Abstract
Background
The efficacy of some therapeutic methods (open surgical debridement (OSD), conservative treatment (CST) and minimally invasive drainage (MID)) for severe acute pancreatitis (SAP) and moderately severe acute pancreatitis (MSAP) has been widely evaluated. However, the results remained controversial. We performed this study to illuminate whether any difference in incidence exists on patients with SAP/MSAP treated with OSD and MID.
Methods
Eligible articles were collected base of a comprehensive review of PUBMED, EMBASE, COCHRANE, CKNI and WANGFANG for published randomized controlled trials. Two steps of meta-analysis were performed, routine pair-wise meta-analysis and network meta-analysis.
Results
Thirteen studies were included in this study. Participants were classed as 5 groups, CST, early MID (EMID), late MID (LMID), early OSD (EOSD) and late OSD (LOSD). And MID contains endoscopic drainage (ESD), percutaneous catheter drainage (PCD) and minimally invasive surgery (MIS). Compared with CST, MID could decrease both mortality and multiple organ dysfunction syndrome (MODS) rate but OSD couldn’t. Both EMID and MID can significantly decrease the mortality and MODS rate compared to CST. PCD might be most likely to have a benefit compared to CST.
Conclusion
Existing evidence for the use of MID in SAP/MSAP is reliable and it can be used as early treatment. OSD, if necessary, should be avoided or delayed as long as possible.
Similar content being viewed by others
Introduction
Acute pancreatitis (AP) is one of the most common digestive system diseases requiring acute hospitalization worldwide [1]. In Atlanta Criteria revision of 2012 [2], AP was classified based on severity as mild, moderately severe, or severe. Most patients have mild acute pancreatitis and recover without intervention [3,4,5]. Moderately severe acute pancreatitis (MSAP), which is characterized by local complications in the absence of persistent organ failure, while severe acute pancreatitis (SAP) is defined as persistent single or multiorgan failure (lasting> 48 h) and is present in around 20% of patients, with a mortality rate of 10 to 40% [6, 7]. SAP is a sudden occurrence and an irreversible condition. It usually contains two phases. Early or toxic enzymatic phases in first 2 weeks and later on septic phase after third to fourth week onwards. It occurs with about 20–30% in clinic practices and mortality rate of up to 10–35%. Intervention is generally required for patients with SAP. Timely and effective drainage of abdominal cavity effusion, removal of necrotic tissue and infection control can obviously improve prognosis of SAP include the rate of multiple organ dysfunction syndrome (MODS), complications and death, even the hospitalization time [8]. It is one of the most challenging medical conditions in acute abdomen surgery [9]. In a prospective study, Buchler et al. suggested that patients with infected necrosis remain a high-risk group of SAP, and recommended surgical treatment [10]. Although the open surgical debridement (OSD) was the traditional treatment, it has been associated with high complications and mortality of patients [11, 12]. Many studies have been showed that minimally invasive drainage (MID) may be successfully and safely applied to treat SAP [13]. There is a lack of large-scale randomized clinical trials in this field to compare the effect of MID and OSD [14]. The PANTER trial was the first time to show the feasibility and success of the step-up approach in comparison with open necrosectomy in a randomized controlled manner in the management of SAP [15]. However, it is still bothering us that subset of patients treated by the step-up approach would require laparotomy. Moreover, the timing of surgery is difficult to choose, which remains a problem that needs to be addressed. Therefore, in this review, we mainly aimed to conduct a random-effects routine pairwise meta-analysis and network meta-analysis comparing the safety and efficacy of MID and OSD.
Methods
IRB approval and informed consent
This study is a meta-analysis of randomized controlled trials and the IRB approval and informed consent is unnecessary.
Types of participants
Patients with SAP/MSAP undergoing treatment of CST, MID or OSD were included.
Types of interventions
We included trials comparing MID (Minimally invasive drainage is small incision surgery and video-assisted surgery. It contains ESD, PCD and MIS), OSD (Open surgical debridement consisted of a laparotomy through an abdominal or retroperitoneal route incision. After removal of all necrotic tissue, drains for postoperative lavage were inserted. And then, the abdomen was closed) and CST (Conservative treatment is an intensive care treatment, which consists of drug therapy (including spasmolysis, analgesia, protease inhibitors), circulatory volume maintenance to prevent electrolyte imbalances, oxygen supplementation, nutritional supplementation, mechanical ventilation). ESD is defined that ERCP is given and nasal biliary drainage or stenting of the pancreatic duct and stone removal were performed under endoscope as appropriate. PCD is a technique that ultrasound-guided percutaneous drainage tube placement. MIS usually means a surgery performed by laparoscope, which make a small incision in the abdomen. Patients whose intervention were started as MID and later converted to OSD belong in MID group. We excluded trials that did not use the above definition. For the operation time, we define that treatments do immediately or early reflected in the studies as early, and those treated late or timing not clear in these studies were categorized as late.
Types of studies
We only included randomized clinical trials irrespective of blinding or publication status. No language restrictions were used.
Types of outcome measure
-
1.
Primary outcomes: Mortality.
-
2.
Secondary outcomes: MODS Rate. MODS is thepresence of altered organ function which cannot bemaintained without intervention. It usually involves twoor more organ systems.
Procedures
We searched the electronic databases up to Aug 2017. We used to search terms included “negative pressure wound therapy”, “negative pressure wound therapies”, “drain”, “drains”, “drainage”, “severe pancreatitis”, “severe acute pancreatitis”, “severe necrotized pancreatitis”, “moderately severe pancreatitis”, “moderately severe acute pancreatitis”, “moderately AND severe necrotizing pancreatitis”, “random allocation”, “random”, “randomly”, “randomized”, “longitudinal studies”. These terms were combined using “AND” and “OR”. References from the acquired articles were also hand-searched. Studies, which were RCT studies for treatment of SAP/MSAP, were included if they met the following criteria: they addressed any types of interventions above and were published in the years 2000–2017. Studies were excluded if they contained any of the following: they were not in English or Chinese, not peer reviewed, and if the main focus did not relate to interventions in SAP/MSAP above. Our search strategy, selection criteria and data extraction were completed independently by two reviewers (Kai Zhang and Xiaole Zhu). We assessed risk of bias in contributing studies with standard criteria [14].
Study design
We did a network meta-analysis using a Bayesian model. Network meta-analysis can integrate all the data from direct comparisons of treatments within trials and from indirect comparisons of interventions assessed against a common comparator in different trials, to compare all investigated treatments.
Statistical analysis
Analysis was performed using RevMan 5.3 (freeware from The Cochrane Collaboration) and R-3.4.2 software. The gemtc packages (version 0.8) were used to conduct a Bayesian analysis that combined data from multiple randomized control trials. We assessed the risk of bias of studies in accordance with the Cochrane Handbook for Systematic Reviews of Interventions using RevMan 5.3. The figure of risk of bias summary was showed as Fig. 1. Network meta-analyses are better at integrating different types of evidence compared with conventional pairwise meta-analyses, however this type of analysis leads to inevitable heterogeneity. We did two steps of meta-analysis. First, we did routine pairwise meta-analysis with a random-effects model [17] and I2 metric was used to assess the heterogeneity in these analyses [16]. Second, we did random-effects network meta-analysis [18] and the I2 metric and meta-regression were also used to assume a common heterogeneity variable for these comparisons by meta packages (version 4.9–6). We did routine random-effects pair-wise and network meta-analyses to estimate at primary and secondary outcomes, and we presented the estimates as risk ratios (dichotomous outcomes) with 95% CIs and Crls [19]. The Node-splitting analysis method was used to assess the inconsistency between direct and indirect comparisons when a loop connecting three arms existed. Transitivity is a feature of Network meta-analysis. CST was used as a link to know the relationship between MID and PSD better [20]. Participants who fulfilled our inclusion criteria could be allocated to one of the treatments being compared. Transitivity proceeds if all direct comparisons between treatments respecting to the distribution of effect modifiers (for example, studies comparing MID with CST were similar to studies comparing OSD with CST in terms of the level of mortality).
Result
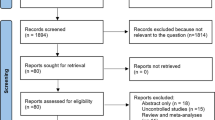
Finally, thirteen studies with a total of 985 participants were included, which provided enough data for the analyses of mortality conducted in this study. In all of the studies, ten studies were from China while three were from Holland or Finland. Six studies were published in English and the rest were published in Chinese (Table 1). Twelve studies with data for 931 participants were available for the comparison between OSD, MID and CST. Thirteen studies including 985 adults were eligible for the network meta-analysis of different timing for OSD and MID. Six studies with 675 participants were available for the network meta-analysis of different types of MID. The PRISMA flowchart [18] showing electronic searching processes is shown in the Fig. 2. Participants were classed as 5 groups, CST, early MID, MID, early PSD and PSD. And MID contains ESD, PCD and MIS and the comparison between each other was shown in Fig. 3.
Network of all these comparisons. a and b for Comparison 1, c and d for Comparison 2 and e and f for Comparison 3. The circle stands for one type of therapy, such as MID, CST and OSD. The thickness of lines stand for the number of studies between the two circles (types of therapy) and thicker line means more studies
Comparison 1-MID VS. OSD
All these twelve studies contain the data onto mortality (113/931) and six studies for MODS rate (65/406). Comparison of mortality (34/453 in MID and 29/136 in OSD with 50/342 in CST) and MODS rate (15/196 in MID and 33/91 in OSD with 17/119 in CST) of the patients showed that MID could significantly decrease the mortality (pair−wise RR: 0.50, 95%CI 0.21–0.81, I2 = 19.9% and network RR: 0.36, 95%CrI 0.16–0.64, I2 = 24.1%) but not MODS rate (Fig. 4, Table 2).
Comparison 2-EMID VS. LMID VS. EOSD VS. LOSD VS. CST
Thirteen studies were taken in this part. Data for direct comparisons and network estimates for both mortality and for MODS rate of SAP/MSAP treated with various ways are shown in the Table 2. We ranked the comparative effects of all treatment against CST. Overall, both early MID and MID can significantly decrease the mortality (RR: 0.43, 95%CrI 0.21–0.78, I2 = 0.0% and RR: 0.19, 95%CrI 0.06–0.47, I2 = 66.2%) and MODS rate compared to CST (RR: 0.43, 95%CrI 0.20–0.76, I2 = 0.0% and RR: 0.18, 95%CrI 0.06–0.46, I2 was incalculable), but early PSD or PSD can’t in network estimates (Fig. 5).
Comparison 3-ESD VS. PCD VS. MIS VS. CST
The above result showed the positive effect of MID SAP/MSAP treatment. Then, we proceeded the direct comparisons and network estimates to estimate the mortality and MODS rate of SAP/MSAP treated with various types of MID. Only one direct comparison showed that MIS could significantly decrease the mortality (RR: 0.48, 95%CI 0.24–0.93, I2 = 0.0%). The networks of eligible comparisons showed that ESD, PCD and MIS can decrease the mortality but not statistically significant (Fig. 6).
Discussion
This meta-analysis based on thirteen comparative studies of MID (ESD, PCD, and MIS), OSD and CST, enrolling 931 patients with SAP/MSAP. The results of 453 patients in the MID group, 136 patients in the OSD group and 342 patients in CST group documents the feasibility and potential benefits of MID. No matter early MID and MID could decrease the mortality and MODS rate comparing to CST. Moreover, MID in the later period may be better. OSD had no influence on overall morbidity and MODS rate compared to CST. Several Studies got the same conclusion and suggested that one or more types of MID should be prefered [21].
MID contained several types, such as ESD, PCD and MIS. Despite high popularity of minimally invasive surgery in other surgical disciplines, MID has still not become the gold standard in the treatment for SAP/MSAP [22, 23]. While performing this meta-analysis, we found few randomized controlled trials on this topic, but the sample size is not large enough. As we know, there are several previously published meta-analysis comparing the MID with open approach [24,25,26]. However, in most of them, there is a methodological bias due to the fact that they were including not only RCT but also some retrospective study in their analysis studies. Therefore, in our analysis, we included only studies reporting as RCT, thus, limiting bias associated with uncertain data.
The mainstream principle of interventions in SAP/MSAP now is that no single approach is appropriate for all patients. The best approach which is adaptable to the individual patient is multimodal. Integrated management of these patients by specialists is essential to achieve a better outcome. The step-up approach involves percutaneous or endoscopic transmural drainage for sepsis control followed by minimally invasive or open necrosectomy as indicated and was recommended in some guidelines [27, 28]. A multi-center RCT showed the result that patients with (suspected) infected necrosis treated with a step-up approach of PCD, followed, if needed, by minimally invasive necrosectomy could be superior to those treated with primary open necrosectomy [15]. Another multicenter RCT designed by the same team suggested that endoscopic transluminal necrosectomy may decrease the risk compared to surgical necrosectomy in some terms, such as new onset multiple organ failure and overall complications [21]. In another study by Sunil Shenvi et al., a randomized controlled trial was designed to establish the benefits of group A (step-up approach as a bridge to surgery) or group B (step-up approach with intention to avoid surgery). The trial was stopped after the first 8 patients randomized into two groups because of difficulty in accrual and poor progress [8].
In this meta-analysis, SAP/MSAP treated with MID would get better prognosis than those treated with CST or OSD. And early MID may achieve better effect than late. But, in this study, there are some aspects which should be improved. The first and the most important limitation is that it is not an interventional study in which improvement could be made. Secondly, the articles included in these studies contain more Chinese ones than English (seven Chinese articles and six English articles). And even in some English articles, the first authors and data were from China. Fortunately, the conclusion of the studies both from Chinese or English articles are the same (Additional file 1: Figure S1 and Additional file 2: Figure S2) and the results of meta-regression suggested language was not statistically significant in the mortality comparison of CST and MID, and CST and EMID (Additional file 3: Table S1). The results showed that MID would get better prognosis. Thirdly, it was hard to identify what is early and what is late. We could only define that treatments do immediately or early reflected in the studies as early. And those treated late or timing not clear in the studies were categorize as late. After that, the timing effect would be weakened. All these above factors can affect the credibility of our meta-analysis.
Conclusions
The existing evidence of this study shows that the use of MID in SAP/MSAP is reliable and it could be used as early treatment. OSD, if necessary, should be avoided or delayed as long as possible.
Availability of data and materials
All data in our study are available from the corresponding authors upon reasonable request.
Abbreviations
- AP:
-
Acute pancreatitis
- CST:
-
Conservative treatment
- EMID:
-
Early minimally invasive drainage
- EOSD:
-
Early open surgical debridement
- ESD:
-
Endoscopic drainage
- LMID:
-
Late minimally invasive drainage
- LOSD:
-
Late open surgical debridement
- MID:
-
Minimally invasive drainage
- MIS:
-
Minimally invasive surgery
- MODS:
-
Multiple organ dysfunction syndrome
- MSAP:
-
Moderately severe acute pancreatitis
- OSD:
-
Open surgical debridement
- PCD:
-
Percutaneous catheter drainage
- RCT:
-
Randomized controlled trial
- RR:
-
Risk ratio
- SAP:
-
Severe acute pancreatitis
References
Yadav D, Lowenfels AB. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology. 2013;144:1252–61.
Feldman M, Friedman LS, Brandt LJ, et al. Sleisenger and Fordtran’s gastrointestinal and liver disease: pathophysiology, diagnosis, management. 10th ed. Philadelphia: Saunders/Elsevier; 2015.
Bradley EL III. A clinically based classification system for acute pancreatitis. Summary of the international symposium on acute pancreatitis, Atlanta, Ga, September 11 through 13, 1992. Arch Surg. 1993;128:586–90.
Working Party of the British Society of Gastroenterology, Association of Surgeons of Great Britain and Ireland, Pancreatic Society of Great Britain and Ireland, Association of Upper GI Surgeons of Great Britain and Ireland. UK guidelines for the management of acute pancreatitis. Gut. 2005;54:iii1–9.
Toouli J, Brooke-Smith M, Bassi C, et al. Guidelines for the management of acute pancreatitis. J Gastroenterol Hepatol. 2002;17:15–39.
Uhl W, Warshaw A, Imrie C, et al. IAP guidelines for the surgical management of acute pancreatitis. Pancreatology. 2002;2:565–73.
Werner J, Feuerbach S, Uhl W, et al. Management of acute pancreatitis: from surgery to interventional intensive care. Gut. 2005;54:426–36.
Shenvi S, Gupta R, Kang M. Timing of surgical intervention in patients of infected necrotizing pancreatitis not responding to percutaneous catheter drainage. Pancreatology. 2016;16(5):778–87.
Hu H-k, Du X-j, Li A, Ke N-w, Hu W-m. A minimally invasive management for abdominal compartment syndrome in severe acute pancreatitis. Pak J Med Sci. 2013;29:231–3.
Büchler MW, Gloor B, Müller CA, et al. Acute necrotizing pancreatitis: treatment strategy according to the status of infection. Ann Surg. 2000;232(5):619–26.
Nieuwenhuijs VB, Besselink MG, van Minnen LP, et al. Surgical management of acute necrotizing pancreatitis: a 13-year experience and a systematic review. Scand J Gastroenterol Suppl. 2003;239:111–6.
Rau B, Bothe A, Beger HG. Surgical treatment of necrotizing pancreatitis by necrosectomy and closed lavage: changing patient characteristics and outcome in a 19-year, single-center series. Surgery. 2005;138:28–39.
Gagner M, Pomp A. Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc. 1994;8:408–10.
Song KB, Kim SC, Hwang DW, et al. Matched case-control analysis comparing laparoscopic and open pylorus-preserving pancreaticoduodenectomy in patients with periampullary tumors. Ann Surg. 2015;262:146–55.
Van Santvoort HC, Besselink MG, Bakker OJ, Hofker HS, Boermeester MA, Dejong CH, et al. A step-up approach or open necrosectomy for necrotizing pancreatitis. N Engl J Med. 2010;362:1491e502.
Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions, version 5.1.0. March, 2011. http://www.cochrane-handbook.org (Accessed 9 Apr 2015).
DerSimonian R, Laird N. Meta-analysis in clinical trials. Clin Trials. 1986;7:177–88.
Salanti G. Indirect and mixed-treatment comparison, network, or multiple-treatments meta-analysis: many names, many benefits, many concerns for the next generation evidence synthesis tool. Res Synth Methods. 2012;3:80–97.
Turner RM, Davey J, Clarke MJ, Thompson SG, Higgins JP. Predicting the extent of heterogeneity in meta-analysis, using empirical data from the Cochrane database of systematic. Int J Epidemiol. 2012;41(3):818–27.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700 reviews. Int J Epidemiol. 2012;41:818–27.
Bakker OJ, van Santvoort HC, van Brunschot S, et al. Dutch Pancreatitis Study Group Endoscopic transgastric vs surgical necrosectomy for infected necrotizing pancreatitis: a randomized trial. JAMA. 2012;307:1053–61.
de Rooij T, Klompmaker S, Abu Hilal M, et al. Laparoscopic pancreatic surgery for benign and malignant disease. Nat Rev Gastroenterol Hepatol. 2016;13:227–38.
Coppola A, Stauffer JA, Asbun HJ. Laparoscopic pancreatoduodenectomy: current status and future directions. Updat Surg. 2016;68:217–24.
Zhang H, Wu X, Zhu F, et al. Systematic review and metaanalysis of minimally invasive versus open approach for pancreaticoduodenectomy. Surg Endosc. 2016;30:5173–84.
Wang M, Cai H, Meng L, et al. Minimally invasive pancreaticoduodenectomy: a comprehensive review. Int J Surg. 2016;35:139–46.
Qin H, Qiu J, Zhao Y, et al. Does minimally-invasive pancreaticoduodenectomy have advantages over its open method? A meta-analysis of retrospective studies. PLoS One. 2014;9:e104274.
Working Group IAP/APA Acute Pancreatitis Guidelines. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 2013;13(4 a 2):e1–15.
Tenner S, Baillie J, DeWitt J, et al. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013;108(9):1400–16.
Ai X, Qian X, Pan W, et al. Ultrasound-guided percutaneous drainage may decrease the mortality of severe acute pancreatitis. J Gastroenterol. 2010;45(1):77.
Chen X-Q, Wu J, Liu X-C, et al. Clinical contrast study of endoscopic treatment for acute biliary pancreatitis. World Chin J Digestol. 2007;15(3):298–301.
Lin F. Clinical control study of early endoscopic therapy for severe gallstone pancreatitis. Chin J Gastroenterol Hepatol. 2016;25(8):903–5.
Liu H, Chen K, Xiang G'a, et al. Laparoscopy combined with endoscopic and digital subtraction angiography for treatment of severe acute pancreatitis. J South Med Univ. 2009;29(8):1620–2.
Liu L, Yan H, Liu W, et al. Abdominal paracentesis drainage does not increase infection in severe acute pancreatitis: A prospective study [J]. J Clin Gastroenterol. 2015;49(9):757.
Schröder T, Sainio V, Kivisaari L, et al. Pancreatic resection versus peritoneal lavage in acute necrotizing pancreatitis. Ann Surg. 1991;214(6):663–6.
Wang G, Liu H, Xu L, et al. Effect of laparoscopic peritoneal lavage and drainage and continuous Venovenous Diahemofiltration on severe acute pancreatitis. J Laparoendosc Adv Surg Tech A. 2017;27(11):1145–50.
Zhang H, Liu L, Sun L, et al. Efficacy of continuous peritoneal lavage for severe acute pancreatitis:a prospective randomized controlled study of 104 cases. Chin J Pancreatol. 2007;7(6):353–6.
Zhang J, Yang Z'A, Li X, et al. Therapeutic effects of percutaneous catheter drainage for treatment of severe acute pancreatitis complocated with peripancreatic fluid collections. Chongqing Med. 2011;40(35):3543–4.
Wang Z, He Y, He C. The application of laparoscopic lavage drainage in early treatment of severe acute pancreatitis. J Guangxi Med Univ. 2006;23(6):981–2.
Zhong Y, Cui N. The comparison of efficacy between early non-surgical treatment and early endoscopic treatment in biliary severe acute pancreatitis. Chin J Surg Integ Tradit West Med. 2013;4:361–4.
Acknowledgements
Not applicable.
Funding
This work was supported by grants from the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD, JX10231801), The Innovation Capability Development Project of Jiangsu Province (No. BM2015004) and Jiangsu Biobank of Clinical Resources (BM2015004).
Author information
Authors and Affiliations
Contributions
QL, YM, CQH, CYS, XLZ and KZ all have made substantial contributions to conception, acquisition of data, analysis, and interpretation of data. All of them have been involved in drafting the manuscript and revising it critically for important intellectual content. All authors read and approved the final manuscript and take public responsibility for appropriate portions of the content and agreed to be accountable for all aspects of work.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study is a meta-analysis of randomized controlled trials and the IRB approval and informed consent is unnecessary.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Figure S1. Forest plot of Mortality for CST, MID and OSD in Chinese Articles. (JPG 27 kb)
Additional file 2:
Figure S2. Forest plot of Mortality for CST, MID and OSD in English Articles. (JPG 27 kb)
Additional file 3:
Table S1. The assessment of heterogeneity by meta-regression. (DOCX 11 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zhang, K., Zhu, X., Hou, C. et al. Minimally invasive drainage versus open surgical debridement in SAP/SMAP – a network meta-analysis. BMC Gastroenterol 19, 168 (2019). https://doi.org/10.1186/s12876-019-1078-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-019-1078-x