Abstract
Background
Capecitabine plus bevacizumab (CAP-B) maintenance treatment after 6 cycles of capecitabine, oxaliplatin, and bevacizumab (CAPOXB) has demonstrated clinical activity and failure to compromise quality of life in patients with metastatic colorectal cancer (MCC) in a previous phase 3 CAIRO3 study. The objective of this study is to evaluate the efficacy and safety of CAP-B versus CAP in maintenance treatment after 6-cycle CAPOXB induction therapy in Chinese postmenopausal women with untreated characterised KRAS exon 2 wild-type MCC.
Methods
During 2012–2016, prospectively maintained databases were reviewed to evaluate cohorts with untreated characterised KRAS exon 2 wild-type MCC and stable disease or better after 6-cycle CAPOXB induction treatment. After induction treatment, all patients received either CAP-B or capecitabine (CAP) as maintenance treatment. Median progression-free survival (mPFS) and median overall survival (mOS) were the primary endpoints. Safety was the secondary endpoint.
Results
A total of 263 women with untreated characterised KRAS exon 2 wild-type MCC and stable disease or better after 6-cycle CAPOXB induction treatment were included for the evaluation of efficacy and safety (CAP-B-treated cohort, n = 130 and CAP-treated cohort, n = 133). The mPFS was 11.5 months (95% confidence interval [CI], 5.6–17.4) and 9.2 months (95% CI, 3.6–14.8) for the CAP-B-treated and CAP-treated cohorts, respectively (HR 0.54, 95% CI 0.32~0.85; P = 0.013). The mOS was 16.2 months (95% CI, 11.4–18.7) and 12.4 months (95% CI, 10.6–15.5) for the CAP-B- and CAP-treated cohorts, respectively (HR 0.72, 95% CI 0.51~0.94; P = 0.022). The CAP-B-treated cohort experienced significantly more grade 3 or 4 diarrhoea (P < 0.001) than the CAP-treated cohort.
Conclusions
CAP-B maintenance treatment after 6-cycle CAPOX-B in Chinese postmenopausal women with untreated KRAS exon 2 wild-type MCC is poorer tolerated but has a more modest, if any, benefit compared with that of CAP maintenance treatment.
Similar content being viewed by others
Background
The estimated incidence of stage 1–3 colorectal cancer in China for 2017 is 100,000 patients, of which almost 70% did develop metastatic colorectal cancer (MCC), which is partially related to common delays in diagnosis [1,2,3]. Despite the lack of multi-centre, open-label, double-arm trials that compared the efficacy and safety of different therapeutic regimens in patients with MCC, 4 prospective studies comparing the efficacy and safety of bevacizumab(B) and capecitabine (CAP) had indicated a safe and effective regimen for the treatment of patients with late-stage colorectal cancer [3,4,5,6]. However, evidence from recent studies suggests that MCC carrying extended KRAS exon 2 mutations predicted for the lack of activity of anti-epidermal growth factor receptor (EGFR) therapies and resulted in restriction to the use of anti-EGFR monoclonal antibodies, making these drugs suitable for the so-called “super” wild-type patients only [7,8,9]. Approximately 70% patients with KRAS exon 2 wild-type(wt) MCC tend to have a poor prognosis, with a median overall survival (mOS) of 4–8 months and a median progression-free survival (mPFS) of 3–9 months [10,11,12].
KRAS exon 2 wt MCC has historically demonstrated restricted response to intervention, and prospective trials with small samples have presented poor outcomes [10, 11]. Despite recent developments in targeted therapies, experience with these agents in KRAS exon 2 wt MCC is still inadequate [12]. Previous retrospective studies have either excluded or lacked definite details of the inclusion of KRAS exon 2 wt MCC [13, 14]. At the time of study development, bevacizumab, a recombinant humanised monoclonal immunoglobulin G antibody, was considered a favourable antiangiogenic agent and was approved by the US Food and Drug Administration(UFDA) for the first-line treatment of KRAS exon 2 wt MCC [15]. The combination regimen of bevacizumab and CAP in MCC has been reviewed extensively [16]. In previous retrospective studies, the addition of bevacizumab was observed to significantly improve the patient’s mPFS and mOS, with 5–7 months and 5–18 months for bevacizumab in comparison to 3–6 months and 4–12 months for placebo, respectively [17]. The results of a prior phase 3 CAIRO3 trial demonstrated that MCC patients with stable disease or better after 6-cycle induction treatment with capecitabine, oxaliplatin, and bevazicumab (CAPOXB) had a significant benefit from CAP-B maintenance treatment compared to observation [18]. Although the trial was not premeditated to detect a difference in mOS between groups, an absolute mOS benefit of 3.5 months was detected, which was not statistically significant (HR0.89, 95% CI 0.73–1.07). In addition, in the phase 3 CAIRO3 trial, the analysis of this type of patients with untreated characterised KRAS exon 2 wt MCC is disregarded. A multi-center, single-arm, phase II trial (CCOG-0801) has been conducted to investigate targeted therapy alone, where either bevacizumab was unavailable or the toxicity profile of bevacizumab had been considered adverse [19]. Their study included 47 patients from 2008 to 2010 with untreated characterised KRAS exon 2 wt MCC, and patients underwent 6-cycle CAPOXB induction therapy, followed by CAP-B or CAP maintenance treatment. The CAP maintenance treatment group described 2-year clinical outcomes that were encouraging, with mPFS of 54% and mOS of 63%. Nevertheless, with a median follow-up of 30 months, adverse events had occurred in 9 (19.1%) cases, which raises questions about whether CAP maintenance treatment was acceptable in the absence of bevacizumab, regardless of the cost-effectiveness of CAP-B. Furthermore, hormone-based therapy, a potential MCC preventive intervention, may influence carcinogenesis through cellular pathways involving the KRAS oncogene in postmenopausal women. Nevertheless, most existing literature tend to ignore hormones as an interference factor, which is likely to lead to a weakening of the power to draw conclusions.
The purpose of this study was to compare the safety and efficacy of CAP and CAP-B as maintenance treatment after 6-cycle-CAPOXB induction treatment for Chinese postmenopausal women with untreated characterised KRAS exon 2 wt MCC even after progression with these drugs during the treatment.
Methods
Study design and patient eligibility
A retrospective study was conducted on Chinese postmenopausal women with untreated characterised KRAS exon 2 wt MCC at 3 tertiary medical institutions from January 2012 to December 2016. MCC was defined by the International Classification of Disease Clinical Modification 10th edition ICD-10 code (C.18–C.20). For these patients, the analysis results of EGFR next-generation sequencing of the RAS/BRAF/PI3KCA genes were available. The study cohort included 412 patients diagnosed with untreated characterised KRAS exon 2 wt MCC. Diagnosis of metastasis was based on contrast-enhanced computed tomography (CT), contrast-enhanced magnetic resonance imaging (MRI), or positron emission tomography–computed tomography (PET-CT) scan, and these patients had received initial 6-cycle CAPOXB induction therapy, followed by either capecitabine plus bevacizumab (CAP-B) or capecitabine (CAP) maintenance treatment. Inclusion criteria: patients age range 60–80 years, with histologically proven metastatic colorectal adenocarcinoma; patients with KRAS exon 2 mutation detected by high-resolution melting analysis; unresectable metastasis; an Eastern Collaborative Oncology Group (ECOG) performance score of 0–2 and a life expectancy of 2 years, excluding their colorectal cancer diagnosis; at least one measurable lesion evaluated according to the Response Evaluation Criteria in Solid Tumours (RECIST) version 1.1 [20] by using either CT, MRI or PET-CT; adequate haematologic, liver, and renal function (neutrophil granulocytes ≥1.5 × 109/L; thrombocytes ≥75 × 109/L; creatinine clearance ≥30 mL/min; total bilirubin concentration ≤ 2 times the upper normal limit; liver transaminase or alkaline phosphatase ≤3 times the upper limit of normal; and concentrations). Exclusion criteria: patients with failure to undergo rigid proctoscopy; another primary cancer within 5 years; non-healed or planned surgery; uncontrollable underlying diseases; brain metastasis; thrombotic episode within 6 months; clinically significant cardiovascular or cerebrovascular diseases; clinical obstruction requiring a temporary diverting ostomy or endorectal stent to maintain bowel patency; modification, discontinuation or interruption of CAP-B or CAP regimen; blood system or liver diseases; previous chemoradiotherapy; uncontrolled diabetes mellitus or hypertension; severe infectious; cognitive dysfunction; mental illness; incomplete medical records; and refusal to participate.
Definitions of the descriptive variables
Patients with untreated characterised KRAS exon 2 wt MCC was defined as that patients with characterised KRAS exon 2 wt MCC had failed to undergo radiotherapy, chemotherapy, or surgical resection of colorectal cancer before 6-cycle CAPOXB induction therapy. PFS was calculated from the onset of maintenance until the date of disease progression or death from any cause. OS was alculated from the onset of maintenance until the date of death for any cause. The tumour cell content of each sample included was assessed on haematoxylin–eosin stained slides by an experienced pathologist. EGFR mutation analysis was performed by using the next-generation sequencing method of the RAS/BRAF/PI3KCA genes, as described [2, 21]. Symptom assessment were performed every 3 months for the entire study period. Metastatic recurrence was confirmed mainly on the basis of imaging data. The rating rules for adverse events was based on Common Terminology Criteria for Adverse Events (NCI-CTCAE) version 4.0. Medical therapy was performed in line with institutional guidelines. Assessment of response or progression was on the basis of either MRI or endorectal ultrasound. Temporary diverting ostomy was mainly based on the general situation of patients.
Study design and treatment
A retrospective, multi-centre study was performed, in which eligible patients received 6-cycle CAPOX-B induction therapy, as described by Nakayama et al. [19]. CAP-B maintenance therapy (intravenous B 7.5 mg/kg once a day and intravenous CAP 1000 mg/m2 twice daily) or CAP maintenance therapy (intravenous CAP 1000 mg/m2 twice daily) was performed for patients with stable or better following 6-cycle CAPOX-B induction therapy. The primary endpoints were mPFS and mOS. The secondary endpoint was safety.
Statistical analysis
The X-square test or Mann–Whitney U-test was used to compare categorical data. Continuous data were expressed as mean ± SD. A two-sample Student’s t test was applied to analyse differences in continuous data. The primary endpoints were compared using the log-rank test and were assessed by the Kaplan-Meier methods to estimate the mean and median with 95% CI. Cox hazard model were executed to assess the effect of CAP-B and CAP on PFS and OS. Statistical programming and analyses were produced using SPSS software, version 24.0 (IBM, Armonk, New York, USA). All statistical tests were two-sided. Differences were considered statistically significant at P < 0.05.
Results
Comparison of baseline data
From January 2012 to December 2016, the cohort comprised 263 postmenopausal women (CAP-B-treated cohort n = 130, mean age 68.6 years [SD 8.43] and CAP-treated cohort n = 133, 69.1 years [SD 8.27]) for study eligibility (Fig. 1). The median follow-up time of all cases included in the study was 15.2 months (range 3.1–39.4 months). The mean duration of the study at the primary analysis cut-off date was 25.2 months (IQR 6.0–42.3) for patients on CAP-B and 24.7 months (IQR 3.4–46.0) for patients on CAP, and the last follow-up time was January 2018. Characteristics of the 263 cases from which all relevant information was available are presented in Tables 1 and 2. No significant difference was detected in baseline data between groups.
Comparison of efficacy
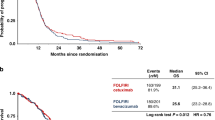
The mPFS, one of the primary endpoints, was 11.5 months (95% CI, 5.6–17.4 months) for the CAP-B-treated group and 9.2 months (95% CI, 3.6–14.8) for the CAP-treated group. The mOS was 16.2 months (95% CI, 11.4–18.7) for the CAP-B-treated cohort and 12.4 months (95% CI, 10.6–15.5) for the CAP-treated cohort, as presented in Table 3. Significant differences in the mPFS (0.54, 95% CI 0.32~0.85; P = 0.013) (Fig. 2) and mOS (0.72, 95% CI 0.51~0.94; P = 0.022) (Fig. 3) were detected between the CAP-treated and CAP-B-treated cohorts, respectively. The 2-group cohorts received no surgical treatment for primary or metastatic lesions.
Kaplan–Meier Curves for progression-free survival. The median progression-free survival was respectively 9.2 months (range, 3.6–14.8 months) in the CAP group; the median progression-free survival was 11.5 months (range, 5.6–17.4 months) in the CAP-B group. Statistically significant difference was detected in the progression-free survival between groups. *Hazard ratio was calculated using a Cox proportional-hazards model, with the type of age, site of primary tumour, number of metastatic sites, and performance status as covariates and CAP/CAP-B therapy as time-dependent factor. With respect to the progression-free survival, results of a log-rank test, P = 0.013
Kaplan–Meier Curves for overall survival. The median overall survival was 16.2 months (range, 9.2–23.2 months) in the CAP-B group; the median overall survival was 12.4 months (range, 5.9–18.9 months) in the CAP group. Significant difference was detected in the overall survival between groups. *Hazard ratio was calculated using a Cox proportional-hazards model, with the type of age, site of primary tumour, number of metastatic sites, and performance status as covariates and CAP/CAP-B therapy as time-dependent factor. With respect to the overall survival, results of a log-rank test, P = 0.022
Adverse events
The incidence of major drug-related adverse events is presented in Table 4. The frequencies of haematological and non-haematological adverse events exceeding grade 3 were 13.8 and 6.9% for the CAP-B- and CAP-treated groups, respectively, for the complete treatment period. Peripheral sensory neuropathy occurred in 36 cases (13.7%), including 8 cases (3.0%) with 3-grade peripheral sensory neuropathy, of which 5 occurred at the end of the 3rd month of the CAP-B therapy and 3 occurred at the end of 4th month of the CAP therapy. The drug-related toxicities observed occurred at a moderately constant rate of cases throughout the overall treatment period; nevertheless, treatment discontinuation occurred in 17 cases (11 [8.5%] for CAP-B and 6 [4.5%] for CAP) that were excluded from the study for myocardial ischaemia, apparently owing to drug-related coronary vasospasm, and 5 cases (3.8%) that failed to complete the maintenance therapy as a result of bevacizumab-related toxicities (2 for 2-grade mucositis and 3 for 3-grade dehydration and 3-grade diarrhoea. Of 263 cases, 29 (11.0%) completing the initial CAPOX-B induction therapy had a requirement of reduction in the CAP-B or CAP dose: 22 (16.9%) required a reduced CAP-B dose, 7 (5.3%) required a reduced CAP dose. Diarrhoea, the most frequent 4-grade toxicity eliminating lymphopenia, occurred in 10.8 and 3%, followed by rash in 13.3 and 6.4%, in the CAP- and CAP-B-treated cohorts, respectively(P = 0.013).
Discussion
The present study followed Chinese postmenopausal women with untreated KRAS exon 2 wt MCC for a mean of 2 years, and the most important finding was that CAP-B is a feasible maintenance treatment for these patients after 6-cycle CAPOX-B induction treatment compared with CAP. The superiority of CAP-B over CAP after 6-cycle CAPOX-B in Chinese postmenopausal women with untreated KRAS exon 2 wt MCC remains a matter of debate, which precludes any recommendations.
In most patients, in daily practice, KRAS mutational status is evaluated in samples originating from primary intestinal lesions at the time of diagnostic colonoscopy [9, 12]. The rationale for the application of anti-EGFR monoclonal antibodies in KRAS exon 2 wt MCC cases depended on the appropriate concordance of mutational status between primary and metastatic tumours, as presented in previous literature [22, 23]. Nevertheless, noteworthy differences in the incidence of KRAS exon 2 mutations among tumour locations have been reviewed [8, 9, 24]. The superiority of CAP-B over CAP remains controversial, which precludes any recommendations [2, 6, 7]. A growing but still very limited body of literature comparing the clinical efficacy of CAP-B and CAP in the management of Chinese postmenopausal women with untreated KRAS exon 2 wt MCC after 6-cycle CAPOX-B induction treatment demonstrated comparable outcomes [10]. Chen et al. [25] noticed a longer mPFS in postmenopausal women receiving CAP-B treatment than those recieving CAP treatment at a mean follow-up of 2 years. Our finding further expounded the significant differences in the mPFS between groups but were inconsistent with several prior retrospective reports that showed no significant differences in the mPFS [14, 22]. Furthermore, a prospective study by Yamaguchi et al.[26]comprising 31 cases with untreated KRAS exon 2 wt MCC receiving CAP-B or CAP treatment after 6-cycle CAPOX-B induction treatment confirmed no significant difference in the mPFS.
As using chemotherapy alone in the current treatment only has a modest, if any, benefit, we wanted to evaluate whether CAP-B or CAP as maintenance treatment after 6-cycle CAPOX-B induction treatment could improve mPFS and/or mOS in untreated KRAS exon 2 wt MCC [27]. Only a few 3 phase II trials comparing CAP-B with CAP in similar regimens showed no improvement in mPFS or mOS [1, 26, 27]. Comparing with prior trials using the identical strategy with bevacizumab, the last study reported by Gervais et al.[18]failed to obtain benefit, although CAP-B, which had been investigated in a small population of 27 cases, had an extraordinary mOS of 2 years.
This study undoubtedly showed that Chinese postmenopausal women with untreated KRAS exon 2 wt MCC managed in the CAP-B or CAP setting have almost indistinguishable 2-year PFS and OS when treated using neoadjuvant chemotherapy first, followed by chemoradiation and then surgery [16]. Moreover, compared to no addition, the addition of bevacizumab produced statistically significant benefit [15]. The CAP-B or CAP maintenance treatment has been espoused by previous investigations [1, 15, 28]. Based on the above facts, CAP-B or CAP has become the wide-reaching favoured approach for those women with untreated KRAS exon 2 wt MCC [1]. The application of CAPOX-B administration rather than other regimens was based predominantly on a US Intergroup study indicating outstanding outcomes with CAP therapy [1, 2]. However, the CAP strategy was observed to be relevant to outcomes inferior to those with the CAP-B strategy in Chinese postmenopausal women with untreated MCC. A previous trial evaluating CAP as a maintenance treatment failed to reach its primary endpoint of increasing the mPFS from 2 to 4 months [18]. Hence, CAP showed no distinct benefit for the cohort. In addition, the end-points, as mentioned above, tended to be inferior to the outcomes from previous meta-analyses with bevacizumab [29, 30]. The current study consequently seemed to support the treatment concept that combining bevacizumab with CAP in maintenance treatment was superior to CAP alone. Nevertheless, comparison of the results from different maintenance treatments was challenging [15]. The attributes of research object were difficult to achieve relative consistency. Thus, the study only demonstrated that combining bevacizumab with CAP in these cases previously treated with 6-cycle CAPOX-B induction treatment tended to result in a benefit.
Despite the small sample of the study and the drawback of the retrospective study, the strength and consistency of the CAP-B treatment results corroborated the findings from previous multi-centre studies [31, 32]. The current therapeutic regimen was clearly different from previous neoadjuvant chemotherapy regimens reported by several Asian researchers [33, 34]. Given the positive mPFS and mOS of our results in the CAP-B setting in untreated KRAS exon 2 wt MCC, we have an optimistic opinion that the positive results were attributable to bevacizumab. However, despite the documented benefits of bevacizumab in the management of MCC, rare adverse reactions have been reported, i.e., thromboembolic events, diarrhea, wound healing abnormalities, irreversible leuco-encephalopathy syndrome [29,30,31]. In addition, maintenance treatment with CAP-B does not appear to be cost-effective [9].
This study should be interpreted in light of important limitations. First, the nature of the retrospective study with all the problems inherent with this methodology limits the level of confidence of our conclusion, and it is possible that every potential confounding variable, such as underlying diseases, failed to be addressed in our analyses. Second, limited sample size may have introduced bias. Nevertheless, the focus of our study is to assess an area that has not been studied extensively in the literature. Third, our analysis has the lack of generalisability because our study population included only postmenopausal women with KRAS exon 2 wild-type MCC. Fourth, every attempt was made to adjust for all potential confounders, but other unmeasured factors may also be relevant.
Conclusions
In summary, the study confirms that CAP-B maintenance treatment after 6-cycle CAPOX-B in Chinese postmenopausal women with untreated KRAS exon 2 wt MCC is poorly tolerated but has a more modest, if any, benefit compared with that of CAP maintenance treatment. Further evidence-based prospective evaluation of the long-term efficacy and safety of CAP or CAP-B in these patients with untreated KRAS exon 2 wt MCC should be expanded using randomised controlled trials.
Abbreviations
- B:
-
Bevacizumab
- CAP:
-
Capecitabine
- CAP-B:
-
Capecitabine plus bevacizumab
- CAPOXB:
-
Capecitabine, oxaliplatin, and bevacizumab
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- ECOG:
-
Eastern collaborative oncology group
- EGFR:
-
Epidermal growth factor receptor
- HR:
-
Hazard ratio
- IQR:
-
Interquartile range
- MCC:
-
Metastatic colorectal cancer
- mOS:
-
Median overall survival
- mPFS:
-
Median progression-free survival
- MRI:
-
Nuclear magnetic resonance imaging
- PET-CT:
-
Positron emission tomography–computed tomography
- RECIST:
-
Response evaluation criteria in solid tumours
- UFDA:
-
US Food and Drug Administration
- wt:
-
Wild-type
References
Li J, Qin SK, Xu RH, Yau TCC, Ma B, Pan HM, et al. Regorafenib plus best supportive care versus placebo plus best supportive care in Asian patients with previously treated metastatic colorectal cancer (CONCUR): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2015;16(6):619–29.
Algars A, Sundstrom J, Lintunen M, Jokilehto T, Kytola S, Kaare M, et al. EGFR gene copy number predicts response to anti-EGFR treatment in RAS wild type and RAS/BRAF/PIK3CA wild type metastatic colorectal cancer. Int J Cancer. 2017;140(4):922–9.
Xu JM, Kim TW, Shen L, Sriuranpong V, Pan HM, Xu RH, et al. Results of a Randomized, Double- Blind, Placebo- Controlled, Phase III Trial of Trifluridine/Tipiracil (TAS-102) Monotherapy in Asian Patients With Previously Treated Metastatic Colorectal Cancer: The TERRA Study. J Clin Oncol. 2018;36(4):350-+.
Alfonso PG, Chaves M, Munoz A, Salud A, Garcia-Giron C, Gravalos C, et al. Phase ii study to evaluate efficacy and safety of irinotecan, CAPECITABINE and bevacizumab in metastatic colorectal cancer (MCRC) patients. Ann Oncol. 2012;23:103–4.
Lang I, Brodowicz T, Ryvo L, Kahan Z, Greil R, Beslija S, et al. Bevacizumab plus paclitaxel versus bevacizumab plus capecitabine as first-line treatment for HER2-negative metastatic breast cancer: interim efficacy results of the randomised, open-label, non-inferiority, phase 3 TURANDOT trial. Lancet Oncol. 2013;14(2):125–33.
Gligorov J, Doval D, Bines J, Alba E, Cortes P, Pierga JY, et al. Maintenance capecitabine and bevacizumab versus bevacizumab alone after initial first-line bevacizumab and docetaxel for patients with HER2-negative metastatic breast cancer (IMELDA): a randomised, open-label, phase 3 trial. Lancet Oncol. 2014;15(12):1351–60.
Allegra CJ, Jessup JM, Somerfield MR, Hamilton SR, Hammond EH, Hayes DF, et al. American Society of Clinical Oncology provisional clinical opinion: testing for KRAS gene mutations in patients with metastatic colorectal carcinoma to predict response to anti-epidermal growth factor receptor monoclonal antibody therapy. J Clin Oncol. 2009;27(12):2091–6.
Kang MJ, Hong YS, Kim KP, Kim SY, Baek JY, Ryu MH, et al. Biweekly cetuximab plus irinotecan as second-line chemotherapy for patients with irinotecan-refractory and KRAS wild-type metastatic colorectal cancer according to epidermal growth factor receptor expression status. Investig New Drugs. 2012;30(4):1607–13.
Konigsberg R, Hulla W, Klimpfinger M, Reiner-Concin A, Steininger T, Buchler W, et al. Clinical and economic aspects of KRAS mutational status as predictor for epidermal growth factor receptor inhibitor therapy in metastatic colorectal Cancer patients. Oncology. 2011;81(5–6):359–64.
Li W, Shi Q, Wang W, Liu J, Ren J, Li Q, et al. KRAS status and resistance to epidermal growth factor receptor tyrosine-kinase inhibitor treatment in patients with metastatic colorectal cancer: a meta-analysis. Color Dis. 2014;16(11):O370–O8.
Riesco-Martinez MC, Berry SR, Ko YJ, Mittmann N, Giotis A, Lien K, et al. Cost-effectiveness analysis of different sequences of the use of epidermal growth factor receptor inhibitors for wild-type KRAS Unresectable metastatic colorectal Cancer. J Oncol Pract. 2016;12(6):574–E723.
Webster J, Kauffman TL, Feigelson HS, Pawloski PA, Onitilo AA, Potosky AL, et al. KRAS testing and epidermal growth factor receptor inhibitor treatment for colorectal Cancer in community settings. Cancer Epidemiol Biomark Prev. 2013;22(1):91–101.
Chen Y, Cao D, Bi F, Li Q, Qiu M. Biweekly cetuximab plus FOLFIRI/irinotecan as first/second-line chemotherapy for patients with KRAS wild-type metastatic colorectal cancer: a retrospective analysis in southwest Chinese population. Med Oncol. 2014;31(5).
Deng YH, Cai Y, Lin JY, Jiang L, Hu HB. Survival of patients with KRAS wild-type metastatic colorectal cancer is identical after sequential treatment with cetuximab and bevacizumab regardless of the sequence - a retrospective single-center study. Gastroenterol Rep. 2015;3(4):339–43.
Cunningham D, Lang I, Marcuello E, Lorusso V, Ocvirk J, Shin DB, et al. Bevacizumab plus capecitabine versus capecitabine alone in elderly patients with previously untreated metastatic colorectal cancer (AVEX): an open-label, randomised phase 3 trial. Lancet Oncol. 2013;14(11):1077–85.
Tebbutt NC, Wilson K, Gebski VJ, Cummins MM, Zannino D, van Hazel GA, et al. Capecitabine, Bevacizumab, and Mitomycin in First-Line Treatment of Metastatic Colorectal Cancer: Results of the Australasian Gastrointestinal Trials Group Randomized Phase III MAX Study. J Clin Oncol. 2010;28(19):3191–8.
Feliu J, Safont MJ, Salud A, Losa F, Garcia-Giron C, Bosch C, et al. Capecitabine and bevacizumab as first-line treatment in elderly patients with metastatic colorectal cancer. Br J Cancer. 2010;102(10):1468–73.
Gervais C, Tournigand C. Maintenance treatment with capecitabine and bevacizumab in metastatic colorectal cancer (CAIRO3): a phase 3 randomised controlled trial of the Dutch colorectal Cancer group. Oncologie. 2015;17(9):405–6.
Nakayama G, Ishigure K, Yokoyama H, Uehara K, Kojima H, Ishiyama A, et al. The efficacy and safety of CapeOX plus bevacizumab therapy followed by capecitabine plus bevacizumab maintenance therapy in patients with metastatic colorectal cancer: a multi-center, single-arm, phase II study (CCOG-0902). BMC Cancer. 2017;17.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47.
Simi L, Pratesi N, Vignoli M, Sestini R, Cianchi F, Valanzano R, et al. High-resolution melting analysis for rapid detection of KRAS, BRAF, and PIK3CA gene mutations in colorectal cancer. Am J Clin Pathol. 2008;130(2):247–53.
Price TJ, Bruhn MA, Lee CK, Hardingham JE, Townsend AR, Mann KP, et al. Correlation of extended RAS and PIK3CA gene mutation status with outcomes from the phase III AGITG MAX STUDY involving capecitabine alone or in combination with bevacizumab plus or minus mitomycin C in advanced colorectal cancer. Br J Cancer. 2015;112(6):963–70.
Rebersek M, Boc M, Cerkovnik P, Benedik J, Hlebanja Z, Volk N, et al. Efficacy of first-line systemic treatment in correlation with BRAF V600E and different KRAS mutations in metastatic colorectal cancer - a single institution retrospective analysis. Radiol Oncol. 2011;45(4):285–91.
Cserepes M, Ostoros G, Lohinai Z, Raso E, Barbai T, Timar J, et al. Subtype-specific KRAS mutations in advanced lung adenocarcinoma: a retrospective study of patients treated with platinum-based chemotherapy. Eur J Cancer. 2014;50(10):1819–28.
Chen HH, Lin JK, Chen JB, Chuang CH, Liu MC, Wang JY, et al. Neoadjuvant therapy of bevacizumab in combination with oxaliplatin and capecitabine (XELOX) for patients with metastatic colorectal cancer with unresectable liver metastases: a phase II, open-label, single-arm, noncomparative trial. Asia Pac J Clin Oncol. 2018;14(1):61–8.
Yamaguchi K, Taniguchi H, Komori A, Narita Y, Nitta S, Nomura M, et al. A single-arm phase II trial of combined chemotherapy with S-1, oral leucovorin, and bevacizumab in heavily pre-treated patients with metastatic colorectal cancer. BMC Cancer. 2015;15.
Naeim A, Ward PR, Wang HJ, Dichmann R, Liem AKD, Chan D, et al. A phase II trial of frontline capecitabine and bevacizumab in poor performance status and/or elderly patients with metastatic colorectal cancer. J Geriatr Oncol. 2013;4(4):302–9
Adamo V, Festa V, Adamo B, Franchina T, Iorfida M, Maugeri SM, et al. Safety of the combination capecitabine plus bevacizumab in the treatment of heavily treated advanced colorectal cancer patients: Our experience. Ann Oncol. 2007;18:VII68–VII9.
Alahmari AK, Almalki ZS, Alahmari AK, Guo JJ. Thromboembolic events associated with bevacizumab plus chemotherapy for patients with colorectal Cancer: a meta-analysis of randomized controlled trials. Am Health Drug Benefits. 2016;9(4):221–31.
Chen XX, Chen YF, Cai XY, Zhang DS, Fan L, Qiu HJ, et al. Efficacy and safety of bevacizumab in elderly patients with advanced colorectal cancer: a meta-analysis. J Cancer Res Ther. 2017;13(5):869–77.
Nakayama G, Uehara K, Ishigure K, Yokoyama H, Ishiyama A, Eguchi T, et al. The efficacy and safety of bevacizumab beyond first progression in patients treated with first-line mFOLFOX6 followed by second-line FOLFIRI in advanced colorectal cancer: a multicenter, single-arm, phase II trial (CCOG-0801). Cancer Chemother Pharmacol. 2012;70(4):575–81.
Simkens LHJ, van Tinteren H, May A, ten Tije AJ, Creemers GJM, Loosveld OJL, et al. Maintenance treatment with capecitabine and bevacizumab in metastatic colorectal cancer (CAIRO3): a phase 3 randomised controlled trial of the Dutch Colorectal Cancer Group. Lancet. 2015;385(9980):1843–52.
Cao RH, Zhang S, Ma DD, Hu LK. A multi-center randomized phase II clinical study of bevacizumab plus irinotecan, 5-fluorouracil, and leucovorin (FOLFIRI) compared with FOLFIRI alone as second-line treatment for Chinese patients with metastatic colorectal cancer. Med Oncol. 2015;32(1).
Sugimachi K, Sakimura S, Kuramitsu S, Hirata H, Niida A, Iguchi T, et al. Serial mutational tracking in surgically resected locally advanced colorectal cancer with neoadjuvant chemotherapy. Br J Cancer. 2018;119(4):419–23.
Acknowledgements
The authors would like to thank Ping Xu for help with retrieval of patients’ notes and radiographs.
Funding
Funding for this research was received from the Shanghai Municipal Health and Family Planning Commission Fund Project (Grant No. 201640057), and the National Natural Science Foundation of China (Grant No. 81770876; 81270011; 81472125). The funding body did not play a role in study design, analysis, interpretation of the data, or the writing of the manuscript.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
JS performed the data collection and analysis and participated in manuscript writing. JL, RY, BX and YZ performed the database setup and statistical analysis. JS, CY, GL and MZ participated in the study design and coordination and helped to draft the manuscript. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki. The histological samples collected were analysed and the clinical data were retrieved with the endorsement of the Institutional Review Boards and Ethical Review Boards of the First Affiliated Hospital, Zhengzhou University; the First Affiliated Hospital, Sun Yat-sen University; Jinshan Hospital, Fudan University. Written informed consent failed to be acquired because the majority of the patients included had died of cancer-related diseases. The informed consent from participants was waived by our Ethical Review Boards.
Consent for publication
Not applicable as no identifying personal information is being published in this manuscript.
Competing interests
All authors have no actual or potential conflict of interest including any financial, personal or other relationships with other people or organizations.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Su, J., Lai, J., Yang, R. et al. Capecitabine plus bevacizumab versus capecitabine in maintenance treatment for untreated characterised KRAS exon 2 wild-type metastatic colorectal cancer: a retrospective analysis in Chinese postmenopausal women. BMC Gastroenterol 19, 17 (2019). https://doi.org/10.1186/s12876-018-0916-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-018-0916-6