fibrinogen degradation product and D-dimer. Based on the blood test results, the patient was diagnosed with KMS.
Liver hemangioma was diagnosed mistakenly before operation due to the insufficiency of typical imaging features for angiosarcoma. Diagnostic indicators are difficult to obtain for distinguishing angiosarcoma from hemangioma. Some studies suggested that there were several imaging features on contrast-enhanced CT: hepatic angiosarcoma should be highly suspected if non-peripheral enhancement and arteriovenous short circuit were observed; while the radiological features of hepatic hemangioma was characterized by peripheral nodular enhancement, arteriovenous short circuit was scarce [3, 13, 14]. Unfortunately, it was difficult to get the correct diagnosis by observing patient’s imaging before operation.
Radical resection followed by targeted therapy is the most effective treatment strategy for hepatic angiosarcoma [15]. Less than 20% of patients were suitable for radical hepatectomy due to its aggressive behavior and multifocal distribution [1]. Liver transplantation is not recommended since no advantages for survival in those patients who received transplantation incidentally or with therapeutic intentions [16]. Median survival after liver transplantation is less than 7 months according to European Liver Transplant Registry [16]. Liver transplantation was conducted for this patient on account of liver failure and incorrect diagnosis. Standard adjuvant chemotherapy regimens have not been established for the disease till now.
Because of highly aggressive behavior, low radical resection rate and insensitivity to chemoradiotherapy, hepatic angiosarcoma has a very high relapse rate and short survival time. The vast majority of patients have a mean survival time of less than 6 months if no treatment is provided [6, 15]. Even if treatment is conducted, only 3% of patients have the survival time of more than 2 years [17]. Groeschl et al. [18] reported that the median overall survival time of patients with hepatic angiosarcoma was only 1 month, and survival time can be prolonged to 6 months if patients received radical resection. Patient died of lung and brain metastasis 2 month after liver transplantation in this report.
In conclusion, hepatic angiosarcoma is a rare malignant tumor with very poor prognosis, it can result in KMS and liver failure. Radical resection followed by targeted therapy may be the most effective treatment strategy. Liver transplantation should not be considered in hepatic angiosarcoma regardless of the reason.
Availability of data and materials
The datasets used and/or analyzed in the current study are available from the corresponding author on reasonable request.
Abbreviations
- CT:
-
Computed Tomography
- DCD:
-
Donation after circulatory death
- INR:
-
International Normalized Ratio
- KMP:
-
Kasabach-Merritt phenomenon
- KMS:
-
Kasabach-Merritt syndrome
References
Chaudhary P, Bhadana U, Singh RA, Ahuja A. Primary hepatic angiosarcoma. Eur J Surg Oncol. 2015;41:1137–43.
Pickhardt PJ, Kitchin D, Lubner MG, Ganeshan DM, Bhalla S, Covey AM. Primary hepatic angiosarcoma: multi-institutional comprehensive cancer Centre review of multiphasic CT and MR imaging in 35 patients. Eur Radiol. 2015;25:315–22.
Zhu YP, Chen YM, Matro E, Chen RB, Jiang ZN, Mou YP, et al. Primary hepatic angiosarcoma: a report of two cases and literature review. World J Gastroenterol. 2015;21:6088–96.
Hall GW. Kasabach-Merritt syndrome: pathogenesis and management. Br J Haematol. 2001;112:851–62.
Schilsky ML, Honiden S, Arnott L, Emre S. ICU management of acute liver failure. Clin Chest Med. 2009;30:71–87 viii.
Molina E, Hernandez A. Clinical manifestations of primary hepatic angiosarcoma. Dig Dis Sci. 2003;48:677–82.
Wang ZB, Yuan J, Chen W, Wei LX. Transcription factor ERG is a specific and sensitive diagnostic marker for hepatic angiosarcoma. World J Gastroenterol. 2014;20:3672–9.
Bolt HM. Vinyl chloride-a classical industrial toxicant of new interest. Crit Rev Toxicol. 2005;35:307–23.
Ji Y, Yang K, Peng S, Chen S, Xiang B, Xu Z, et al. Kaposiform haemangioendothelioma: clinical features, complications and risk factors for Kasabach-Merritt phenomenon. Br J Dermatol. 2018;179:457–63.
Habringer S, Boekstegers A, Weiss L, Hopfinger G, Meissnitzer T, Melchardt T, et al. Kasabach-Merritt phenomenon in hepatic angiosarcoma. Br J Haematol. 2014;167:716–8.
Enjolras O, Wassef M, Mazoyer E, Frieden IJ, Rieu PN, Drouet L, et al. Infants with Kasabach-Merritt syndrome do not have “true” hemangiomas. J Pediatr. 1997;130:631–40.
Wadhwa S, Kim TH, Lin L, Kanel G, Saito T. Hepatic angiosarcoma with clinical and histological features of Kasabach-Merritt syndrome. World J Gastroenterol. 2017;23:2443–7.
Lin J, Bigge J, Ulbright TM, Montgomery E. Anastomosing hemangioma of the liver and gastrointestinal tract: an unusual variant histologically mimicking angiosarcoma. Am J Surg Pathol. 2013;37:1761–5.
Wu CH, Chiu NC, Yeh YC, Kuo Y, Yu SS, Weng CY, et al. Uncommon liver tumors: case report and literature review. Medicine (Baltimore). 2016;95:e4952.
Zheng YW, Zhang XW, Zhang JL, Hui ZZ, Du WJ, Li RM, et al. Primary hepatic angiosarcoma and potential treatment options. J Gastroenterol Hepatol. 2014;29:906–11.
Orlando G, Adam R, Mirza D, Soderdahl G, Porte RJ, Paul A, et al. Hepatic hemangiosarcoma: an absolute contraindication to liver transplantation--the European liver transplant registry experience. Transplantation. 2013;95:872–7.
Locker GY, Doroshow JH, Zwelling LA, Chabner BA. The clinical features of hepatic angiosarcoma: a report of four cases and a review of the English literature. Medicine (Baltimore). 1979;58:48–64.
Groeschl RT, Miura JT, Oshima K, Gamblin TC, Turaga KK. Does histology predict outcome for malignant vascular tumors of the liver? J Surg Oncol. 2014;109:483–6.
Acknowledgements
All authors thank Li Shen-ming and Liu Rong-jun for supporting data, their supports are the key factor for completion of this manuscript.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
ZXM and HQ reviewed the literature, drafted and edited the manuscript; LQ and TY aided in acquisition and interpretation of the data; TY gave advice on the work; ZXM and HQ conceived the study, and participated in its design and in data acquisition. All authors were involved in the patient’ active management. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was reviewed and approved by the Ethics Committee of Beijing Chaoyang Hospital. Consent to participate was not required in this case report, as all procedures described were parts of normal treatment protocol and were presented here retrospectively.
Consent for publication
Written informed consent was obtained from the patient for publication of the case report and accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, Xm., Tong, Y., Li, Q. et al. Diffused hepatic angiosarcoma with Kasabach-Merritt syndrome-case report and literature review. BMC Gastroenterol 20, 80 (2020). https://doi.org/10.1186/s12876-020-01216-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-020-01216-z