Abstract
Background
Hereditary diffuse gastric cancer (HDGC) is a hereditary autosomal inherited syndrome associated with CDH1 germline mutations. In Brazil, gastrointestinal tumors are among the most prevalent tumor types and constitute a serious public health problem, especially in the northern and northeastern regions. This study aimed to investigate germline mutations, methylation pattern and genomic rearrangements in the CDH1 gene and quantitative changes in the DNA of HDGC patients in northern and northeastern Brazil.
Methods
Twenty-seven DNA samples from the members of four families affected by HDGC were analyzed using array comparative genomic hybridization (aCGH), DNA sequencing and methylation pattern.
Results
No evidence of gain and loss events or any rearrangements were found in any of the samples tested using aCGH. No promoter region hypermethylation was observed either. Two of the four families presented different types of germline mutations. The 185G > T and 1018A > G germline mutations detected in this study have been described in Asian and European families, respectively. The ancestors of the two families carrying these mutations had originated from those continents.
Conclusion
This is the first study to evaluate CDH1 gene germline mutations in Brazilian families with HDGC. In our study, 50% of the families showed no CDH1 gene alterations, and it is possible that in regions with a high incidence of gastric cancer, such as northern and northeastern Brazil, environmental factors might have induced the different genetic alterations analyzed in this study.
Similar content being viewed by others
Introduction
In northern and northeastern Brazil, gastric cancer (GC) is the second most common type of cancer and is considered a serious public health problem because it is usually diagnosed at an advanced stage[1]. In addition to its sporadic manifestation, GC is also associated with various syndromes that predispose the carrier to cancer. Among the familial forms of GC, hereditary diffuse gastric cancer (HDGC) is the only form with a well-defined genetic cause[2, 3].
In order for a family to qualify for a diagnosis of HDGC, the following criteria must be met: two or more documented cases of diffuse gastric cancer in first- or second-degree relatives with at least one diagnosed before the age of 50 years or three or more cases of documented diffuse gastric cancer in first- or second-degree relatives independent of the age of onset[4, 5].
The correlation between an E-cadherin gene germline mutation (CDH1 inactivation) and the predisposition to diffuse gastric cancer was first identified in a large family in New Zealand[6]. Based on this finding, HDGC was characterized and other occurrences were described in patients with different ethnic backgrounds[7, 8].
The CDH1 gene, located on the 16q22.1 chromosome, encodes the E-cadherin intercellular adhesion protein; this protein acts as a tumor suppressor and plays an important role in maintenance of the epithelial tissue architecture[9]. Mutations in this gene primarily affect both the intracellular and extracellular domains of the protein and thus affect the integrity of the protein, leading to disturbances in epithelial tissue cell-cell adhesion, increased cell motility and an enhanced infiltrative capacity and tumor metastasis[10, 11]. As HDGC is an infiltrative tumor, endoscopy and biopsy-based diagnostic strategies are inefficient; furthermore, given the high penetrance of CDH1 mutations, prophylactic gastrectomy is recommended for affected patients[11, 12].
Over one hundred germline mutations have been described for the CDH1 gene. Although several of these mutations have been detected in different families, to date, no hotspot has been characterized[3, 13]. Although the CDH1 gene is the predominantly affected gene in HDGC, other inactivation mechanisms should be investigated. Additionally, large deletions might also be responsible for CDH1 inactivation[8, 14–20]. For this reason, an array comparative genomic hybridization (aCGH) analysis is essential to the identification of quantitative alterations in the CDH1 gene or other genome regions in families affected by HDGC[21].
The objective of this study was to identify germline mutations in the CDH1 gene and/or quantitative genomic alterations in four families with HDGC in northern and northeastern Brazil.
Methodology
Patients
The samples evaluated in this study were obtained from patients who fulfilled the clinical criteria according to the latest consensus of the International Gastric Cancer Linkage Consortium[5]. The patients had been treated at referral hospitals in northern and northeastern Brazil. The samples were processed in their states of origin and then sent to the Federal University of Pará (Universidade Federal do Pará; UFPA) for genetic analysis.
A retrospective study of the family members was also conducted to identify previous generations with DGC. All genetically analyzed patients (or their guardians) signed consent forms that had been approved by the Research Ethics Committee of University Hospital João de Barros Barreto (Hospital Universitário João de Barros Barreto; HUJBB) under protocol number 274/12. Assurance was provided that the use of biological materials and participation in the study would not cause any harm to nor have any negative influence on patient treatment.
All biological materials except one sample (that was Formaldehyde Fixed-Paraffin Embedded tissue) was blood DNA. And all genetic screening analysis - mutation, deletion and methylation - were all looking for germline changes, not somatic.
DNA extraction
Peripheral blood samples were collected in EDTA-containing tubes and extracted with the QIAamp® DNA Blood Mini Kit (Qiagen N.V., Venlo, The Netherlands) according to the manufacturer’s instructions.
Paraffin block sample was obtained from one patient, and extracted with the QIAamp DNA® FFPE Tissue Kit (Qiagen) according to the manufacturer’s instructions.
Genotypic analysis
The obtained DNA was used to perform molecular screening of the CDH1 gene. Gene fragments containing the analyzed polymorphisms were amplified by polymerase chain reaction (PCR) using gene-specific reaction conditions and primers (Table 1) according to Brooks-Wilson et al.[22].
The result of each reaction was subjected to direct sequencing on an ABI 3130 capillary sequencing platform (Applied Biosystems/Life Technologies, Carlsbad, CA, USA). The sequences were obtained as electropherograms and analyzed with the software package provided with the equipment. The generated sequences were analyzed with the BIQ Analyzer software package[23].
aCGH
High-density probe microarray analyses were performed to determine the copy number variation (CNV). The complete genomes of all patients were evaluated with the goal of identifying genes related to tumor development.
The Affymetrix® CytoScan ™ HD Array (Affymetrix, Inc., Santa Clara, CA, USA) was used; this system features a total of approximately 1.9 million probes for detecting CNV and 750,000 SNP molecular markers. The standard protocol incorporates the following eight procedures before scanning the chip: genomic DNA digestion, NSP adapter ligation, fragment amplification by PCR (Polymerase Chain Reaction), PCR product purification, PCR product fragmentation, end-labeling, hybridization and washing.
The Chromosome Analysis Suite software v1.2.1 (Affymetrix®) was used for the chip analysis.
Methylation status
For methylation analyses, the samples were subjected to DNA modification using sodium bisulfite[24]. A fragment with 22 CpGs of the CDH1 promoter region was amplified using a nested PCR strategy[25]. Fragments obtained were purified using PCR Purification Kit (Invitrogen/Life Technologies, Carlsbad, CA, USA) and sequenced using an ABI3130 automatic sequencer (Applied Biosystems, Foster City, CA, USA). The sequences were aligned with BioEdit v7.0.5[26]. Methylation analyses were run in BiQ Analyzer[23] software.
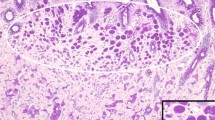
Immunohistochemistry
An anti-cadherin (Abcam PLC, Cambridge, UK) commercial primary antibody was used to detect the protein product of the CDH1 gene (HDGC). Streptavidin-biotin-peroxidase staining as described by Hsu et al.[27] was adopted as the immunohistochemical method. The normality parameter was defined with samples from normal (non-tumor) formalin-fixed and paraffin-embedded tissues that had been obtained from routine samples. The World Health Organization histopathological classifications for each tumor were used as well as the Lauren classification for gastric cancer[28].
Results
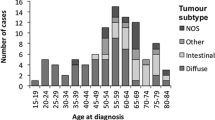
The detailed patient data are shown in Table 2. A total of 27 patient samples were collected for genetic analysis from four unrelated families with histories of DGC in northern and northeastern Brazil. All biological samples collected were peripheral blood, except for the patient AM05, whose sample was Paraffin-embedded tumor. The sample comprised 18 men and nine women with a mean age of 42 years and an age range of 20–75 years (24–56 years for women and 20–75 years for men).
Of these 27 patients, nine (33.4%) had been previously diagnosed with diffuse gastric cancer, whereas the remaining patients did not have any type of gastric tumor. Among the patients diagnosed with DGC, the age at diagnosis ranged from 27–67 years.After the retrospective study and using information collected from the analyzed patients, it was possible to identify relatives with a history of DGC and other types of tumors (Figure 1).
Pedigrees of hereditary diffuse gastric cancer families. (A), (B), (C) and (D) represents the four families presented in this study. The numbers present under the symbols represent the age at diagnosis. The solid symbols represent the affected members with confirmed diffuse gastric cancer diagnoses. Upper left arrows indicate the probands.
Mutations in the CDH1 gene
Among the four families of patients, two families exhibited germline mutations in the CDH1 gene, namely family A from northern Brazil and family B from northeastern Brazil (Table 3). In the other two families, which originated from northeastern Brazil, no mutations were found in the evaluated CDH1 exons.
Array comparative genomic hybridization (aCGH)
The aCGH sample analysis showed no gains or losses of DNA in the four tested families (27 samples).
Immunoreactivity in HDGC
CDH1 protein detection was performed only for patient AM05, a carrier of the germline mutation 185 G > T and member of family A. This patient died before the start of the study, and a genetic analysis was performed on a paraffin-embedded tumor tissue. The other study participants with this syndrome donated peripheral blood for genetic analysis, and consequently, there was no need to request paraffin blocks of the resected tumor tissues. The tumor cells of patient AM05, revealed negative immunoreactivity to the E-cadherin protein.
Methylation status in HDGC
We analyzed the methylation pattern of a CDH1 gene promoter region fragment in one CpG island containing 22 CpG dinucleotides, to find possible heritable epimutations. No promoter region hypermethylation was observed in all 27 tested individuals, from the four families, and also in 10 healthy controls.
Discussion
In addition to sporadic manifestation, gastric cancer can be associated with various syndromes that predispose the carrier to cancer. Among the familial forms of gastric cancer, HDGC is the only syndrome with a well-defined genetic cause[2, 3].
The relationship between a genetic germline mutation in the E-cadherin-encoding gene (CDH1 inactivation) and the predisposition to HDGC was first identified in a family in New Zealand[6]. Based on this finding, the HDGC syndrome was characterized, and other occurrences were described in patients with different ethnic backgrounds[29].
Mutations in CDH1 gene affect protein integrity, thus causing disturbances in cell-cell adhesion in epithelial tissues, increasing cell motility and enhancing infiltrative behavior of the tumor and metastasis development[10, 11].
This genetic study of four families that carried the HDGC syndrome allowed us to evaluate a previously unaddressed issue within the Brazilian population. CDH1 germline mutations are observed in 30–40% of cases that meet the clinical criteria for HDGC[30, 31]. In our study, 50% of the families exhibited CDH1 gene mutations. This information is useful in clinical evaluations of patients with family histories of HDGC because in addition to prophylactic measures, the information facilitates monitoring aimed at identifying the occurrence of other tumors such as lobular carcinomas of the breast; these types of cancers had also been detected in members of the families analyzed in this study[13, 20, 32].
The cases described in the literature demonstrate that the most common CDH1 gene alterations associated with HDGC are point mutations and small changes in the reading frame; these occur in approximately 93% of families with CDH1 gene mutations[13, 20, 33].
In this study, two individuals in family A, a father and son (Figure 1A), were carriers of a familial CDH1 gene mutation at nucleotide position 185 (185G > T); this mutation causes a change in the protein structure from the amino acid glycine to valine. This missense mutation was first described by Shinmura et al.[34] in a family of Japanese origin. Our results suggest the hypothesis that this 185G > T mutation was introduced into family A by the grandfather of the proband (first generation pedigree), who was of Japanese origin, and suggest that this mutation might result from this ethnic background.
A CDH1 gene germline mutation was also identified in two brothers from family B who had developed an early form of gastric cancer (before 45 years of age)[35]. The mutation was identified at nucleotide position 1018 (1018A > G) and resulted in a change from the amino acid threonine to alanine. The 1018A > G mutation was previously described in a family of European origin and in a Chinese family[36, 37]. Because the proband of this family was of Portuguese descent, it is possible that their ancestors brought this mutation to Brazil upon immigration. On the other hand, another alternative to ancestral mutations is an increased susceptibility of different CDH1 locations to mutations.
A literature review revealed the occurrence of a total of 122 germline mutations in the CDH1 gene in HDGC[38]. Although several types of mutations have been detected in different families, no hotspot has been characterized to date[3, 13]; this led us to sequence all 16 exons of the gene in the 30 members of the four analyzed families.
Of the mutations reported in the literature, approximately 15% are shared by many families worldwide, suggesting that CDH1 mutation-associated HDGC might share a common ancestry, as was suggested for families A and B in this study[33, 39].
In the other two families (C and D), in which the evaluated subjects carried no CDH1 gene mutations, there were considerable numbers of HDGC-affected members in different generations (Figure 1). Pinheiro et al.[20] have proposed that many HDGC families carry some mutations in non-exonic regulatory regions of CDH1 (or in upstream regulators). Based on this, it may be possible in the future to test families C and D, for allele-specific loss on CDH1.
In other populations in which the incidence of gastric cancer is high, there are also reports of HDGC-carrier families with large numbers of affected individuals who do not carry CDH1 gene germline mutations. This finding might be consequent to exposure to environmental risk factors or the susceptibility of individuals to genetic alterations in low-penetrance genes[40, 41].
In a study conducted in southeastern Brazil on 88 patients with early gastric cancer, 16 of whom had familial histories of gastric cancer, it was possible to detect changes in the E-cadherin protein expression in 41 individuals via immunohistochemical analysis. Although CDH1 gene sequencing was not conducted to identify possible mutations, the immunohistochemical analysis revealed the involvement of CDH1 in the early development of gastric cancer in a Brazilian population[42].
Because the CDH1 gene acts as a tumor suppressor, other gene inactivation mechanisms of this gene besides germline mutations in one allele should be investigated to identify changes to the second allele in somatic cells (second event of the Knudson hypothesis[43]), which was not able to be done in the present work. Mechanisms such as CDH1 gene deletion[33] and promoter region hypermethylation[44], were investigated in germline from those analyzed patients, because are also considered potentially responsible for its inactivation.
Cytosine hypermethylation in the CpG dinucleotides present within the CDH1 promoter region induces transcriptional silencing[45] and might thus explain the lack of E-cadherin immunoreactivity. However, analyses to confirm the presence of CDH1 gene promoter region hypermethylation in patients with HDGC have not been conclusive. For example, studies by Li et al.[46] and Concolino et al.[47] demonstrated CDH1 promoter hypermethylation-mediated gene silencing in 53–57% of patients with HDGC. Conversely, Wu et al.[48] reported an absence of this phenomenon in 140 Chinese gastric cancer patients with a familial history of HDGC.
The analyses conducted in the present study did not detect CDH1 gene promoter region hypermethylation in the families with HDGC syndrome. Our results reinforce the theory put forth by Yamada et al.[19] who, after analyzing 22 Japanese patients with early gastric cancer, suggested that germline CDH1 promoter hypermethylation was not a predisposing factor of gastric cancer.
In addition to epigenetic alterations in the promoter region, the CDH1 gene might also suffer deletions even in the absence of point mutations in the germlines of patients with HDGC[49]. Kim et al.[50] used multiplex ligation-dependent probe amplification (MLPA) to analyze 23 patients with HDGC and, similarly to our study, found no deletions or duplications in these genes.
Oliveira et al.[33] genetically analyzed 160 patients with HDGC from different geographic regions and found that CDH1 gene deletions occurred in the peripheral blood in approximately 4% of families affected by this syndrome. The same authors also observed that all families with CDH1 deletions originated from countries with low gastric cancer incidence rates. A large number of patients with HDGC, in northern and northeastern from Brazil, needs to be analyzed to verify if the absence of CDH1 gene deletions and other quantitative genomic alterations, as found in patients of this work, corroborate this observation because these regions have high gastric cancer incidence rates.
It is widely known that the most common forms of cancer develop as a result of interactions between endogenous and environmental factors such as the diet[51]. Environmental factors might be related to the high incidence of these neoplasms in the northern and northeastern regions, or for some reason the HDGC frequency is higher than elsewhere in the world, where sporadic gastric cancer is also endemic, such as Japan and Korea. In particular, Helicobacter pylori (H. pylori) infection during childhood as well as the high consumption of salt-preserved foods, infrequent use of refrigeration and low consumption rates of cereals, fresh fruits and vegetables are considered risk factors for gastrointestinal tumors[52–55].
Conclusions
This is the first study to evaluate CDH1 gene germline mutations and quantitative gene alterations in Brazilian families with HDGC. CDH1 gene germline mutations were found in 50% of the families evaluated. The detected mutations appeared to originate from Asia and Europe. This migratory flow does not rule out the possibility that environmental factors might have caused these same mutations in the affected members of the analyzed families. No quantitative changes were observed in the genomes of any of the analyzed families. It is possible that in regions with high gastric cancer incidence rates such as northern and northeastern Brazil, environmental factors or other molecular mechanisms might induce different genetic alterations from those analyzed in this study.
References
da Silva JAG: Estimate/2012—Cancer Incidence in Brazil. Rio de Janeiro: National Cancer Institute; 2011. (acessed 15 Out, 2013) http://www.inca.gov.br/estimativa/2012
Bresciani C, Perez RO, Gama-Rodrigues J: Familial gastric cancer. Arq Gastroenterol 2003, 40: 114–7.
Guilford P, Blair V, More H, Humar B: A short guide to hereditary diffuse gastric cancer. Hered Cancer Clin Pract 2007, 5: 183–94.
Caldas C, Carneiro F, Lynch HT, Yokota J, Wiesner GL, Powell SM, Lewis FR, Huntsman DG, Pharoah PDP, Jankowski JA, MacLeod P, Vogelsang H, Keller G, Park KGM, Richards FM, Maher ER, Gayther SA, Oliveira C, Grehan N, Wight D, Seruca R, Roviello F, Ponder BAJ, Jackson CE: Familial gastric cancer: overview and guidelines for management. J Med Genet 1999, 36: 873–80.
Fitzgerald RC, Hardwick R, Huntsman D, Carneiro F, Guilford P, Blair V, Chung DC, Norton J, Ragunath K, Krieken JHV, Dwerryhouse S, Caldas C: Hereditary diffuse gastric cancer: updated consensus guidelines for clinical management and directions for future research. J Med Genet 2010, 47: 436–44.
Guilford P, Hopkins J, Harraway J, McLeod M, McLeod N, Harawira P, Taite H, Scoular R, Miller A, Reeve AE: E-cadherin germline mutations in familial gastric cancer. Nature 1998, 392: 402–5.
Dunbier A, Guilford P: Hereditary diffuse gastric cancer. Adv Cancer Res 2001, 83: 55–65.
Moran CJ, Joyce M, McAnena OJ: CDH1 associated gastric cancer: a report of a family and review of the literature. Eur J Surg Oncol 2005, 31: 259–64.
van Roy F, Berx G: The cell-cell adhesion molecule E-cadherin. Cell Mol Life Sci 2008, 65: 3756–88.
Mateus AR, Simões-Correia J, Figueiredo J, Heindl S, Alves CC, Suriano G, Luber B, Seruca R: E-cadherin mutations and cell motility: a genotype–phenotype correlation. Exp Cell Res 2009, 315: 1393–402.
Ghaffari SR, Rafati M, Sabokbar T, Dastan J: A novel truncating mutation in the E- cadherin gene in the first Iranian family with hereditary diffuse gastric cancer. Eur J Surg Oncol 2010, 36: 559–62.
Mayrbaeurl B, Kellerf G, Schauerb W, Burgstaller S, Czompo M, Hoebling W, Knoflach P, Duba HC, Hoefler H, Thaler J: Germline mutation of the E- cadherin gene in three sibling cases with advanced gastric cancer: clinical consequences for the other family members. Eur J Gastroenterol Hepatol 2010, 22: 306–10.
Guilford P, Humar B, Blair V: Hereditary diffuse gastric cancer: translation of CDH1 germline mutations into clinical practice. Gastric Cancer 2010, 13: 1–10.
Fitzgerald RC, Caldas C: Clinical implications of E-cadherin associated hereditary diffuse gastric cancer. Gut 2004, 53: 775–8.
Oliveira C, Suriano G, Ferreira P, Canedo P, Kaurah P, Mateus R, Ferreira A, Ferreira AC, Oliveira MJ, Figueiredo C, Carneiro F, Keller G, Huntsman D, Machado JC, Seruca R: Genetic screening for familial gastric cancer. Hered Cancer Clin Pract 2004, 2: 51–64.
Corso G, Roviello F, Paredes J, Pedrazzani C, Novais M, Correia J, Marelli D, Cirnes L, Seruca R, Oliveira C, Suriano G: Characterization of the P373L E-cadherin germline missense mutation and implication for clinical management. Eur J Surg Oncol 2007, 33: 1061–7.
Barber M, Murrell A, Ito Y, Maia AT, Hyland S, Oliveira C, Save V, Carneiro F, Paterson AL, Grehan N, Dwerryhouse S, Lao-Sirieix P, Caldas C, Fitzgerald RC: Mechanisms and sequelae of E-cadherin silencing in hereditary diffuse gastric cancer. J Pathol 2008, 216: 295–306.
Oliveira C, Sousa S, Pinheiro H, Karam R, Bordeira-Carriço R, Senz J, Kaurah P, Carvalho J, Pereira R, Gusmão L, Wen X, Cipriano MA, Yokota J, Carneiro F, Huntsman D, Seruca R: Quantification of epigenetic and genetic 2nd hits in CDH1 during hereditary diffuse gastric cancer syndrome progression. Gastroenterology 2009, 136: 2137–48.
Yamada H, Shinmura K, Goto M, Iwaizumi M, Konno H, Kataoka H, Yamada M, Ozawa T, Tsuneyoshi T, Tanioka F, Sugimura H: Absence of germline mono-allelic promoter hypermethylation of the CDH1 gene in gastric cancer patients. Mol Cancer 2009, 8: 63.
Pinheiro H, Bordeira-Carriço R, Seixas S, Carvalho J, Senz J, Oliveira P, Inácio P, Gusmão L, Rocha J, Huntsman D, Seruca R, Oliveira C: Allele-specific CDH1 downregulation and hereditary diffuse gastric cancer. Hum Mol Genet 2010, 19: 943–52.
Fan B, Dachrut S, Coral H, Yuen ST, Chu KM, Law S, Zhang L, Ji J, Leung SY, Chen X: Integration of DNA copy number alterations and transcriptional expression analysis in human gastric cancer. PLoS ONE 2012, 7: e29824.
Brooks-Wilson AR, Kaurah P, Suriano G, Leach S, Senz J, Grehan N, Butterfield YSN, Jeyes J, Schinas J, Bacani J, Kelsey M, Ferreira P, MacGillivray B, MacLeod P, Micek M, Ford J, Foulkes W, Australie K, Greenberg C, LaPointe M, Gilpin C, Nikkel S, Gilchrist D, Hughes R, Jackson CE, Monagham KG, Oliveira MJ, Seruca R, Gallinger S, Caldas C, Huntsman D: Germline E-cadherin mutations in hereditary diffuse gastric cancer: assessment of 42 new families and review of genetic screening criteria. J Med Genet 2004, 41: 508–17.
Bock C, Reither S, Mikeska T, Paulsen M, Walter J, Lengauer T: BiQ Analyzer: visualization and quality control for DNA methylation data from bisulfite sequencing. Bioinformatics 2005, 21: 4067–8.
Herman JG, Graff JR, Myohanen S, Nelkin BD, Baylin : Methylation-specific PCR: a novel PCR assay for methylation status of CpG islands. Proc Natl Acad Sci USA 1996, 93: 9821–9826.
Nojima D, Nakajima K, Li L, Franks J, Ribeiro-Filho L, Ishii N, Dahiya R: CpG methylation of promoter region inactivates E-cadherin gene in renal cell carcinoma. Molecular Carcinogenesis 2001, 32: 10–27.
Hall TA: BioEdit: a user-friendly biological sequence aligment editor and analysis program for Windows 95/98/NT. Nucleic Acids Symp Ser 1999, 41: 95–8.
Hsu SM, Raine L: Protein A, avidin, and biotin in immunohistochemistry. J Histochem Cytochem 1981, 29: 1349–53.
Lauren P: The two histological main types of gastric carcinoma: diffuse and so-called intestinal-type carcinoma. An attempt at a histo-clinical classification. Acta Pathol Microbiol Scand 1965, 64: 31–49.
Oliveira C, Pinheiro H, Figueiredo J, Seuca R, Carneiro F: E-cadherin alterations in hereditary disorders with emphasis on hereditary diffuse gastric cancer. Prog Mol Biol Transl Sci 2013, 116: 337–59.
Fitzgerald RC, Caldas C: E-cadherin mutations and hereditary gastric cancer: prevention by resection? Dig Dis 2002, 20: 23–31.
Corso G, Pedrazzani C, Pinheiro H, Fernandes E, Marelli D, Rinnovati A, Pascale V, Seruca R, Oliveira C, Roviello F: E-cadherin genetic screening and clinico-pathologic characteristics of early onset gastric cancer. Eur J Cancer 2011, 47: 631–9.
Benusiglio PR, Malka D, Rouleau E, De Paul A, Buecher B, Nogues C, Forume E, Colas C, Coulet F, Warcoin M, Grandjouan S, Sezeur A, Laurent-Puig P, Moliere D, Tlemsani C, Di Maria M, Byrde V, Delaloge S, Blayau M, Caron O: CDH1 germline mutations and the hereditary diffuse gastric and lobular breast cancer syndrome: a multicentre study. J Med Genet 2013, 50: 486–9.
Oliveira C, Senz J, Kaurah P, Pinheiro H, Sanges R, Haegerte A, Corso G, Schouten J, Fistzgerald R, Vogelsang H, Keller G, Dwerryhouse S, Grimmer D, Chin SF, Yang HK, Jackson CE, Seruca R, Roviello F, Stupka E, Caldas C, Huntsman D: Germline CDH1 deletions in hereditary diffuse gastric cancer families. Hum Mol Genet 2009, 18: 1545–55.
Shinmura K, Kohno T, Takahashi M, Sasaki A, Ochiai A, Guilford P, Hunter A, Reeve AE, Sugimura H, Yamaguchi N, Yokota J: Familial gastric cancer: clinicopathological characteristics, RER phenotype and germline p53 and Ecadherin mutations. Carcinogenesis 1999, 20: 1127–31.
Milne AN, Sitarz R, Carvalho R, Carneiro F, Offerhaus GJ: Early onset gastric cancer: on the road to unraveling gastric carcinogenesis. Curr Mol Med 2007, 7: 15–28.
Oliveira C, Bordin MC, Grehan N, Huntsman D, Suriano G, Machado JC, Kiviluoto T, Aaltonen L, Jackson CE, Seruca R, Caldas C: Screening E-cadherin in gastric cancer families reveals germline mutations only in hereditary diffuse gastric cancer kindred. Hum Mutat 2002, 19: 510–7.
Zhang Y, Liu X, Fan Y, Ding J, Xu A, Zhou X, Hu X, Zhu M, Zhang X, Li S, Wu J, Cao H, Li J, Wang Y: Germline mutations and polymorphic variants in MMR, E-cadherin and MYH genes associated with familial gastric cancer in Jiangsu of China. Int J Cancer 2006, 119: 2592–6.
Corso G, Marrelli D, Roviello F: Familial gastric cancer and germline mutations of E-cadherin. Ann Ital Chir 2012, 83: 177–82.
Kaurah P, MacMillan A, Boyd N, Senz J, De Luca A, Chun N, Suriano G, Zaor S, Van Manen L, Gilpin C, Nikkel S, Connolly-Wilson M, Weissman S, Rubinstein WS, Sebold C, Greenstein R, Stroop J, Yim D, Panzini B, McKinnon W, Greenblatt M, Wirtzfeld D, Fontaine D, Coit D, Yoon S, Chung D, Lauwers G, Pizzuti A, Vaccaro C, Redal MA, et al.: Founder and recurrent CDH1 mutations in families with hereditary diffuse gastric cancer. JAMA 2007, 297: 2360–72.
Figueiredo C, Machado JC, Pharoah P, Seruca R, Sousa S, Carvalho R, Capelinha AF, Quint W, Caldas C, van Doorn LJ, Carneiro F, Sobrinho-Simões M: Helicobacter pylori and interleukin 1 genotyping: an opportunity to identify high-risk individuals for gastric carcinoma. J Natl Cancer Inst 2002, 94: 1680–7.
Machado JC, Figueiredo C, Canedo P, Pharoah P, Carvalho R, Nabais S, Castro Alves C, Campos ML, Van Doorn LJ, Caldas C, Seruca R, Carneiro F, Sobrinho-Simões M: A proinflammatory genetic profile increases the risk for chronic atrophic gastritis and gastric carcinoma. Gastroenterology 2003, 125: 364–71.
Silva EM, Fregnani JHTG, Martel G, Costa WL Jr, Coimbra FJF, Achatz MIW, Hainaut P, Soares FA: Molecular analyses of early-onset gastric cancer in Brazilian patients: TP53 mutations, cadherin-catenin and mucins proteins expression. J Cancer Ther 2013, 4: 33–42.
Knudson AG: Genetics of human cancer. Annu Rev Genet 1986, 20: 231–51.
Yamamoto E, Suzuki H, Takamaru H, Yamamoto H, Toyota M, Shinomura Y: Role of DNA methylation in the development of diffuse-type gastric cancer. Digestion 2011, 83: 241–9.
do Nascimento Borges B, Burbano RM, Harada ML: Analysis of the methylation patterns of the p16 INK4A, p15 INK4B, and APC genes in gastric adenocarcinoma patients from a Brazilian population. Tumour Biol 2013, 34: 2127–33.
Li XJ, Zhao Y, Ren H: E-cadherin expression and CDH1 promoter methylation in sporadic and hereditary gastric cancer. J South Med Univ 2013, 33: 125–7.
Concolino P, Papa V, Mozzetti S, Ferlini C, Pacelli E, Martinelli E, Ricci R, Filippetti F, Scambia G, Doglietto GB: The unsolved enigma of CDH1 down-regulation in hereditary diffuse gastric cancer. J Surg Res 2004, 121: 50–5.
Wu PY, Zhang Z, Wang JM, Guo WW, Xiao N, He Q, Wang YP, Fan YM: Germline promoter hypermethylation of tumor suppressor genes in gastric cancer. World J Gastroenterol 2012, 18: 70–8.
Yamada M, Fukagawa T, Nakajima T, Asada K, Sekine S, Yamashita S, Okochi-Takada E, Taniguchi H, Kushima R, Oda I, Saito Y, Ushijima T, Katai H: Hereditary diffuse gastric cancer in a Japanese family with a large deletion involving CDH1. Gastric Cancer 2013. Sep 15 [Epub ahead of print]
Kim S, Chung JW, Jeong TD, Park YS, Lee JH, Ahn JY, Kim DH, Choi KD, Lee W, Song HJ, Lee GH, Chun S, Jung HY, Min WK, Kin JH: Searching for E-cadherin gene mutations in early onset diffuse gastric cancer and hereditary diffuse gastric cancer in Korean patients. Fam Cancer 2013, 12: 503–7.
Haas P, Anton A, De Francisco A: Câncer colo retal no Brasil: consumo de grãos integrais como prevenção [Colorectal cancer in Brazil: whole grain consumption as prevention]. Rev Bras Análises Clínicas 2007, 39: 231–5.
Moutinho V, Makino E: Epidemiological features of the gastric cancer in Belém (Brasil). Arq Bras Cir Dig 1988, 3: 69–74.
Koifman S, Koifman RJ: Environment and cancer in Brazil: an overview from a public health perspective. Mutat Res 2003, 544: 305–11.
Neves FJ, Koifman RJ, Mattos IE: Mortalidade por câncer de cólon e reto e consumo alimentar em capitais brasileiras selecionada [Colorectal cancer mortality and dietary patterns in selected Brazilian state capitals]. Rev Bras Epidemiol 2006, 9: 112–20.
Nakashima JP, Koifman RJ, Koifman S: Cancer incidence in the Western Amazon: population-based estimates in Rio Branco, Acre State, Brazil, 2007–2009. Cad Saude Publica 2012, 28: 2125–32.
Acknowledgments
This study was supported by Conseho Nacional de Desenvolvimento Científico e Tecnológico (http://www.cnpq.br) grant number 401976/2010-6, 305220/2013-6 to RRB and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (http://www.capes.gov.br) grant number PNPD 2810/2011 to CFAMN. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
Conceived and designed the experiments: CFAMN, MBLB, BNB, LML, RMRB. Performed the experiments: CFAMN, MBLB, BNB, LML, ABB. Analyzed the data: CFAMN MBLB, BNB, HFR, RMRB. Wrote the paper: CFAMN, PPA, JAR, GRP, RMRB. All authors read and approved the final manuscript.
Caroline Aquino Moreira-Nunes contributed equally to this work.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Moreira-Nunes, C.A., Barros, M.B.L., do Nascimento Borges, B. et al. Genetic screening analysis of patients with hereditary diffuse gastric cancer from northern and northeastern Brazil. Hered Cancer Clin Pract 12, 18 (2014). https://doi.org/10.1186/1897-4287-12-18
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1897-4287-12-18