Abstract
Background
Renal failure carries high mortality even in high-resource countries. Little attention has been paid to renal failure patients presenting acutely in emergency care settings in low-to-middle income countries (LMIC). Our aim was to describe the profile, management strategies and outcome of renal failure patients presenting with indications for emergent dialysis to an urban Emergency Department (ED) in a tertiary public hospital in Tanzania.
Methods
This was a prospective cohort study of consecutive patients (age ≥ 15 yrs) presenting to the Emergency Medicine Department of Muhimbili National Hospital from September 2017 to February 2018. All patients with renal failure and complications requiring acute dialysis were included. A structured data collection sheet was used to gather demographics, clinical presentation, management strategies and outcomes. Data were summarized with descriptive statistics. Logistic regressions were performed to determine factors associated with receiving dialysis and with mortality.
Results
We enrolled 146 patients, median age was 49 years (IQR 32–66 years), and 110 (75.3%) were male. Shortness of breath 67 (45.9%) and reduced urine output 58 (39.7%) were the most common presenting complaints. The most common complications were hyperkalemia 77 (53%), uremic encephalopathy 66 (45%) and pulmonary edema 54 (37%). All patients were hospitalized, and 61 (42%) received dialysis. Overall mortality was 39% (57 patients); the mortality in non-dialysed patients was 53% vs. 20% (p < 0.0005) in those receiving dialysis. 54% of patients with health insurance were dialyzed, compared to 39% who paid out of pocket (adjusted OR = 0.3, 95%CI: 0.1–0.9). Patients (≥55 years) were less likely to be dialysed (adjusted OR = 0.2 [0.1–0.9]). Independent predictors of mortality were vomiting (OR = 6.2, 95%CI: 1.8–22.2), oliguria (OR = 3.4, 95%CI: 1.2–9.5), pulmonary edema (OR = 4.6, 95%CI: 1.6–14.3), creatinine level > 1200umol/L (OR = 5.0 95%CI: 1.4–18.2), and not receiving dialysis (OR = 8.0, CI: 2.7–23.5). Female sex had a lower risk of dying (OR = 0.13, CI: 0.03–0.5).
Conclusions
In this ED in LIC, acute complications of renal failure created a need for ED stabilization and emergent dialysis. Overall in-hospital mortality was high; significantly higher in undialysed patients. Future studies in LICs should focus on identification of categories of patients that will do well with conservative therapy.
Similar content being viewed by others
Background
Renal disease is common worldwide. Chronic Kidney Disease (CKD) affects up to 16% of the world population [1], while Acute Kidney Injury (AKI) is associated with 5–20% of hospital admissions [2, 3]. Renal failure carries a high mortality rate in both high and low resource countries [4]. Emergency departments are frequently the first site of care for patients who develop acute kidney injury and those who develop complications from chronic kidney disease. Appropriate management of these patients can be life-saving.
In developing countries, the prevalence of CKD is similar to that of high resource countries, 13·9%, while that of AKI is up to 7% [3]. To a certain extent the etiologies are similar to those in high resource countries with non-communicable diseases such as hypertension, diabetes, lipid disorders being major contributors. However, in LMIC’s, communicable diseases such as kidney infections, schistosomiasis, leishmaniasis and Human Immunodeficiency Virus (HIV) infections are also significant risk factors for the development of renal injury [5]. Poor access to care for some of these diseases (e.g. hypertension) result in earlier onset of CKD than in high resource countries and late presentation and financial inability to access advanced care such as dialysis and renal transplant contribute to higher mortality rates from renal disease [4].
Management of acute complications of renal failure at the emergency medicine department (EMD) rests on early recognition, early resuscitation, and treatment of the underlying causes to prevent further renal damage [5]. Patients present with life-threatening electrolyte imbalance, commonly hyperkalemia, severe metabolic acidosis and uremic complications such as pulmonary edema, uremic pericarditis and encephalopathy. Non-invasive ventilation such as continuous positive airway pressure or intubation may be needed to manage patients with respiratory failure due to fluid overload. However, these are often temporizing measures, and dialysis is often necessary.
In Tanzania, as in much of sub-Saharan Africa, the infrastructure for emergency care is still in development. Dialysis availability is limited throughout the country [6, 7]. Recent studies on challenges and outcomes of hemodialysis showed a substantial challenges in accessing dialysis services, which is compounded with the high cost related to its utilization [8]. Muhimbili National Hospital (MNH), a tertiary referral hospital, is among few public hospitals in the country with full capacity emergency medicine department (EMD) staffed by Emergency Medicine specialists, which is in the position to provide stabilization for patients with acute complications of renal failure. However, little is known about the number and characteristics of patients presenting to the EMD, how they are managed or the outcome of EMD treatment. Moreover, it is unknown how many who meet requirements for dialysis receive it, and how many patients survive to discharge. Determining the numbers of patients presenting with acute complications of renal failure, their clinical characteristics and requirements for dialysis, and their current outcomes can help improve management and direct scarce resources appropriately.
Methods
Study design
This was a prospective cohort study of patients aged 15 years and above presenting to the EMD of the national referral hospital in Tanzania from September 2017 to February 2018, with acute symptoms of renal failure requiring emergent dialysis.
Study setting
The study was conducted at the EMD and nephrology unit of Muhimbili National Hospital (MNH), which is a tertiary public hospital located in Dar es salaam, Tanzania. This hospital has approximately 1500 beds; patients are referred from different districts and regional facilities across Tanzania. At the EMD-MNH, more than 1200 patients attend weekly. The dialysis unit at MNH has about 40 machines running about 80 dialysis sessions per day. The hospital offer emergency dialysis to all patients with emergency presentations of renal failure (including symptomatic hyperkalemia, pulmonary oedema, uremic encephalopathy and pericarditis), patients with chronic renal failure, receives care in line with existing national guideline. All patients with emergency conditions receives care regardless of the ability to pay, while regular patients receives care as per the cost sharing (Government subsidized cost), insurance, exemption and private categories.
Participants
We defined renal failure using RIFLE criteria [9]. Since RIFLE criteria use creatinine levels and urine output measured at 12 or 24 h intervals, and this was not feasible in the emergency setting where a patient might spend less time, for this study we used reported or observed oliguria or anuria for 12 h and above. Eligible participants were those with renal failure who presented to the ED with one or more acute complications such as fluid overload, severe electrolyte imbalance, acute drug intoxication, severe metabolic acidosis and uremia that required emergent dialysis. Patients with pregnancy, trauma, obstructive oliguria and those who did not consent were excluded.
Study protocol
A researcher was scheduled for 12 h a day throughout the study period; shifts alternated days and nights. The research also collected information of all patients by chart reviewing and identified patients that came in during the off hours. During these periods, all patients presenting to the resuscitation area of the ED were screened by real-time chart review for provisional and final diagnoses and rounding with physicians; the diagnosis of renal failure was confirmed by having elevated serum creatinine levels. We then determined which patients had complications requiring dialysis and these patients were enrolled.
After obtaining patients consent, a structured data collection sheet was used to gather demographic information, clinical presentation, management strategies and outcomes. Laboratory results were followed up through electronic system to get the data for creatinine levels in case the results were not recorded in the electronic medical record system at ED or in the patient’s file. Patients were followed until hospital discharge or up to 30 days in the wards for the outcomes.
Outcomes
Primary outcome was mortality rate (ED mortality and 30-days in-hospital mortality rates). Secondary outcomes were risk factors for mortality, whether or not patients received dialysis, and predictors of receiving dialysis.
Data analysis
As there were no similar studies on the outcomes of patients admitted with complications of renal failure, we based the sample size estimate on a mortality rate of 34% for patients with AKI hospitalised in a US study [10]. Using a 95% confidence interval, a minimum sample size of 119 was calculated.
All the data collected were entered into an electronic database (Redcap), and then exported into excel sheet and transferred to the Statistical Package for Social Sciences (SPSS), version 20 for analysis. Data were summarized with descriptive statistics including median and frequencies. Logistic regression was used to determine factors associated with mortality and receipt of dialysis. Patients who died in the ED were excluded from these analyses as they could not be evaluated for dialysis access. A probability value of less than 5% was considered statistically significant.
Results
Demographics and clinical characteristics of study participants
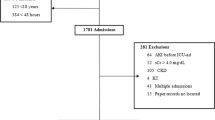
Of the 3013 patients admitted to resuscitation rooms during the study period, 266 (8.8%) had a diagnosis of renal failure (71 AKI versus 195 CKD). (Fig. 1) Among these, we enrolled 146 (55%) patients who had indications for dialysis. Majority of participants were male 110 (75.3%) and aged above 55 years 55(37.7%) while median age was 49 years (IQR 32 to 66 years). The majority 88 (62%), had not gone beyond primary school education. More than half (52%) were referred from government health facilities; 74% (108) were uninsured and paying out of pocket (Table 1). The most common complaints of participants were shortness of breath 67(45.9%), reduced urine output 58 (39.7%) and generalized swelling 51(34.9%). The main presenting complications diagnosed among study participants were hyperkalemia 77(53%), uremic encephalopathy 66 (45%) and pulmonary edema 54 (37%) (Table 2).
Management given and outcome at ED
Most of ED management was directed for treatment of hyperkalemia and pulmonary fluids overload (Fig. 2). The ED administered non-invasive ventilation (NIV) (33%), Calcium gluconate (33%), insulin with dextrose (32%), diuretics (30%), and nebulization with salbutamol (24%), antibiotics (20%), nitrates (19%) and sodium bicarbonates (16%). Few patients received antihypertensives (4%) and 1% of the participants received invasive ventilation and inotropes. 2.7% (4/146) patients died at ED, while 97.3% (142/146) were admitted alive.
Frequency and predictors of dialysis
Out of 142 patients who were admitted with emergency complications of renal failure in need of dialysis, 61 (42.8%) received dialysis while 81 (57.2%) were managed conservatively.
In multivariate logistic regression analysis, lack of insurance and older age were independent predictors of not receiving dialysis (OR: 0.30; 95%CI: 0.1–0.9) and OR 0.2 95% CI 0.1–0.9), respectively (Table 3).
Mortality
Among all 146 enrolled patients, four patients died in the ED while 53 patients died in the hospital, giving an overall mortality rate of 39%, (95%CI 31.1–45.0%). Table 4 shows the results of univariate and multivariate analysis of risk factors for mortality. The following patient characteristics were independent predictors for mortality: vomiting at presentation (OR: 6.23; 95%CI: 1.75–22.2), oliguria (OR: 3.40; 95%CI: 1.22–9.48), body swelling (OR: 3.40; 95%CI: 1.17–9.88), altered mental status (OR: 7.48; 95%CI:1.90–29.41), pulmonary edema (OR: 4.60; 95%CI: 1.6–13.3), and serum creatinine level above 1200ummol/L (OR: 5.02; 95%CI: 1.4–18.20). Hospital management, specifically dialysis, was the strongest predictor of mortality: Among the 61 patients dialyzed, there were 12 (20.3%) deaths, and among the 85 not dialyzed, there were 45 deaths (53%). Patients who were not dialyzed were significantly more likely to die than those dialyzed. (OR: 8.02; 95%CI: 2.7–23.5) Females were less likely to die than males (OR: 0.13; 95%CI: 0.03–0.53) Table 4.
Discussion
Prior studies of patients with renal failure attending emergency departments come from high-income countries (HIC), where demographics and etiology of renal failure may differ [8,9,10,11,12,13] In addition, low-to-middle income countries (LMIC) generally have poor access to primary care, and individuals often delay seeking care. LMIC have less availability of life-saving treatments, including ventilators, dialysis and IV medications. These factors can result in different management strategies and outcomes for patients. To our knowledge, there have been no previous studies in LMIC determining the number of patients presenting to the ED with emergency complications of renal failure or their characteristics.
During the study period, 266 patients presented with renal failure, approximately 8.8% of the patients attending the ED resuscitation rooms. Of these, 146 met criteria for emergency dialysis. Most patients (75.3%) in our study were males, similar to previous published studies across European countries [14, 15]. The median age was 49 years, which is higher than the average ED population, which has a median age of 30 years [16]. However this is lower than patients presenting to EDs in HIC’s [17, 18]. This could be attributed to the presence of untreated comorbidities such as hypertension, unique etiologies of renal failure in sub-Saharan Africa, and less access to preventive care.
Patients with low education levels and no health insurance made up the majority of the patients, while in HIC the majority had higher education [19]. This could be a result of the fact that MNH is a public hospital, and people with higher education and health insurance are likely to opt for other centers when seeking medical care. However, another potential reason is that those with insurance and higher education get health care more regularly, and may be on chronic dialysis, thus are less likely to present to any ED with complications of renal failure.
Similar to studies from HIC’s, the most common symptom reported was shortness of breath (45.9%) although in a US study, this was found in a higher proportion (61%) of patients [20]. There were relatively more patients with uremic encephalopathy (45%) and vomiting (24%) compared to 6.6 and 8.2% respectively in previous HIC literature [15, 20]. Most notably, more than 50% of our patients had hyperkalemia, compared to studies in HIC’s where hyperkalemia in patients presenting to ED with renal failure requiring dialysis was found in less than 10 % [19, 21]. This is likely due to the late presentation of renal failure in those not getting regular care, as well as those who have renal failure not getting dialysis.
Temporizing management given at ED suggested a significant stabilizing effect in which less than 3 % of patients died at ED while others were admitted alive to renal units to receive definitive management. This is similar to the mortality of the ED population with renal failure in HIC [22].
Our study found that, overall 30-day mortality of patients who needed dialysis was somewhat higher (39%) than in developed countries which had a mortality of around 8.8% [17]. Higher mortality found in our study can be attributed to late presentation to the hospital and lack of dialysis in more than 50% of patients who meet the indications. In developed countries more than 80 % of those admitted to renal and dialysis units receive dialysis [20].
The strongest predictor for mortality in our population was dialysis; non-dialyzed patients had more than eight times higher odds of dying than those who got dialyzed. This is consistent with a previous study done in a high income setting in which less than 10 % of those who were dialyzed died [15]. We found that mode of payment and age, were associated with the probability of being dialyzed or not. Not having health insurance (i.e. paying out of pocket), reduced the odds of dialysis by 70%. Age 55 years and above decreased the odds of dialysis by almost 80%. This is different from a study in the US which showed shortness of breath was the only factor in predicting dialysis [20, 23]. Dialysis units are limited in Tanzania and other LMIC’s and thus a form of triage occurs: it is widely accepted that more advanced age is associated with poor outcome and due to limited resources in Tanzania; the younger population is usually preferred. Unfortunately, inability to pay for dialysis is also a barrier to receiving it. Study by Meremo et al. among patients receiving dialysis at the University teaching identified potential predictors of poor outcomes to be gender, type of kidney disease, residence of patients and insurance status of patient [8].
Limitations
This was a single-centre study, which may affect generalizability of its results. We did however reach the appropriate sample size to increase accuracy. There was also some missing patient information at medical records and uncharted documentation of point-of-care and laboratory results. Some patients may have been missed due to the fact that the research assistant was not present at the emergency department all the time, and this could underestimate the prevalence of the problem. However, as the shifts were varied in timing, we feel that this sample is representative of our population. Some screened patients were identified as potentially eligible but left the department before they could be enrolled; however, this number is small.
Conclusion
In this ED in LIC, we found that acute complications of renal failure created a substantial need for ED stabilization and emergent dialysis. Overall in-hospital mortality was high; significantly higher in undialysed patients. Future studies in LICs should focus on identification of categories of patients that will do well with conservative therapy.
Abbreviations
- AKF:
-
Acute renal failure
- AKI:
-
Acute Kidney Injury
- BUN:
-
Blood urea nitrogen
- CKD:
-
Chronic Kidney Disease
- CPAP:
-
Continuous positive pressure ventilation
- ED:
-
Emergency Medicine Department
- EMD:
-
Emergency Medicine Department
- GFR:
-
Glomerular Filtration Rate
- INR:
-
International Normalized Ratio
- IRB:
-
Institutional Review Board
- IV:
-
Intravenous
- IVF:
-
Intravenous fluids
- LIC:
-
Low Income Countries
References
Global Facts: About Kidney Disease [Internet]. The National Kidney Foundation. 2015 [cited 2017 Mar 21]. Available from: https://www.kidney.org/kidneydisease/global-facts-about-kidney-disease
Nor FSM, Draman CR, Seman MR, Manaf NA, Ghani ASA, Hassan KA. Clinical outcomes of acute kidney injury patients treated in a single-center, sub-urban satellite hospital. Saudi J Kidney Dis Transplant. 2015;26(4):725.
Susantitaphong P, Cruz DN, Cerda J, Abulfaraj M, Alqahtani F, Koulouridis I, et al. World incidence of AKI: a meta-analysis. Clin J Am Soc Nephrol. 2013;8(9):1482–93.
Fry AC, Farrington K. Management of acute renal failure. Postgrad Med J. 2006;82(964):106–16.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for Sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–10.
Kohli HS, Bhat A, Jairam A, Aravindan AN, Sud K, Jha V, et al. Predictors of mortality in acute renal failure in a developing country: a prospective study. Ren Fail. 2007;29(4):463–9.
Joslin J, Ostermann M. Care of the Critically ill Emergency Department Patient with acute kidney injury. Emerg Med Int. 2011 Nov 24;2012:e760623.
Meremo AJ, Ngilangwa DP, Mwashambwa MY, Masalu MB, Kapinga J, Tagalile R, et al. Challenges and outcomes of haemodialysis among patients presenting with kidney diseases in Dodoma. Tanzania BMC Nephrol. 2017;18(1):212.
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute renal failure – definition, outcome measures, animal models, fluid therapy and information technology needs: the second international consensus conference of the acute Dialysis quality initiative (ADQI) group. Crit Care. 2004;8(4):R204–12.
Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol JASN. 2005;16(11):3365–70.
Kilonzo KG. Outcome of acute peritoneal dialysis in NORTHERN Tanzania. Perit Dial Int. 2012 May;32(3):261–6.
Stanifer, John. The epidemiology of chronic kidney disease in sub-Saharan Africa: a systematic review and meta-analysis.
Stanifer JW, Maro V, Egger J, Karia F, Thielman N, Turner EL, et al. The epidemiology of chronic kidney disease in Northern Tanzania: a population-based survey. PLoS One. 2015;10(4):e0124506.
Nash K, Hafeez A, Hou S. Hospital-acquired renal insufficiency. Am J Kidney Dis Off J Natl Kidney Found. 2002;39(5):930–6.
Hou SH, Bushinsky DA, Wish JB, Cohen JJ, Harrington JT. Hospital-acquired renal insufficiency: a prospective study. Am J Med. 1983;74(2):243–8.
Reynolds T, Sawe HR, Lobue N, Mwafongo V. Most frequent adult and pediatric diagnoses among 60,000 patients seen in a new urban emergency Department in Dar Es Salaam. Tanzania Ann Emerg Med. 2012;60(4):S39.
Kazancioglu R, Kutlu C, Sezer Caymaz M, Tatli E, Sar F. Demographic analysis of renal failure patients presenting to the emergency unit. Hong Kong J Nephrol. 2007;9(2):82–5.
Sacchetti A, Harris R, Patel K, Attewell R. Emergency department presentation of renal dialysis patients: indications for ems transport directly to dialysis centers. J Emerg Med. 1991;9(3):141–4.
Hecking M, Bieber BA, Ethier J, Kautzky-Willer A, Sunder-Plassmann G, Säemann MD, et al. Sex-Specific Differences in Hemodialysis Prevalence and Practices and the Male-to-Female Mortality Rate: The Dialysis Outcomes and Practice Patterns Study (DOPPS). PLoS Med [Internet]. 2014 28 [cited 2018 May 17];11(10). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4211675/
Brück K, Stel VS, Gambaro G, Hallan S, Völzke H, Ärnlöv J, et al. CKD Prevalence Varies across the European General Population. J Am Soc Nephrol. 2015 Dec 23;ASN.2015050542.
Pani A, Floris M, Rosner MH, Ronco C. Hyperkalemia in hemodialysis patients. Semin Dial. 2014;27(6):571–6.
Acedillo RR, Wald R, McArthur E. Nash DM. James MT, et al. Characteristics and Outcomes of Patients Discharged Home from an Emergency Department with AKI. Clin J Am Soc Nephrol CJASN: Silver SA; 2017.
Xue JL, Daniels F, Star RA, Kimmel PL, Eggers PW, Molitoris BA, et al. Incidence and mortality of acute renal failure in Medicare beneficiaries, 1992 to 2001. J Am Soc Nephrol JASN. 2006;17(4):1135–42.
Acknowledgements
The authors would like to thank all emergency department staff and participants for their support in this project.
Funding
This was a non-funded project. The principal investigators used their own funds for logistics, data collection and analysis.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on request.
Author information
Authors and Affiliations
Contributions
ES was involved in the conceptualization, study design, data acquisition and entry, data analysis, interpretation and writing original draft of the manuscript. HRS contributed to the initial conception, design of the study and methodology, critically revised the analysis, interpretation and the manuscript. BM contributed to the initial conception, revised data analysis, interpretation and the manuscript. EM contributed to the initial conception, revised data analysis and interpretation and revised the manuscript. JAM contributed to the initial conception, revised data analysis and interpretation and revised the manuscript. SSK contributed to the design of the study, revised the methodology, analysis and interpretation and manuscript. EW contributed to the initial conception, design of the study, revised the methodology, data analysis and interpretation and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Permission to conduct the study was requested and granted from Muhimbili national hospital after review and approval by Institutional Review Board of Muhimbili University of Health and Allied Science (MUHAS). Written informed consent was sought from all patients, and child assent and parental permission sought prior to enrollment into the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflicts of interest.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Sylvanus, E., Sawe, H.R., Muhanuzi, B. et al. Profile and outcome of patients with emergency complications of renal failure presenting to an urban emergency department of a tertiary hospital in Tanzania. BMC Emerg Med 19, 11 (2019). https://doi.org/10.1186/s12873-019-0229-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12873-019-0229-2