Abstract
Background
Serum fatty acid (s-FA) compositions and their correlation with serum lipids (s-LPs) such as total cholesterol (T-CHO) and triglycerides (TG) have been reported in healthy young subjects. However, little is known about such features in acute ischaemic stroke (AIS). The aim of our study was to investigate s-FA characteristics and their correlation with AIS in elderly patients.
Methods
We conducted a cross-sectional study of patients aged 50 years or older who were admitted between September 2015 and March 2017 within 24 h of the first AIS onset. We evaluated concentrations and compositions of s-FAs and their association with s-LPs, age, and ischaemic stroke subtypes, including large-artery atherosclerosis (LAA), small-vessel occlusion (SVO), and cardioembolism (CE) or others.
Results
One hundred ninety-one patients met our inclusion criteria. Their average age was 74.4 years, mean T-CHO and median TG were 203.4 and 94.5 mg/dl, respectively, and median or mean concentrations of palmitic acid (PA), oleic acid (OlA), linoleic acid (LiA), and docosahexaenoic acid (DHA) were 680.7, 602.5, 795.2, and 136.9 μg/ml, respectively, with mean compositions of 23.7, 21.3, 27.1, and 4.4%, respectively. PA, OlA, and LiA concentrations were weakly negatively associated with age and positively correlated with TG. In LAA or SVO (LAA_SVO) and CE or others (CE_O), mean age was 71.9 and 77.4 years (p < 0.001), mean T-CHO was 213.9 and 191.2 mg/dl (p < 0.0001), median TG was 106.5 and 88.5 mg/dl (p < 0.01), median PA was 717.2 and 648.4 μg/ml (p < 0.01), median OlA was 638.2 and 567.5 μg/ml (p < 0.01), and median LiA was 844.7 and 728.5 μg/ml (p < 0.01), respectively. DHA composition was weakly positively correlated with age. There were no differences in PA, OlA, LiA, and DHA compositions between LAA_SVO and CE_O.
Conclusions
In AIS elderly patients, concentrations, rather than compositions of PA, OlA, and LiA, correlated with age, TG, and ischaemic stroke subtypes. Patients with LAA_SVO were younger and had higher concentrations of PA, OlA, and LiA than those with CE_O. There were no differences in such compositions between LAA_SVO and CE_O.
Similar content being viewed by others
Background
Previous studies have reported compositions of serum fatty acids (s-FAs) such as saturated fatty acids (SFAs), n-6 polyunsaturated fatty acids (n-6 PUFAs), n-9 monounsaturated fatty acid (n-9 MUFA), and n-3 polyunsaturated fatty acids (n-3 PUFAs), and their correlation with serum lipids (s-LPs) in healthy young or middle-aged human subjects [1,2,3,4,5]. The proportion of n-6 PUFAs, as a fraction of total fatty acids, decreases with increasing age. Compositions of eicosapentaenoic acid (EPA) or docosahexaenoic acid (DHA) were found to be positively correlated with serum total cholesterol (T-CHO), compositions of stearic acid (StA) or oleic acid (OlA) were positively correlated with serum triglycerides (TGs), and compositions of linoleic acid (LiA) or arachidonic acid (AA) were negatively correlated with TGs [1].
Further, a comparison of lipid fatty acids based on concentration basis vs composition (weight %) was reported for patients with and without coronary artery disease (CAD), concluding that serum concentrations of lipid fatty acids are more accurate reflections of changes in lipid fatty acids rather than compositions [6]. Concentrations of palmitic acid (PA), StA, OlA, LiA, and AA were found to be higher, and concentrations of EPA were lower in subjects with CAD than in subjects without CAD, whereas compositions of PA and StA were higher and those of EPA and DHA were lower in subjects with CAD [6]. A previous study also reported that people with higher serum levels of saturated fatty acids, n-9 MUFA, and n-6 PUFAs more frequently experienced lacunar or atherosclerotic stroke during middle age (50 to 74 years old) [7]. Serum FA concentrations and compositions might thus be associated with acute ischaemic stroke (AIS). However, limited information is available regarding such parameters and their association with AIS in elderly patients. The aim of our retrospective study was to investigate s-FA concentrations, s-FA compositions, and their correlation with age, serum lipids, and ischaemic stroke subtypes in AIS elderly patients.
Methods
We conducted a cross-sectional study of acute ischaemic stroke patients aged 50 years or older who 1) were admitted to our institution between September 2015 and March 2017 within 24 h of first stroke onset and then 2) underwent blood evaluations of s-LPs and s-FAs at arrival. We excluded patients who used statins, supplemental n-3 PUFA, fibrates, or ezetimibe at the onset. Additionally, we excluded those with a pre-hospital modified Rankin scale (mRS) score of 3 or more or a body mass index (BMI) less than 18.5, which was defined as severe disability or underweight according to the World Health Organisation (WHO) guidelines, as we determined that possible malnutrition was not appropriate for our investigation.
Measurements
Serum T-CHO, TG, and HDL-cholesterol (HDL-C) were measured through enzymatic analysis using reagents manufactured by Denka Seiken. A BioMajesty 6050 (JEOL Ltd., Tokyo, Japan) was used for measurements. For this purpose, 1.0 ml of serum was used to analyse fatty acids. Serum fatty acids were analysed at the Safety studies section at BML, Inc. (Tokyo, Japan). Fatty acids were extracted according to the general technique of Bligh and Dyer using tricosanoic acid (Nu-Chek Prep, Inc., MN, USA) as an internal standard. The lipid extracts were hydrolysed and extracted with chloroform and evaporated to dryness under nitrogen. After a 30% potassium methoxide methanol solution (FUJIFILM Wako Pure Chemical Corporation, Osaka, Japan) was added to the residual sample, it was incubated at 100 °C for 5 min and cooled. Boron trifluoride methanol reagent was added and incubated at 100 °C for 10 min for methyl esters. The samples were extracted with hexane before analysis. These samples were analysed with a capillary GC: column (BPX70, 30 m × 0.22 mm ID, 0.25 μm film thickness; SHIMADZU GLC Ltd., Tokyo, Japan). The gas chromatograph was a GC-2010Plus (SHIMADSU Corporation, Kyoto, Japan) equipped with a flame ionisation detector. Operating conditions were as follows: the oven temperature was 50 °C for 0.5 min, and then was raised to 260 °C over 25 min and held for 5 min. Injector temperature was 240 °C, the detector temperature was 280 °C, and helium as the carrier gas was delivered at 1.09 ml/min. The identification of components was based on a comparison of retention times with those of standards (Sigma-Aldrich Japan, Inc., Tokyo, Japan; Nu-Chek Prep, Inc., MN, USA). The concentration of each sample was calculated from the internal standard ratio of the standard.
Variables
The following fatty acids were examined: SFAs [lauric acid (LaA; C12:0), myristic acid (MyA; C14:0), palmitic acid (PA; C16:0), stearic acid (StA; C18:0)], an n-9 MUFA [oleic acid (OlA; C18:1)], n-6 PUFAs [linoleic acid (LiA; C18:2), di-homo-gamma-linolenic acid (DGLA; C20:3), and arachidonic acid (AA; C20:4)] and n-3 PUFAs [alpha-linolenic acid (AlA; C18:3), eicosapentaenoic acid (EPA; C20:5), and docosahexaenoic acid (DHA; C22:6)]. Low-density lipoprotein (LDL)-cholesterol (LDL-C) was calculated using the Friedewald formula as follows: LDL-C = T-CHO − HDL-C − TG/5. Mean blood pressure (MBP) was calculated using the following formula: DBP + (SBP − DBP) / 3.
Evaluation
We evaluated concentrations of s-LPs, concentrations of s-FAs and compositions created against total fatty acids of s-FAs (in weight percent; %), and correlation coefficients of s-FA concentrations and compositions with age and s-LPs. We divided age into three groups, specifically 50–64 years as working-age after menopause in females, 65–79 years as probable life expectancy after retirement, and 80 years or older as the oldest age. We also compared concentrations and compositions (%) of s-FAs between age groups and between AIS subtypes of large-artery atherosclerosis (LAA), small-vessel occlusion (SVO; lacunar stroke), cardioembolic (CE) stroke, TIA, and patients for whom AIS subtype was not determined [8].
Statistical analysis
Normally distributed continuous variables are expressed as means ± standard deviations (SDs) and an unpaired Student’s t-test or analysis of variance (ANOVA) was used to compare unpaired groups. Non-normally distributed continuous variables were expressed as medians and interquartile ranges (IQRs), and a Wilcoxon rank-sum test was used to compare unpaired groups. A multiple comparison test was used to compare all possible pairs among three groups. The Pearson correlation coefficient (r) was used to measure the strength of the linear relationship between normally distributed variables, and the Spearman rank correlation coefficient (rs) was used to measure the strength of the relationship between non-normally distributed variables. We defined 0 ≤ |r| < 0.3 or 0 ≤ |rs| < 0.3 as no correlation, 0.3 ≤ |r| < 0.5 or 0.3 ≤ |rs| < 0.5 as a weak correlation, 0.5 ≤ |r| < 0.7 or 0.5 ≤ |rs| < 0.7 as a moderate correlation, and 0.7 ≤ |r| < 0.9 or 0.7 ≤ |rs| < 0.9 as a strong correlation. Logistic regression was used to estimate odds ratios (OR) and 95% confidence intervals (CIs) for ischaemic stroke in LAA or SVO groups. A probability (p) value less than 0.05 was considered statistically significant. We used the JMP software program (version 15.0; SAS Institute, Cary, NC, USA) to perform statistical analyses.
Results
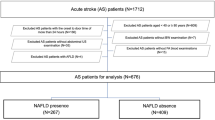
A total of 463 patients with ischaemic stroke were admitted to our stroke centre during the study period. Among them, 129 patients were excluded from our analysis because of a pre-hospital mRS scores of 3 or more, 37 were excluded with a BMI less than 18.5, 57 were excluded because they did not undergo s-FA analysis at admission, and 49 were excluded for using medication for dyslipidaemia. Finally, 191 patients met our inclusion criteria (Table 1). All patients were of East Asian ethnicity and were most likely of Japanese ancestry. Regarding stroke subtype, 52 (27.2%) patients experienced LAA, 50 patients experienced SVO (lacunar stroke), 50 patients (26.2%) experienced CE stroke, five patients (2.6%) experienced TIA, and for 34 (17.8%) patients, the subtype was not determined. BMI was lower in females, concentrations of T-CHO, LDL-C, and HDL-C were higher in females, and levels of DGLA, AA, and DHA were also higher in females (Table 2).
Patients with LAA or SVO (LAA_SVO) ischaemic stroke subtypes due to arteriosclerosis were younger and had higher concentrations of T-CHO, LDL-C, TG, PA, StA, OlA, LiA, DGLA, and AA than patients with an ischaemic stroke subtype of CE or others (CE_O). However, there were no differences in BMI, sex, AlA, EPA, and DHA concentrations and no differences in s-FAs compositions, except for that of DGLA, between LAA_SVO and CE_O groups (Table 2).
Serum T-CHO and TG were weakly negatively correlated with age (Table 3). Serum concentrations of PA, StA, OlA, LiA, DGLA, AA, and AlA were weakly negatively correlated with age and compositions of SFAs, LiA, AA, and AlA were not correlated with age. Compositions of OlA and DGLA and the EPA/AA ratio were weakly negatively correlated with age. Compositions of EPA and DHA and the n-6/n-3 ratio were weakly positively correlated with age. Most s-FA concentrations were weakly negatively correlated with age, and most s-FA compositions had no correlations with age in our patients (Table 3). Serum concentrations of StA, LiA, and AA showed positive correlations with T-CHO, concentrations of SFAs, LiA, and AlA were positively correlated with TG, and the concentration of OlA was strongly correlated with TG (rs = 0.7661). In contrast, no serum FA concentrations exhibited correlations with LDL-C or HDL-C (Table 3). Further, compositions of MyA and OlA showed positive correlations with TG, whereas no serum FA compositions were correlated with LDL-C or HDL-C (Table 3).
Patients aged 50–64 years had the highest concentrations of TG, PA, StA, OlA, LiA, DGLA, and AA among the three age groups, and patients aged 80 years or older had the highest compositions of EPA (2.47%) and DHA (5.14%) (Table 4). Twenty-five (78.1%) of 32 patients aged 50–64 years suffered from LAA_SVO and these 25 patients had higher concentrations of TG (MD, IQR: 173, 104–223 mg/dl), PA (777.8, 704.5–960.5 μg/ml), StA (229.4, 208.6–280.05 μg/ml), OlA (742.5, 637.45–865.85 μg/ml), LiA (896.8, 806.4–1007.75 μg/ml), DGLA (36.8, 28.9–48.35 μg/ml), and AA (172.4, 146.4–204.5 μg/ml) than the seven patients with CE_O; however, there were no differences in the compositions of EPA and DHA or the EPA/AA and n-6/n-3 ratios between LAA_SVO and CE_O groups among the 68 patients aged 80 or older (Table 5). These oldest 68 patients had the highest compositions of EPA and DHA; however, there were no differences in such compositions between LAA_SVO and CE_O groups (Table 5). With adjustments for age, TCHO, and TG by logistic regression analysis, AA (OR = 1.011, 95% CI, 0.999–1.012), DGLA (OR = 1.042, 95% CI, 0.998–1.089), and T-CHO (OR = 1.011, 95% CI, 0.999–1.024) were weakly associated with LAA_SVO, rather than CEO_O, although TG (OR = 1.013, 95% CI, 1.003–1.024) and age (OR = 0.961, 95% CI, 0.927–0.993) were associated with LAA_SVO, rather than CEO_O.
Discussion
Our results of elderly AIS patients demonstrated that concentrations, but not compositions, of PA, OlA, and LiA are significantly correlated with age, TG, and ischaemic stroke subtypes. Patients with LAA_SVO were younger and had higher concentrations of T-CHO, TG, PA, StA, OlA, LiA, DGLA, and AA among patients aged 50 years or older, whereas there were no differences in the compositions of s-FAs, except for that of DGLA, between LAA_SVO and CE_O groups. Although no fatty acid concentrations were significant independent predictors of LAA_SVO, as compared to the predictive power of CE_O, AA and DGLA concentrations had a weak association with LAA_SVO rather than CE_O. Compositions of EPA and DHA were not related to ischaemic stroke subtype but rather were associated with age at onset.
A previous study reported that TG concentration had a stronger relationship with n-6 PUFA than T-CHO concentration in healthy Japanese individuals with normal serum T-CHO and TG levels, and that correlation coefficient between TG and n-6 PUFA was negative, specifically, − 0.417 in men and − 0.330 in women [1]. In our elderly patients, the Spearman rank correlation coefficient comparing TG and LiA was positive, specifically 0.5088 at AIS onset. Correlations between TG and n-6 PUFA were quite different between young, healthy individuals. and elderly patients at AIS onset. A previous study reported that serum palmitic and oleic acid were associated with an increased incidence of incidental atherothrombotic, lacunar, and ischemic strokes of undetermined cause compared to that with matched controls, and that DHA and arachidonic acid were associated with a decreased incidence of ischaemic stroke [9]. However, that was a case-control study in which fasting blood samples were collected from all observational study participants, and their values of serum fatty acids were not reported at AIS onset [9]. Concentrations of PA, StA, and OlA were higher in the LAA_SVO group than in the CE_O group in our elderly AIS patient cohort, although patients with CE_O were not the matched controls but were ischaemic stroke patients.
A previous study reported that higher concentrations of serum n-6 PUFAs and lower levels of MUFAs are strongly associated with lower TG levels [4]. However, in our study, higher concentrations of n-6 PUFAs were associated with higher TG levels. A previous study also reported that mean compositions of PA, OlA, LiA, EPA, and DHA in healthy Japanese male subjects aged 50 to 59 years were 25, 21.3, 27.3, 2.4, and 4.0%, respectively [1], which were almost the same as those in our male patients (Table 2). A previous study reported that the mean concentration of LiA was 2233.8 μmol/L (626.5 μg/ml) in healthy young adults in their 20s [10], which was almost the same as the concentration detected in our patients. In contrast, a previous study reported that in US patients with CAD at an average age of 47 ± 5 years, the mean concentrations of PA, StA, OlA, LiA, DGLA, AA, EPA, and DHA were 823, 13, 1336, 4358, 33, 688, 67, and 40 μg/ml, respectively, and the mean compositions of PA, StA, OlA, LiA, DGLA, AA, EPA, and DHA were 11.3, 0.2, 18.4, 58.6, 0.4, 9.4, 0.9, and 0.5%, respectively [6]. Their concentrations of OlA, LiA, and AA and compositions of LiA and AA were much higher, but compositions of OlA, EPA, and DHA were much lower, than those in our patients (Table 1). Compared to those in our patients, concentrations of 4358 μg/ml of LiA and 688 μg/ml of AA were extremely high, and in that previous study, atherosclerotic CAD typically occurred in patients in their 40s. Our patients with LAA_SVO due to arteriosclerosis were younger among the cohort, and they also had higher concentrations of LiA and AA. Even though the concentration of a fatty acids might be high, its proportion could be low because the proportion is relative. If the concentration of one variable increases, the composition of the other variables has to decrease. Composition, therefore, is not appropriate to identify driving factors. Further, serum concentrations of fatty acids can be more easily interpreted in metabolic and therapeutic terms, as reported previously. Our study was retrospective and cross-sectional, and there was no control group. Therefore, it was not determined whether s-FA concentrations in patients with LAA_SVO were high or whether compositions of EPA and DHA were high or low, compared to those in hypothetical control subjects.
Previous studies have reported that n-3 PUFA might reduce the incidence of CAD or stroke or the mortality associated with cardiovascular disease [11,12,13,14,15]. The administration of highly-purified EPA appeared to reduce the risk of recurrent stroke in a Japanese population of hypercholesterolemic patients receiving low-dose statin therapy [13]. In contrast, SFAs might increase the risk factors associated with these conditions [16]. A fish diet decreases very-low-density lipoprotein (VLDL) but increases both low-density lipoprotein (LDL) and high-density lipoprotein (HDL) in healthy human subjects [3]. Further, dietary SFAs were found to increase serum T-CHO, and it was shown that dietary n-6 PUFAs lower serum T-CHO [17, 18]. LiA-rich food can also lower T-CHO [5]. However, in our patients, the concentration of LiA was strongly positively correlated with T-CHO and TG levels. Dietary fatty acids with lower amounts of PA, StA, OlA, and n-6 PUFAs and higher compositions of EPA and DHA might also reduce the incidence of ischaemic stroke associated with LAA_SVO and in the oldest age group, although the appropriate dietary intake of fatty acids to prevent ischaemic stroke cannot be confirmed based on the results of our study. Serum fatty acids at AIS onset are significantly influenced by recent dietary intake, and it is important to assess what types and quantities of meats and fish were consumed and what kind and volume of vegetable oils were used a few days before AIS onset. The assessment of dietary intake might lead to a recommendation for the appropriate dietary intake of fatty acids to prevent ischaemic stroke. If the appropriate intake of fatty acids is identified, a prospective randomised control study is required to address this.
Conclusions
In AIS elderly patients, concentrations, rather than compositions, of PA, OlA, and LiA correlated with age, TG, and ischaemic stroke subtype. Further, patients with LAA_SVO were younger and had higher concentrations of PA, OlA, and LiA than those with CE_O, although serum fatty acids were not independent predictors of LAA_SVO, as compared to the predictive power of CE_O. There were no differences in s-FA compositions between LAA_SVO and CE_O groups. Higher compositions of EPA and DHA were associated with the oldest age. Further studies are warranted to determine the appropriate dietary intake of fatty acids for AIS prevention and long life.
Availability of data and materials
Raw data can be made available upon request to the corresponding author.
Abbreviations
- AA:
-
Arachidonic acid
- AIA:
-
Alpha-linolenic acid
- BMI:
-
Body mass index
- CAD:
-
Coronary artery disease
- CE:
-
Cardioembolic stroke
- DBP:
-
Diastolic blood pressure
- DGLA:
-
Di-homo-gamma-linolenic acid
- DHA:
-
Docosahexaenoic acid
- EPA:
-
Eicosapentaenoic acid
- FA:
-
Fatty acid
- HDL-C:
-
High-density lipoprotein cholesterol
- LAA:
-
Large-artery atherosclerosis
- LaA:
-
Lauric acid
- LDL-C:
-
Low-density lipoprotein cholesterol
- LiA:
-
Linoleic acid
- MBP:
-
Mean blood pressure
- mRS:
-
Modified Rankin scale
- MyA:
-
Myristic acid
- n-3 PUFA:
-
N-3 polyunsaturated fatty acid
- n-6 PUFA:
-
N-6 polyunsaturated fatty acid
- n-9 MUFA:
-
N-9 monounsaturated fatty acid
- OlA:
-
Oleic acid
- PA:
-
Palmitic acid
- SBP:
-
Systolic blood pressure
- SFA:
-
Saturated fatty acid
- s-FA:
-
Serum fatty acid
- s-LP:
-
Serum lipids
- StA:
-
Stearic acids
- SVO:
-
Small-vessel occlusion (lacunar stroke)
- T-CHO:
-
Total cholesterol
- TG:
-
Triglycerides
- TIA:
-
Transient ischaemic attack
- VLDL:
-
Very-low-density-lipoprotein
References
Takita T, Nakamura K, Kimira M, Yamada N, Kobayashi Y, Innami S. Serum fatty acid compositions and lipid concentrations and their correlations. J Clin Biochem Nutr. 1996;20:149–59.
Lohnera S, Feketeb K, Marosvolgyi T, Decsia T. Gender differences in the long-chain polyunsaturated fatty acid status: systematic review of 51 publications. Ann Nutr Metab. 2013;62:98–112.
von Lossonczy TO, Ruiter A, Bronsgeest-Schoute HC, van Gent CM, Hermus RJ. The effect of a fish diet on serum lipids in healthy human subjects. Am J Clin Nutr. 1978;31:1340–6.
Jelenkovic A, Bogl LH, Rose RJ, Kangas AJ, Soininen P, Ala-Korpela M, et al. Association between serum fatty acids and lipoprotein subclass profile in healthy young adults: exploring common genetic and environmental factors. Atherosclerosis. 2014;233:394–402.
Rassias G, Kestin M, Nestel PJ. Linoleic acid lowers LDL cholesterol without a proportionate displacement of saturated fatty acid. Eur J Clin Nutr. 1991;45:315–20.
Schwertner HA, Mosser EL. Comparison of lipid fatty acids on a concentration basis vs weight percentage basis in patients with and without coronary artery disease or diabetes. Clin Chem. 1993;39:659–63.
Mori T, Tanno Y, Kasakura S, Yoshioka K, Nakai N. Serum fatty acids and ischemic stroke subtypes in middle- and late-onset acute stroke patients. Clin Nutr Exp. 2018;22:19–29.
Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of org 10172 in acute stroke treatment. Stroke. 1993;24:35–41.
Yaemsiri S, Sen S, Tinker LF, Robinson WR, Evans RW, Rosamond W, et al. Serum fatty acids and incidence of ischemic stroke among postmenopausal women. Stroke. 2013;44:2710–7.
Abdelmagid SA, Clarke SE, Nielsen DE, Badawi A, El-Sohemy A, Mutch DM, et al. Comprehensive profiling of plasma fatty acid concentrations in young healthy Canadian adults. PLoS One. 2015;10:e0116195.
Dyerberg J, Bang HO. A hypothesis on the development of acute myocardial infarction in Greenlanders. Scand J Clin Lab Invest Suppl. 1982;161:7–13.
Kromhout D, Bosschieter EB, de Lezenne Coulander C. The inverse relation between fish consumption and 20-year mortality from coronary heart disease. N Engl J Med. 1985;312:1205–9.
Tanaka K, Ishikawa Y, Yokoyama M, Origasa H, Matsuzaki M, Saito Y, et al. Reduction in the recurrence of stroke by eicosapentaenoic acid for hypercholesterolemic patients: subanalysis of the JELIS trial. Stroke. 2008;39:2052–8.
Miyagawa N, Miura K, Okuda N, Kadowaki T, Takashima N, Nagasawa SY, et al. Long-chain n-3 polyunsaturated fatty acids intake and cardiovascular disease mortality risk in Japanese: a 24-year follow-up of NIPPON DATA80. Atherosclerosis. 2014;232:384–9.
Morise A, Serougne C, Gripois D, Blouquit MF, Lutton C, Hermier D. Effects of dietary alpha linolenic acid on cholesterol metabolism in male and female hamsters of the LPN strain. J Nutr Biochem. 2004;15:51–61.
Sacks FM, Lichtenstein AH, Wu JHY, Appel LJ, Creager MA, Kris-Etherton PM, et al. Dietary fats and cardiovascular disease: a presidential advisory from the American Heart Association. Circulation. 2017;136:e1–23.
Hegsted DM, Ausman LM, Johnson JA, Dallal GE. Dietary fat and serum lipids: an evaluation of the experimental data. Am J Clin Nutr. 1993;57:875–83.
Fernandez M, West K. Mechanisms by which dietary fatty acids modulate plasma lipids. J Nutr. 2005;135:2075–8.
Acknowledgements
The authors wish to thank Miss Nozomi Chiba, BA, for her secretarial support.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
Takahisa Mori, MD, had full access to all data in the study and takes responsibility for the integrity of the data and the accuracy of data analysis. TM contributed to the study concept and design. TM and KY acquired the data. TM interpreted the data and performed the statistical analysis. TM drafted the manuscript. TM critically revised the manuscript for valuable intellectual content. TM and KY provided final approval of the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in the study were in accordance with the ethical standards of the institution (Shonan Kamakura General Hospital) and with the 1964 Helsinki Declaration. The institutional (Shonan Kamakura General Hospital) ethics committee approved access to medical records for our retrospective analysis. Informed consent was not required because of routine medical care, the retrospective design, and the anonymisation of patient identifiers.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mori, T., Yoshioka, K. Features of serum fatty acids in acute ischaemic stroke patients aged 50 years or older. BMC Cardiovasc Disord 20, 122 (2020). https://doi.org/10.1186/s12872-020-01408-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-020-01408-1