Abstract
Background
Acute respiratory tract infections (RTI) in children are a common reason for antibiotic prescribing. Clinicians’ prescribing decisions are influenced by perceived parental expectations for antibiotics, however there is evidence that parents actually prefer to avoid antibiotics. This study aimed to investigate the influence of parent-clinician communication on antibiotic prescribing for RTI in children in England.
Methods
A mixed methods analysis of videoed primary care consultations for children (under 12 years) with acute cough and RTI. Consultations were video-recorded in six general practices in southern England, selected for socio-economic diversity. 56 recordings were transcribed in detail and a subset of recordings and transcripts used to develop a comprehensive interaction-based coding scheme. The scheme was used to examine communication practices between parents and clinicians and how these related to antibiotic or non-antibiotic treatment strategies.
Results
Parents’ communication rarely implied an expectation for antibiotics, some explicitly offering a possible viral diagnosis. Clinicians mostly gave, or implied, a viral diagnosis and mainly recommended non-antibiotic treatment strategies. In the minority of cases where parents’ communication behaviours implied they may be seeking antibiotic treatment, antibiotics were not usually prescribed. Where clinicians did prescribe antibiotics, they voiced concern about symptoms or signs, including chest pain, discoloured phlegm, prolonged fever, abnormal chest sounds, or pink /bulging ear drums.
Conclusions
We found little evidence of a relationship between parents’ communication behaviours and antibiotic prescribing. Rather, where antibiotics were prescribed, this was associated with clinicians’ expressed concerns regarding symptoms and signs.
Similar content being viewed by others
Background
High rates of antibiotic prescribing have led to increased antimicrobial resistance (AMR) [1, 2] and higher rates of morbidity and mortality from resistant infections [3]. Understanding the drivers of antibiotic prescribing has therefore become a key priority for health research globally [4, 5]. Acute respiratory tract infections (RTI) in children are a common reason for antibiotic prescribing [6]. There are multiple influences on the decision to prescribe antibiotics, including clinicians’ interpretation of the clinical signs [7, 8], concern for the safety of the child [9, 10] and perceived pressure from parents [11, 12].
Another key influence on whether antibiotics are prescribed is communication between clinicians and patients or carers [13, 14]. We know that parents rarely make explicit requests for antibiotic treatment for their children [15, 16]. However, parents may suggest a possible diagnosis (e.g. “strep throat”) or symptoms (e.g. “chesty cough”) that could indicate a need for antibiotic treatment and lead clinicians to perceive parental antibiotic expectations [15, 17], which in turn is associated with higher antibiotic prescribing [12, 18].
Studies that found an association between antibiotic prescribing and clinician perception of parental expectations, also showed parents’ actual expectations of antibiotic treatment were not predictive of antibiotic prescribing [12]. When parents offer a possible diagnosis or identify concerning symptoms, they may be seeking reassurance that the consultation is justified or that their child is not seriously ill (rather than indirectly requesting antibiotics) [18]. Parents and clinicians often talk at cross purposes about the seriousness of the child’s illness and this miscommunication may contribute to over-prescription of antibiotics [19], with studies of parental views consistently finding a preference for no treatment for minor infections [10, 20].
Our systematic review found few studies examining the relationship between parent-clinician communication and antibiotic prescribing, with none in a UK context and most undertaken over a decade ago [19]. In the USA (a high antibiotic prescribing context), the relationship between actual parental expectations, clinician-perceived expectations and inappropriate antibiotic prescribing has been previously explored using survey data [12] and observational data from video-recordings of clinical encounters [12, 21]. Conversation analytic (CA) methods can be applied to detailed transcripts of recordings to identify the underlying rules and norms that guide key communication activities or tasks (such as soliciting patients’ problems, diagnosing and prescribing), and how these norms can affect outcomes [22]. Using CA methods, Stivers identified two key parental communication behaviours that occur in different phases of paediatric primary care consultations and appear to influence clinician perception of parental antibiotic expectations: firstly what is said at the beginning of the consultation and secondly what is said following treatment recomendation [21, 23]. At the beginning of the consultation, Stivers distinguishes between communications which lead clinicians to perceive treatment expectations (when parents suggest a “candidate diagnosis”, or “implied candidate diagnosis” using symptoms), and those clinicians perceive as being free of treatment expectations (a “symptoms only” presentation) [21, 23]. After the delivery of treatment recommendations by clinicians, Stivers distinguishes between clear acceptance and responses indicating “interactional resistance” (silence, a treatment obstacle or a question) [21]. These findings are supported by a Finnish CA study in the same context that examined parent-clinician communication and found that similar parental communication patterns influenced clinicians’ communication. However this study did not examine the influence on antibiotic prescribing (antibiotic prescribing rates were much lower than reported in the USA study) [24, 25].
Our study aims to build on this earlier work by examining whether these same parental communication patterns can be found in primary care consultations for children with RTI in the UK, and whether they are associated with antibiotic prescribing.
Method
The data consisted of primary care consultations for children with RTI that were recorded between May and December 2013. These recordings were made for a previous study and the data collection methods are described in detail elsewhere [26]. The previous study recorded 60 complete consultations, 56 video recorded and 4 audio only, the analysis for this study was conducted on the 56 consultations that were video recorded. Parents and children were recruited in six General Practices in the South-West of England selected to represent a range of neighbourhoods including both deprived and affluent. Thirteen clinicians agreed to participate, including nine General Practitioners (GPs), three Nurse Practitioners (NPs) and one Physician’s Assistant (PA). Eighty-three parents of children aged 3 months to 12 years who presented with an acute RTI with a cough were invited to participate, 72% agreed and provided written informed consent. 13 consultations included non-native speakers. The study design was guided by a Public Patient Involvement group of local parents.
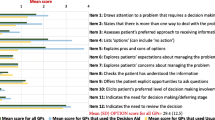
Our mixed methods CA approach combined qualitative CA-grounded coding of the recorded consultations with subsequent descriptive quantitative analysis [22, 27]. In preparation for the initial coding, the recordings were transcribed in detail according to standard Jeffersonian conventions [28]. A comprehensive coding scheme was developed that spanned parent, child and clinician activities across the whole consultation. Initial codes for each of the consultation activity phases – opening, problem presentation, history-taking, physical examination, diagnosis, treatment planning and closing - were developed deductively by CC, RB and JS, drawing on findings from published CA studies of routine primary care consultations [15, 21, 29, 30], and inductively by working with a 15% subset of our transcripts and recordings. This subset included a range of different practice settings, clinicians and outcomes. CC, RB and JS engaged in a series of CA data sessions each focused on a different activity phase. These involved repeatedly watching relevant extracts from the videos and working line-by-line through the transcripts to identify common patterns in the communication behaviours relating to key activities or tasks. Communication behaviours in our data not previously studied, for example safety-netting practices, were assigned new interaction codes.
A first version of the coding scheme was then drafted for testing. The scheme included a codebook with definitions of the codes, coding criteria and clear exemplars. Further focused meetings were then held to test these codes across the original subsample. Consequently, codes were refined or dropped and/or new codes were identified. A randomly selected further 15% subsample were then independently double coded by JS and RB and further amendments and revisions made based on discussions between JS, RB and CC. In the same way, a second and third 15% subsample were independently coded until consensus was reached on the coding scheme. This Four of these types were identified by previous checking and redefining the communication phenomena captured by the code labels ensured a robust coding framework. One researcher (JS) then applied this coding scheme to the whole data set. The frequencies of coded communication behaviours were then examined across the dataset and in relation to treatment recommendations.
This paper reports on the distribution of codes for parent problem presentation, diagnoses delivered, and treatments recommended by clinicians and the relationship between these.
Results
The 56 video-recorded consultations were for 60 children with RTI (in four consultations, two child patients were present), 78% of children were under 5 years and 67% were male (Table 1). The sample of patients and parents was diverse, from both deprived and affluent neighbourhoods and 36% of parents were of non-white ethnicity (Table 1). The 13 participating clinicians had varied experience from < 5 to > 15 years in primary care and included GPs, NPs and a Physician Assistant (Table 1). The consultation duration ranged from 4 min and 12 s to 28 min and 40 s, with an average of 10 min and 45 s.
Parent problem presentation
Five different types of problem presentation by parents were identified and coded (Table 2). Four of these types were identified by previous CA studies but one type ‘viral candidate diagnosis’ is identified and coded for the first time in this study. In the majority (41, 73%), the parents’ problem presentations did not imply an expectation of antibiotic treatment. These included ‘symptom only’ presentations, ‘viral candidate diagnosis’ (explicit or implied) and ‘candidate explanations’ for concerning symptoms such as vomiting. In the remaining cases (27%) parents either suggested candidate diagnoses (e.g. “chest infection”) or cited symptoms (e.g. “phlegmy … on the chest”) that a clinician may understand to imply a possible need or expectation for antibiotic treatment.
Clinician diagnoses and treatment recommendations
A viral diagnosis was the most common and delivered explicitly using the term “virus” or “viral” in 37 (66%) consultations and implied in a further nine (16%) consultations by terms like “cold’” or described as an unproblematic illness (Table 3). In six (11%) cases a diagnosis of a chest or ear “infection” was given, and one child was diagnosed with pneumonia. In three (5%) cases there was no explicit diagnosis, but specific symptoms were identified as concerning and linked to the prescription of antibiotics, implying the diagnosis of a possible bacterial infection.
The most common treatment recommendation was home care (Table 4). This varied widely from a simple watch and wait strategy to detailed instructions about how to manage the symptoms. Antibiotics were prescribed in 12 (21%) cases, eight (14%) for immediate consumption and four (7%) delayed prescriptions. Two children had both antibiotics and steroids prescribed, in both cases they were given a primary diagnosis of an infection, for which antibiotics were prescribed and the steroids (tablets or inhalers) were prescribed as additional symptom relief. Steroids alone were prescribed for 10 (18%) cases as symptom relief treatment. In three (5%) cases, over-the-counter (OTC) medicines (paracetamol and non-steroidal anti-inflammatory drugs and in one case with cough medicine in addition) were prescribed in response to direct requests for these from parents.
In 11 of the 12 cases where antibiotics were prescribed, the clinician linked this decision to specific clinical observations (Table 4). Immediate antibiotics were linked to sounds heard during the chest examination, pain in the chest, yellow phlegm and ear infection. Delayed antibiotics were linked to fever of long duration. There was one case where delayed antibiotics appeared to be issued in response to parental interactional resistance to a non-antibiotic treatment recommendation (see Table 6).
Relationships between forms of communication and treatment decisions
Parents’ problem presentations did not appear to be associated with antibiotic treatment decisions (Table 5). Antibiotics were most often prescribed following ‘symptoms only’ and ‘viral candidate diagnoses’ presentations. In the 15 consultations in which parents presented a candidate diagnosis (e.g. “chest infection”) or symptom (e.g. “it is on the chest”) that implied an antibiotic may be appropriate, antibiotics were prescribed twice and steroids three times (Table 5). Steroids were prescribed more often for ‘symptoms only’ and ‘viral candidate diagnosis’ presentation cases.
The most common response to any treatment recommendation was a simple acknowledgement, which was sometimes stated verbally and sometimes communicated non-verbally with a nod. In 43 (77%) cases, parents acknowledged the clinicians’ primary treatment recommendation by either nodding or saying just one or two words; in three cases (5%) parents actively accepted the recommendation; in six cases (11%) parents displayed active ‘interactional resistance’; and in the remaining four (7%) cases there was no clear response to the treatment recommendation (Table 6). After receiving an acknowledgement or acceptance from a parent, the clinician usually continued almost immediately to give further home care and safety-netting advice.
In the six cases where parents displayed active ‘interactional resistance’, parental responses to the treatment recommendation came in the form of a question. In one case the parent (P13) was responding to a ‘no-antibiotic’ treatment recommendation; in one case the parent (P19) was responding to a recommendation for antibiotic treatment; and in the remaining four cases, parents responding to home care recommendations. In the one case of ‘interactional resistance’ to a ‘no-antibiotic’ treatment recommendation, the parent questioned what to do after the recommended five-day watch and wait period and informed the GP that accessing same day appointments was difficult; a delayed prescription was subsequently issued for use if needed after 5 days (see Table 6). In the case of a parent resisting a recommendation for antibiotic treatment, parents asked a clarifying question about the reason the clinician felt antibiotics were needed (P19) (see Table 6). In the four cases of ‘interactional resistance’ to home care recommendations, parents were asking for more detailed advice on effective symptomatic treatments.
Discussion
Summary
In these consultations, parental communication behaviours did not appear to be linked with antibiotic prescribing. Where antibiotic-indicative candidate diagnoses were presented by parents, this was not associated with higher rates of antibiotic prescription. The most common problem presentation was “symptoms only”, which imply parents are seeking medical evaluation, rather than a particular diagnosis and treatment [21, 23]. In 50 of the 56 consultations, parents responded with acknowledgement or clear acceptance of the treatment recommendations, including parents who had used antibiotic-indicative presentations. Parents responded with active resistance in only six consultations. Clinicians recommended non-antibiotic treatment in the majority of cases and when they did prescribe antibiotics, it was usually linked to a symptom or sign about which they had expressed concern.
Comparison with existing literature
This study found that fewer parents used antibiotic implicative candidate diagnoses compared with the earlier US-based study [15], but the frequencies recorded here are similar to those reported by a recent Finnish study [24]. Our study was carried out in a time when awareness of over prescription of antibiotics was (and is) high and in a different health system context (UK) and where antibiotic prescribing is lower than in the US. The US study was also conducted in predominantly mid to high income populations, whereas our study population encompassed the full range of income levels. These contextual differences may account for the different findings. Our data provide evidence that in the current UK context, parents’ communication behaviours may not be a major influence on antibiotic prescribing in primary care (in hours) for RTI in children.
When parents offer a candidate diagnosis, they are both displaying their own expertise and justifying the need for a consultation. Parents’ communication behaviours within these consultations draw on their knowledge and experience as a way of furthering a shared understanding with the clinician [16, 19, 25]. When parents consult for an RTI in a child the use of a candidate diagnosis can be a means of directing the clinician’s attention to a key concern [31]. For example, using the term ‘chest infection’ may be a way of ensuring this possibility is evaluated by the clinician, and these concerns may be assuaged by a credible evaluation [20]. This study is the first to record the use of viral candidate diagnoses by parents, which may indicate that parents are using this form of problem presentation to indicate they are not seeking antibiotics.
The CA term ‘interactional resistance’ is often interpreted as parents opposing a treatment recommendation [32]. However, this term is meant to describe anything other than clear acceptance (e.g. the parent responds with silence, a minimal acknowledgement, a treatment obstacle or a question), in other words ‘resisting’ the norm or expected response of acceptance. The interactional consequence of interactional resistance is that progress towards next steps such as closing the consultation is delayed [21, 33]. In our study, as in previous work [25], we can see that parents are seeking to understand rather than challenge. Time pressure may be relevant here as clinicians feel the need for consultations to be completed quickly [8, 10], and may resort to prescribing as a way to end the discussion. Pressure to explain may be experienced as pressure to prescribe.
The antibiotic prescribing observed in this study was overtly linked to symptoms of concern observed by clinicians. There is variation between clinicians in the clinical symptoms and signs used to decide when to prescribe antibiotics [8, 34]. This may be because some clinicians are taking a more cautious approach, prescribing ‘just in case’ if they feel there is any risk of negative consequences to the child’s health or themselves (medico-legal) of not prescribing [9, 10].
Strengths and limitations
This was the first study in the UK to use videos of real consultations to explore associations between parental communication and antibiotic prescribing for children with RTIs. Although our study was smaller than previous work in the US (n = 360), it was similar to the Finnish study (n = 70) and our study population was more diverse than previous studies, which drew patients from predominantly mid to high income populations. This sample provides for a robust qualitative and descriptive analysis but limited the inferential statistical analysis possible. We recruited a diverse range of families from deprived and affluent neighbourhoods and included a large proportion of non-White British ethnicities, although few Asian. In five of the six practices, clinicians had no influence over which consultations were recorded. One practice triaged all patients requesting same day appointments and, while clinician selection cannot be ruled out, these 10 consultations had similar characteristics to the others. The use of oral steroids in 12 cases implies a significant proportion had a relatively severe illness and we captured a representative range of cases. Clinicians with a range of professional experience were recruited, although, since they had to ‘opt-in’ to the study, participating clinicians may differ from those who did not take part.
Conclusion
Antibiotic prescribing for children with RTI appears to be influenced mainly by clinicians’ reported interpretation of the symptoms and signs, rather than parental communication behaviours. Parental communication behaviours indicating that they may be seeking antibiotics appeared in few consultations and there was no clear relationship between parental communication behaviours and antibiotic prescribing. If antibiotic prescribing for RTI in children is to be improved, then interventions need a broader focus to include issues that may play a larger role, such as clinical uncertainty, safety concerns and external pressures on clinicians [9, 10, 35].
Availability of data and materials
The whole datasets generated and/or analysed during the current study are not publicly available because the data are videos of medical consultations and it was not possible to anonymise these (face of child patient, parents and clinicians are visible). However anonymised transcripts of the video encounters are available from the corresponding author on reasonable request.
Abbreviations
- AMR:
-
Antimicrobial resistance
- CA:
-
Conversation analytic
- GP:
-
General Practitioner
- NP:
-
Nurse Practitioners
- OTC:
-
Over-the-counter
- PA:
-
Physician’s Associate
- RTI:
-
Respiratory tract infections
References
Bryce A, Hay AD, Lane IF, et al. Global prevalence of antibiotic resistance in paediatric urinary tract infections caused by Escherichia coli and association with routine use of antibiotics in primary care: systematic review and meta-analysis. BMJ. 2016;352. https://doi.org/10.1136/bmj.i939.
Costelloe C, Metcalfe C, Lovering A, et al. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ. 2010;340:c2096 (Published 18 May 2010).
Butler CC, Hillier S, Roberts Z, et al. Antibiotic-resistant infections in primary care are symptomatic for longer and increase workload: outcomes for patients with E. coli UTIs. Br J Gen Pract. 2006;56(530):686–7.
Davies SC. Annual report of the chief medical officer 2011. London: Department of Health; 2013.
WHO. Antibiotic resistance: Multi-country public awareness survey. Geneva: WHO; 2015.
Finkelstein J, Metlay JP, Davis RL, et al. Antimicrobial use in defined populations of infants and young children. Arch Pediatr Adolesc Med. 2000;154(4):395–400. https://doi.org/10.1001/archpedi.154.4.395.
Butler CC, Kelly MJ, Hood K, et al. Antibiotic prescribing for discoloured sputum in acute cough/lower respiratory tract infection. Eur Respir J. 2011;38(1):119–25. https://doi.org/10.1183/09031936.00133910.
Horwood J, Cabral C, Hay AD, et al. Primary care clinician antibiotic prescribing decisions in consultations for children with RTIs: a qualitative interview study. Br J Gen Pract. 2016;66(644):e207–e13. https://doi.org/10.3399/bjgp16X683821.
Cabral C, Lucas PJ, Ingram J, et al. “It's safer to … ” parent consulting and clinician antibiotic prescribing decisions for children with respiratory tract infections: An analysis across four qualitative studies. Soc Sci Med. 2015;136–137:156–64. https://doi.org/10.1016/j.socscimed.2015.05.027.
Lucas PJ, Cabral C, Hay AD, et al. A systematic review of parent and clinician views and perceptions that influence prescribing decisions in relation to acute childhood infections in primary care. Scand J Prim Health Care. 2015;33(1):11–20. https://doi.org/10.3109/02813432.2015.1001942.
Britten N. Patients' expectations of consultations: patient pressure may be stronger in the doctor's mind than in the patient's. BMJ. 2004;328(7437):416–7.
Mangione-Smith R, McGlynn EA, Elliott MN, et al. The relationship between perceived parental expectations and pediatrician antimicrobial prescribing behavior. Pediatrics. 1999;103(4 Pt 1):711–8.
Cals JWL, Butler CC, Hopstaken RM, et al. Effect of point of care testing for C reactive protein and training in communication skills on antibiotic use in lower respiratory tract infections: cluster randomised trial. BMJ. 2009;338. https://doi.org/10.1136/bmj.b1374.
Little P, Stuart B, Francis NA, et al. Effects of internet-based training on antibiotic prescribing rates for acute respiratory-tract infections: a multinational, cluster, randomised, factorial, controlled trial. Lancet. 2013;382(9899):1175.
Stivers T. Presenting the problem in pediatric encounters: "symptoms only" versus "candidate diagnosis" presentations. [references]. Health Commun. 2002;14(3):299–338.
Stivers T. Prescribing under pressure: parent-physician conversations and antibiotics. Oxford: Oxford University Press; 2007.
Stivers T. Participating in decisions about treatment: overt parent pressure for antibiotic medication in pediatric encounters. Soc Sci Med. 2002;54(7):1111–30. https://doi.org/10.1016/S0277-9536(01)00085-5.
Stivers T, Mangione-Smith R, Elliott MN, et al. Why do physicians think parents expect antibiotics? What parents report vs what physicians believe. J Fam Pract. 2003;52(2):140–8.
Cabral C, Horwood J, Hay A, et al. How communication affects prescription decisions in consultations for acute illness in children: a systematic review and meta-ethnography. BMC Fam Pract. 2014;15(1):63.
Cabral C, Ingram J, Hay AD, et al. “They just say everything's a virus” - parent's judgment of the credibility of clinician communication in primary care consultations for respiratory tract infections in children: A qualitative study. Patient Educ Couns. 2014;95:248–53. https://doi.org/10.1016/j.pec.2014.01.010.
Stivers T. Non-antibiotic treatment recommendations: delivery formats and implications for parent resistance. Soc Sci Med. 2005;60(5):949–64.
Heritage J, Clayman SE. Talk in action: interactions, identities and institutions. Boston: Wiley-Blackwell; 2010.
Stivers T. Presenting the problem in pediatric encounters: "symptoms only" versus "candidate diagnosis" presentations. Health Commun. 2002;14(3):299–338. https://doi.org/10.1207/s15327027hc1403_2.
Ijäs-Kallio T, Ruusuvuori J, Perakyla A. Patient involvement in problem presentation and diagnosis delivery in primary care. Commun Med. 2010;7(2):131–41.
Ijäs-Kallio T, Ruusuvuori J, Perakyla A. Patient resistance towards diagnosis in primary care: implications for concordance. Health. 2010;14(5):505–22.
Cabral C, Ingram J, Lucas PJ, et al. Influence of clinical communication on parents’ antibiotic expectations for children with respiratory tract infections. Ann Fam Med. 2016;14(2):141–7. https://doi.org/10.1370/afm.1892.
Stivers T. Coding social interaction: a heretical approach in conversation analysis? Res Lang Soc Interact. 2015;48(1):1–19. https://doi.org/10.1080/08351813.2015.993837.
Jefferson G. Glossary of transcript symbols with an introduction. In: Lerner GH, editor. Conversation analysis: Studies from the first generation. Amsterdam: John Benjamins Publishing Company; 2004. p. 13–31.
Heritage J, Elliott MN, Stivers T, et al. Reducing inappropriate antibiotics prescribing: the role of online commentary on physical examination findings. [references]. Patient Educ Couns. 2010;81(1):119–25.
Heritage J, Stivers T. Online commentary in acute medical visits: a method of shaping patient expectations. Soc Sci Med. 1999;49(11):1501–17. https://doi.org/10.1016/S0277-9536(99)00219-1.
Ingram J, Cabral C, Hay AD, et al. Parents' information needs, self-efficacy and influences on consulting for childhood respiratory tract infections: a qualitative study. BMC Fam Pract. 2013;14:106.
Scott J, Cohen D, DiCicco-Bloom B, et al. Antibiotic use in acute respiratory infections and the ways patients pressure physicians for a prescription. J Fam Pract. 2001;50(10):853–8.
Barnes RK. Preliminaries to treatment recommendations in UK primary care: a vehicle for shared decision making? Health Commun. 2018;33(11):1366–76. https://doi.org/10.1080/10410236.2017.1350915.
Brookes-Howell L, Hood K, Cooper L, et al. Clinical influences on antibiotic prescribing decisions for lower respiratory tract infection: a nine country qualitative study of variation in care. BMJ Open. 2012;2. https://doi.org/10.1093/fampra/cmt052.
Hay AD, Redmond NM, Turnbull S, et al. Development and internal validation of a clinical rule to improve antibiotic use in children presenting to primary care with acute respiratory tract infection and cough: a prognostic cohort study. Lancet Respir Med. 2016;4(11):902–10. https://doi.org/10.1016/S2213-2600(16)30223-5.
Acknowledgements
We would like to thank all the parents and primary care clinicians who kindly agreed to allow us to record their consultations, and our parent Patient and Public Involvement group who advised on study procedures.
Funding
The research was funded by the National Institute for Health Research (NIHR) School for Primary Care Research (SPCR 204). The funder did not have any role in study design, data collection or interpretation or in writing of the manuscript. The views expressed in this article are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care.
Author information
Authors and Affiliations
Contributions
CC led the study, collected the primary data, contributed to the development of the coding scheme and led the analysis that is reported in this paper. RB led the development of the Conversation Analysis informed coding scheme. JS contributed to the development of the coding scheme and conducted the majority of the data coding. JH, PL, JI, NR, JK and AH contributed to the development of the study design, the interpretation of the data and the writing of the final paper. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was granted ethical approval by the National Research Ethics Committee South West – Frenchay (13/SW/0008). All adult participants provided written consent to participation and publication of anonymised quotes. Parents consented on behalf of their children and children were shown an age appropriate illustrated information sheet and asked to give verbal assent.
Consent for publication
All adult participants provided written consent to publication of anonymised quotes.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Cabral, C., Horwood, J., Symonds, J. et al. Understanding the influence of parent-clinician communication on antibiotic prescribing for children with respiratory tract infections in primary care: a qualitative observational study using a conversation analysis approach. BMC Fam Pract 20, 102 (2019). https://doi.org/10.1186/s12875-019-0993-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-019-0993-9