Abstract
Background
The study was undertaken to assess the incidence of lower urinary tract symptoms (LUTS) after short-term indwelling urethral catheter (IUC) in polytrauma patients admitted to a level one trauma unit using core lower urinary tract symptom score (CLSS). Data of patients admitted between January 2013 and December 2015 and meeting the study criteria were retrieved from the hospital informatics system. Chart review was done, and patients were subsequently interviewed telephonically.
Results
Ninety-four respondents comprising of 81.9% males and 18.1% females out of the 221 eligible patients were contacted. The most common LUTS reported was urethral pain, and 90% had mild to moderate symptoms. No severe LUTS were identified. There was a positive correlation between the duration of IUC and LUTS, but there was no statistically significant association between age and LUTS in our study population.
Conclusion
Short-term duration of IUC in the trauma ICU patient is associated with predominantly mild irritative LUTS which are mostly self-limiting and may not need further investigations and management. CLSS was found to be a useful screening tool. Further studies are needed to confirm findings in our study.
Similar content being viewed by others
1 Background
Since the invention in the 1930s, Foley’s catheter has gained universal usage as demonstrated by the fact that between 16 and 25% of hospitalised patients have an indwelling urethral catheter (IUC) inserted during their hospital stay [1]. The use of a urethral catheter is associated with numerous complications, both infectious and non-infectious [2] all of which present with lower urinary tract symptoms and an associated decrease in the quality of life. Catheter-associated urinary tract infection (CAUTI) has received much clinical significance as the commonest complication of urinary catheterisation, as well as the most common cause of infections in hospitals and other health care facilities [3], especially in post-surgical patients, while iatrogenic trauma from poor technique of placement is also common as a reason for litigation [4].
Non-infectious complications of IUC such as bleeding, urethritis, urethrocutaneous fistula, bladder neck incompetence, sphincter erosion, bladder calculi, bladder cancer and allergy (Latex), encrustation and deterioration of upper tract due to obstruction have also been documented [5, 6].
Injury remains a leading cause of morbidity and mortality around the world, and trauma systems have been shown to improve outcomes for severely injured patients [7]. Trauma patients represent a unique patient population due to the sudden derangement of organ function. Eight-six per cent of trauma admissions in one study were diagnosed with organ dysfunction (systemic inflammatory response syndrome at the time of admission) [8]. This in addition to other procedures, such as intubation and the presence of IUC increases susceptibility to both infectious and non-infectious complications.
There is a paucity of information in the literature on complications of post-urethral catheterisation in the trauma population, in patients presenting without any prior injury to the lower urinary tract (LUT). In the present study, we investigated the incidence of lower urinary tract symptoms (LUTS) in trauma patients admitted to a level one trauma unit ICU after IUC using the core lower urinary tract symptom score (CLSS).
2 Methods
The study was approved by the Biomedical Research Ethics Committee (BREC) of the author’s institution (BE 263/15), as well as the Provincial Health Research Committee of the Department of Health. A urinary catheter may be in situ for a short term (1–14 days), medium term (2–6 weeks) or medium to long term (6 weeks–3 months), and it may be inserted via either the transurethral or the suprapubic route [9]. Trauma ICU patients are routinely managed with a TUC, unless requiring a suprapubic catheter.
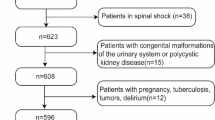
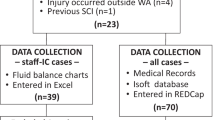
The study included contactable respondents who were admitted into the trauma intensive care unit between January 2013 and December 2015 and had an indwelling TUC. Chart review of patients meeting the inclusion criteria was performed using the Sorian® (Siemens, Germany) and Meditech™ (Meditech, Boston MA) hospital information system (BREC Class Approval BE207-09). Sample determination: All patients in the trauma ICU registry meeting inclusion criteria were eligible for attempted telephonic follow-up.
Contactable consecutive patients meeting the above criteria were subsequently interviewed telephonically using the CLSS questionnaire (“Appendix” section). Patients aged more than 40 years were excluded from the study due to potential age-related effect on LUTS.
The unit operates a strict IUC protocol. An all-silicone catheter is inserted by the on-call registrar at admission and it is changed every 4 weeks or earlier, should there be an indication, such as CAUTI. CAUTI has been found to be lower when there is a routine change of catheter [10]. Further exclusion criteria included accidental IUC removal, patients who had suprapubic catheters as well as permanent IUC. Prior to commencing the study arrangement was made with the Urology Department for referral for further evaluation of any patients who were identified with bothersome LUTS at the telephonic follow-up part of the study.
Definitions of various aspects of LUTS used in the study were based on the international continence society definitions of LUTS [11].
3 Results
Of the 221 patients eligible for the study, 94 (42.5%) were successfully contacted. One hundred and twenty-seven patients could not be included in the study due to incomplete data entry during the admission process, wrong telephone numbers, persistent voicemail and refusal to participate in the study. Only one patient declined consent. There were 77 males (89.1%) and 17 females (18.1%) included in the follow-up study. The mean age was 29.11 years (SD 6.029), and the mean duration of ICU was 15.80 days (SD 13.37). Descriptive analysis of results is given in Table 1. The mean CLSS for the study was 3.52 (SD 1.46).
The most common symptom identified in the post-IUC group was urethral pain, which was reported by almost 90% of the respondents. Urethral pain was described as pain and discomfort on micturition by respondents. Urgency was also reported by about 80% of the respondents, and another 74.5% reported some form of frequency. The trend was similar to nocturia where 20.2% reported mild symptoms and only 1.1% had moderate symptoms. Most respondents attributed both frequency and nocturia to their fluid intake as a self-reported reason for these symptoms.
Although approximately 80% reported some form of urgency, only 25% of the respondents reported associated mild urge incontinence (UI), whereas 1% reported moderate UI. On the other hand, only 3.2% reported rarely experiencing stress incontinence and another 7.4% also complained of occasional poor stream. Both types of incontinence were more common in the female sex. When compared to the number of participants that reported the presence of urethral pain, only 30.1% complained of mild bladder pain or discomfort (Table 2).
The majority of the symptoms were transient and had resolved at the time of the study mostly lasting for up to 10–14 days post-hospital discharge. One respondent had a further evaluation of the LUTS by way of urine culture and sensitivity and was prescribed a course of antibiotics for suspected UTI at his local hospital. No further intervention was carried out.
The Chi-squared test was used to determine the age effect on LUTS presentation in the study, but no significant association was identified; however, the Pearson test showed a positive correlation (0.375) between the duration of IUC and the presence of LUTS.
Aside from urethral pain, the rest of the voiding LUTS were minimally reported in the study. Respondents who experienced mild straining and poor stream were 2.1% and 7.4%, respectively, but they had partly attributed their symptoms to the urethral pain. A further 19.1% also reported a sensation of incomplete emptying, which in some cases was difficult to differentiate from bladder pain. Some respondents explained this as possibly due to their initial injury, especially in the case of those with injury to the abdomen.
The majority of the respondents (76.6%) in our study were pleased with their QOL as far as their LUTS were concerned after a short-term IUC, 12.8% mostly satisfied and a further 8.5% were delighted.
4 Discussion
This study highlights the incidence of LUTS after a short-term IUC in the trauma population admitted to an ICU, of which the most predominant symptoms were urethral pain (dysuria) and urgency.
LUTS is assessed using standardised questionnaires such as International Prostate Symptom Score (IPSS), Overactive Bladder Symptom Score (OABSS), Quality of Life (QOL) index, the International Continence Society (ICS)-male and the short form of the ICS-male, among others [12, 13]. This, however, does not cover all aspects of LUTS because of the disease-specific nature of these questionnaires and as such does not make it an appropriate screening tool for LUTS [12,13,14]. The core lower urinary tract symptom score (CLSS) questionnaire was developed by Homma et al. to address these challenges. It addresses 10 important symptoms selected from 25 symptoms defined by the ICS standardization committee [12, 15]. Its validity and reproducibility have been confirmed in studies, and it is an appropriate initial assessment tool for LUTS [12]. CLSS compared to IPSS and other standardised questionnaires was found to be more comprehensive [14].
In the general population, voiding symptoms are more common in men, whereas storage symptoms are more common in women, but the prevalence of LUTS does not differ by race [16]. LUTS is also more common in the older adult population [16]. The age groups between 18 and 29 years formed almost 50% of the study population, as seen in other studies and sex difference also demonstrated a male dominance [17]. However, sex alone may not fully determine the severity of LUTS post-discharge from ICU. Other factors such as injury severity score and complications like critical illness neuropathy and myopathy, or pelvic pain from pelvic fracture, diabetes mellitus, and also human immune virus infection may all have an impact on LUT functions [18, 19]. These were unaccounted for in this study. There was no significant statistical association between age and the presence of LUTS in our study; however, one previous study found a prevalence of 61.4% LUTS among adult population 18 years and above, but this study and other similar studies included elderly participants above 40 years and LUTS was also found to increase with ageing [11, 20, 21]. In the trauma patient population, the commonest LUTS from our study was urethral pain (dysuria). This in contrast to other studies in a different patient population found urethral pain only in one-fifth of study population [14]. Pain and other irritative symptoms such as frequency, nocturia, urgency and urge incontinence are usually due to up regulation of C unmyelinated fibres as a result of an inflammatory response to the presence of IUC and other noxious stimuli such as infection [22,23,24]. It is unclear whether the physiological changes seen in trauma patients have a negative impact on the functional integrity of the urothelium. Considering the physiological derangement associated with trauma, one would have anticipated a higher number of LUTS reported in the trauma population, but our results showed otherwise. Female participants were more likely to present with associated urge incontinence than their male counterparts. The reasons for this observation may not be readily evident from our study; however, in another study, 45% of healthy female volunteers were excluded from a study due to some degree of urinary incontinence [24]. In a systematic review and meta-analysis to determine the frequency of non-infectious complications of IUC, the incidence of urethral stricture or erosion after short-term IUC was 3.4% [25]. The current study revealed a very low incidence of obstructive LUTS.
Prolonged duration of IUC is associated with an increased incidence of LUTS as evident in other studies [26, 27]. The adherence to urinary catheter policies, on the other hand, is shown to be associated with a decrease in complications as a result of a decrease in IUC duration [28,29,30].
It is unclear the impact of these early symptoms on the development of LUTS later on in life as the individual advances in age. This is a subject for further research. The frequency of change of IUC is also a subject of debate but the authors institution performs IUC change every 4 weeks or earlier when there is an indication, such as UTI being diagnosed.
5 Limitations
This study is limited by sample size and the single-centre nature of the study. The retrospective telephonic follow-up can be associated with recall bias and subjectivity, whereas a self-administered questionnaire may have been more reliable, albeit not practical in the local environment. In addition, some complications may not have yet become apparent in the brief follow-up period and may have been missed in this study. One such potential complication is CAUTI, occurring post-ICU discharge; however, routine urine cultures of all IUC patients are taken weekly in the ICU as part of screening for sepsis and the published CAUTI rate in the unit is low [31]. The CLSS fails to address the new concept of LUTS; post-micturition LUTS, which is the third category of LUTS along storage and voiding LUTS.
6 Conclusion
Despite the limitations of our study, LUTS post-ICU-admission in trauma patients admitted to a dedicated trauma ICU are predominantly mild without significant bother and may not need further follow-up. The CLSS is a valid option for evaluation of LUTS but further prospective multi-institutional studies are needed to determine the true burden of LUTS in these patients and other patients populations.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- BREC:
-
Biomedical Research Ethics Committee
- CAUTI:
-
catheter-associated urinary tract infection
- CLSS:
-
core lower urinary tract symptom score
- FC:
-
foleys catheter
- IALCH:
-
Inkosi Albert Luthuli Central Hospital
- IUC:
-
indwelling urethral catheter
- ICU:
-
intensive care unit
- LUT:
-
lower urinary tract
- TICU:
-
trauma intensive care unit
- TUC:
-
transurethral catheter
- UC:
-
urethral catheterisation
References
Parvey HR, Patel BK (1998) Urethral complications of urinary catheterization presenting as primary scrotal masses: sonographic diagnosis. J Clin Ultrasound 26:261–264
Sekhavat L, Farajkhoda T, Davar R (2008) The effect of early removal of indwelling urinary catheter on postoperative urinary complications in anterior colporrhaphy surgery. Aust N Z J Obstet Gynaecol 48:348–352
Igawa Y, Wyndaele J-J, Nishizawa O (2008) Catheterization: possible complications and their prevention and treatment. Int J Urol 15:481–485
Awad MA, Osterberg EC, Chang H et al (2016) Urethral catheters and medical malpractice: a legal database review from 1965 to 2015. Transl Androl Urol 5(5):762–773
Cassani R (2014) Promoting intermittent self-catheterisation to encourage self-care in district nursing patients. Br J Commun Nurs 19:177–181
Madigan E, Neff DF (2003) Care of patients with long-term indwelling urinary catheters. Online J Issues Nurs 8:130–141
Hardcastle T, Reeds M, Muckart D (2013) Utilisation of a level 1 Trauma Centre in KwaZulu-Natal: appropriateness of referral determines trauma patient access. World J Surg 37:1544–1549
Sakamoto Y, Mashiko K, Matsumoto H et al (2010) Systemic inflammatory response syndrome score at admission predicts injury severity, organ damage and serum neutrophil elastase production in trauma patients. J Nippon Med Sch 77:138–144
Savage AR (2014) Evidence-based practice in relation to indwelling urinary catheters. Afr Health 36:25–28
Feneley RCL, Kunin CM, Stickler DJ (2012) An indwelling urinary catheter for the 21st century. BJU Int 109:1746–1749
Abrams P, Cardozo L, Fall M et al (2003) The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology 61:37–49
Ito H, Sano F, Ogawa T et al (2014) Evaluation and validation of the Core Lower Urinary Tract Symptom Score as an outcome assessment tool for the treatment of benign prostatic hyperplasia: effects of the α1-adrenoreceptor antagonist silodosin. Int J Urol 21:108–112
Donovan, Brookes, La Rosette De et al (1999) The responsiveness of the ICSmale questionnaire to outcome: evidence from the ICS-‘BPH’ study. BJU Int 83:243–248
Fujimura T, Kume H, Nishimatsu H et al (2012) Assessment of lower urinary tract symptoms in men by international prostate symptom score and core lower urinary tract symptom score. BJU Int 109:1512–1516
Homma Y, Yoshida M, Yamanishi T et al (2008) Core Lower Urinary Tract Symptom Score (CLSS) questionnaire: a reliable tool in the overall assessment of lower urinary tract symptoms. Int J Urol 15:816–820
Llorente C (2010) New concepts in epidemiology of lower urinary tract symptoms in men. Eur Urol Suppl 9:477–481
Dinh MM, Russell SB, Bein KJ et al (2016) Age-related trends in injury and injury severity presenting to emergency departments in New South Wales Australia: implications for major injury surveillance and trauma systems. Injury 48:171–176
Apostolakis E, Papakonstantinou N, Baikoussis N et al (2015) Intensive care unit-related generalized neuromuscular weakness due to critical illness polyneuropathy/myopathy in critically ill patients. J Anesth 29:112–121
Lee Y-S, Lee K-S, Jung J et al (2011) Prevalence of overactive bladder, urinary incontinence, and lower urinary tract symptoms: results of Korean EPIC study. World J Urol 29:185–190
Tuncay Aki F, Aygun CEM, Bilir N et al (2003) Prevalence of lower urinary tract symptoms in a community-based survey of men in Turkey. Int J Urol 10:364–370
De Groat WC (2006) Integrative control of the lower urinary tract: preclinical perspective. Br J Pharmacol 147:S25–S40
Birder L, de Groat W, Mills I et al (2010) Neural control of the lower urinary tract: peripheral and spinal mechanisms. Neurourol Urodyn 29:128–139
Delnay KM, Stonehill WH, Goldman H et al (1999) Bladder histological changes associated with chronic indwelling urinary catheter. J Urol 61:1106–1109
Pauwels E, De Wachter S, Wyndaele JJ (2004) Normality of bladder filling studied in symptom-free middle-aged women. J Urol 171:1567–1570
Hollingsworth JM, Rogers MAM, Krein SL et al (2013) Determining the non infectious complication of indwelling urethral catheters: a systematic review and meta analysis. Ann Intern Med 159:401–410
Hu Y, Craig SJ, Rowlingson JC et al (2014) Early removal of urinary catheter after surgery requiring thoracic epidural: a prospective trial. J Cardiothorac Vasc Anesth 28:1302–1306
Pratt R, Pellowe C (2010) Good practice in management of patients with urethral catheters. Nurs Older People 22:25–29
Gotelli JM, Merryman P, Carr C et al (2008) A quality improvement project to reduce the complications associated with indwelling urinary catheters. Urol Nurs 28:465–473
Knoll BM, Wright D, Ellingson L et al (2011) Reduction of inappropriate urinary catheter use at a veterans affairs hospital through a multifaceted quality improvement project. Clin Infect Dis 52:1283–1290
Palka MA (2014) Evidenced based review of recommendations addressing the frequency of changing long-term indwelling urinary catheters in older adults. Geriatr Nurs 35:357–363
Ramsamy Y, Muckart DJJ, Han KSS (2013) Microbiological surveillance and antimicrobial stewardship minimise the need for ultrabroad-spectrum combination therapy for treatment of nosocomial infections in a trauma intensive care unit: an audit of an evidence-based empiric antimicrobial policy. S Afr Med J 103(6):371–376
Acknowledgements
The authors acknowledge the management of Inkosi Albert Luthuli Central Hospital who gave permission for the study to be carried out after BREC approval and also assisted in providing a direct telephone line for the telephonic follow-up interview. We further acknowledge all the respondents who voluntarily accepted to be part of the study.
Funding
None.
Author information
Authors and Affiliations
Contributions
EOS (corresponding author): Had complete access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: EOS, TCH and RS. Acquisition of data: EOS and TCH. Analysis and interpretation of data: BT. Drafting of the manuscript: EOS, TCH and RS. Critical revision of the manuscript for important intellectual: TCH and RS. Content: EOS, TCH, RS and BT. Statistical analysis: BT. Study supervision: TCH and RS. The manuscript was read, and its contents approved by all authors prior to submission.
Corresponding author
Ethics declarations
Competing interest
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was approved by the Biomedical Research Ethics Committee of University of Kwazulu Natal, South Africa, on the 1st September 2015 with a reference; BE263/16. The Committee was chaired by Prof Tsoka-Gwegweni.
Informed consent
An informed consent was obtained from all participants prior to participation in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix

Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Owusu Sekyere, E., Hardcastle, T.C., Sathiram, R. et al. Overview of lower urinary tract symptoms post-trauma intensive care unit admission. Afr J Urol 26, 19 (2020). https://doi.org/10.1186/s12301-020-00027-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-020-00027-8