Abstract
Feeding small for gestational age (SGA) newborns is extremely challenging and the neonatologist should be brave and cautious at the same time. Although these babies have a high risk of milk intolerance and necrotising enterocolitis, enteral feeding guidelines are not well established and practice varies widely among different neonatal units. Currently available studies on this topic include extremely and very low birth weight neonates, but are not focused specifically on small for gestational age infants. This review analyzes papers focused on feeding interventions in order to provide the best available evidences about the optimum timing for introduction of enteral feeding, how fast feed volume can be advanced, which milk and which feeding method is more appropriate in SGA infants.
Similar content being viewed by others
Background
The term “small for gestational age” (SGA) is used to describe newborns whose birth weight and/or crown-heel length is less than expected for their gestational age and sex. Traditionally, the term SGA has been used to describe a neonate whose weight and/or length at birth is at least 2 SD below the mean for the infant’s gestational age, equivalent to the 2.3 percentile, based on the data derived from an appropriate reference population [1]. Some publications define SGA newborns as those with birth weight or length below the 3rd, 5th, or 10th percentiles for gestational age [2]. The first definition was chosen by the international SGA advisory panel because it likely includes the majority of patients with impaired fetal growth.
However, this definition of SGA is inaccurate because it is not able to exclude the constitutional smallness, which is not pathological [3]. The term intrauterine growth retardation (IUGR) suggests diminished growth velocity in the fetus as documented by at least 2 intrauterine growth assessment. Therefore SGA and IUGR are not synonymous. IUGR indicates the presence of a pathological process occurring in utero that inhibits fetal growth. Being born SGA does not necessarily mean that an intrauterine growth retardation has occurred and infants who are IUGR are not inevitably SGA at birth.
There are several causes for being SGA. Exposure of the fetus to toxins (smoking, alcohol, drug abuse), chromosomal anomalies (trisomy 13, Edward Syndrome, Turner Sydrome, Prader-Willy Syndrome etc.), congenital infections (toxoplasmosis, rubella, cytomegalovirus), metabolic disorders, maternal factors (both young and advanced age, maternal hypertension, placental and uterine abnormalities etc.). However the most common etiology of being born SGA is placental insufficiency that impairs growth particularly during the last trimester of pregnancy leading to IUGR [4–6]. Below we discuss the most severe and important complication for these neonates, with pathophysiological considerations.
NEC
Necrotizing enterocolitis (NEC) is a severe inflammatory disorders in which prematurity and enteral feeding seems the major predisposing factors. It occurs in up to 7% of very low birth weight infants, with a mortality rate of 15 - 30%, inversely related to birth weight and gestational age [7]. Garite et al. in a retrospective study including 29.916 premature newborns found that both SGA and IUGR were independently associated with an increased risk of NEC [8] By the physiological point of view growth restriction modifies the developmental pattern of intestinal structure. The intestine of SGA neonates has reduced weight, length, wall thickness, villous weight, and crypt depth [9, 10]. Furthermore these infants have intestinal dysbiosis and an alteration of the proliferation-apoptosis homeostasis which leads to a reduced surface of intestinal exchange [11]. These alterations could be responsible for the higher gastrointestinal morbidity, feeding intolerance and impaired nutrient absorption.
However recently much attention was focused on those infants born prematurely with IUGR and abnormal blood flow on antenatal Doppler studies [12]. Increased placental resistance in the presence of placental failure leads to a reduction in end diastolic blood flow through the umbilical arteries, progressing to absent (AEDF) or reversed flow (AREDF) [13]. Pathophysiology of fetal adaptation to chronic hypoxia involves preferential shunting of blood to the brain at the expense of the splanchnic circulation. It was shown that severe prenatal Doppler abnormalities are associated with poor fetal outcome [14, 15], but it is still debated if they increased the risk of neonatal NEC.
Some studies have demonstrated a close association between AEDF or AREDF and NEC, which appears to be independent of other factors such as degree of growth retardation, prematurity and perinatal asphyxia [16, 17], while others have not confirmed these findings [18, 19]. A meta-analysis of 14 observational studies demonstrated an increased incidence of NEC in preterm infants who had suffered fetal AREDF compared with controls, with an odds ratio of 2.13 (95% CI 1.49 to 3.03) [20]. Nine of the included studies showed an excess of NEC in the AREDF infants; eight studies classified NEC using the stricter definition of radiological or surgical confirmation, of which six showed an excess of confirmed NEC in the AREDF group. Overall, confirmed NEC was not significantly increased in these studies (OR 1.6, 95% CI 0.9 to 2.8), but the six studies examining confirmed NEC in preterm infants with IUGR showed greatly increased odds of confirmed NEC in infants with fetal AREDF (OR 6.9, 95% CI 2.3 to 20). In many of the studies, fetuses with AREDF required earlier delivery than controls so it could be argued that the higher risk of NEC in these studies was primarily related to the lower gestational age and birth weight; nevertheless, the excess of confirmed NEC was also found in the two series that matched controls for gestation and weight (OR 5.5, 95% CI 1.1 to 28) [16, 21]. A more recent study confirmed the results of this meta-analysis demonstrating a strong relation between AREDF and subsequent development of NEC (OR: 5.88, 95% CI: 2.41 to 14.34) also after adjustment for gestational age at birth (OR: 7.64, 95% CI: 2.96 to 19.70,) and after adjustment for birth weight for gestational age z-score (OR: 6.72, 95% CI: 2.23 to 20.25) [22].
All the previous studies examined only the role of umbilical arteries Doppler flows. When Manogura et al. [23] investigated a more comprehensive fetal Doppler assessment that provided greater circulatory details (umbilical artery, middle cerebral artery, ductus venosus, and umbilical vein) the association between NEC and AREDF was lost. In this study, a multinomial logistic regression with NEC as dependent variable failed to demonstrate a relationship between placental resistance and the risk of NEC, and found that birth weight and base deficit at birth were the independent risk factors for NEC. These results have raised some doubts on the reliability of all the evidences suggesting a causal relationship between NEC and abnormal placental resistance. Moreover, many studies were underpowered given the overall low incidence of NEC, and the metabolic status at birth was not taken into consideration by any of these studies. If it is plausible that placental insufficiency predisposes to, but does not initiate, the cascade of events that lead to NEC, it is more likely that the limitations of prematurity define the origins of this disease.
The questions about feeding SGA infant
Enteral feeding guidelines are not well established in preterm SGA neonates, and there is a lack of published information about best feeding regimen. Practice varies widely among different neonatal units as shown by a survey carried out in two different English Health Regions, but a policy of delayed and careful introduction of enteral feeding is often chosen in order to prevent NEC [20]. We now analyze the best current evidences on feeding SGA infants.
What milk
Human breast milk would be expected to protect against NEC for its antimicrobial and anti-inflammatory characteristics. However, proving efficacy in randomized clinical trial has been challenging because of 2 main reasons. First of all, the difficulty of recruiting infants to a randomized trial about human milk when mothers have strong preferences, secondly the lack of standardized definitions of what human milk comprises (maternal or donor, fortified or unfortified, human milk alone or human milk plus formula).
In 1990 Lucas and Cole demonstrated a reduction in the incidence of NEC among preterm infants who received only human milk when compared with infants who received bovine milk–based formula [24]. Two meta-analysis of several small randomized controlled trials reported a lower incidence and severity of NEC in infants fed with an exclusively human milk diet [25, 26]. A recent trial randomized 207 premature infants with a birth weight between 500 and 1250 grams to receive fortified human milk or bovine-milk based products and confirmed earlier data finding that the rates of NEC and NEC requiring surgery were markedly lower in the first group. The number of infants needed to treat (NNT) with an exclusively human milk diet to prevent 1 case of NEC was 10 and NNT to prevent 1 case of surgical NEC or death is 8 [27].
Early vs delayed
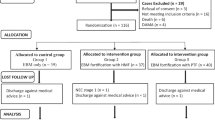
Early enteral feeding is advantageous because it improves the functional adaptation of the gastrointestinal tract by stimulating hormone secretion and gastrointestinal motility [28]. It also decreases the need of total parenteral nutrition and its associated complications, such as catheter related sepsis, cholestasis, cardiac tamponade, osteopenia of prematurity and other metabolic disturbances [29, 30]. Despite this, early enteral feeding is often delayed in high risk infants because it has been thought to be associated with an increased risk of NEC. A meta-analysis of five RCTs conducted on preterm infants did not detect a significantly different risk of NEC between infants randomized to delayed feeding (defined as introduction of enteral feeds as later than day 5–7 after birth) and infants randomized to early feeding (defined as less than 4 day after birth); RR 0.89 (95% CI 0.58 to 1.37) [31]. The two largest trials in that meta-analysis [32, 33] recruited only SGA infants with abnormal fetal circulatory distribution or flow. For these reasons, data from these trials do not provide sufficient evidence that delayed introduction of enteral feeding in SGA neonates reduces the risk of NEC, even if 95% CI for the pooled estimates of effect is wide and consistent with more than 40% reduction in the risk of NEC and death in newborns who have delayed introduction. Given this level of uncertainty this findings should be applied cautiously.
Minimal enteral feeding
An alternative approach to delaying feeding is the minimal enteral feeding (MEF). MEF (also known as “trophic feeding”, “gut-priming”, “non nutritive feeding” and “hypocaloric feeding”) is conventionally defined as giving small volumes of milk (typically 12 to 24 ml/kg/day every 1–3 hours) starting within the first few days after birth without advancing the feed volumes during the first week of life [34]. Enteral fasting during the early neonatal period has potential disadvantages for premature infants, because gastrointestinal hormone and motility are improved by enteral milk. Delayed enteral feeding could impair the functional adaptation of the gastrointestinal tract leading to intestinal dismotility and consequent feeding intolerance [35, 36]. A systematic review published in the Cochrane Library [37] did not detect a statistically significant effect on the incidence of NEC between very low birth weight newborns randomized to MEF and to no enteral feeding (RR 1.07 95% CI 0.67 to 1.70). Substantial clinical uncertainty remains about the effect of MEF on SGA infants because most of the trials on this topic specifically exclude infants who were SGA at birth. The only one including 56 babies with birth weight below 2000 grams and below 10th percentile for gestational age failed to demonstrate significant differences between newborns fed with trophic feeding or no feeds for the first five days of life in the primary outcome of intestinal permeability measured by the sugar absorption test [38]. There were also no differences in feeding tolerance, growth and incidence of NEC between the two groups [38].
How to advance feed volume
The rate of advancement of enteral feeding is another area of uncertainty. Retrospective studies have found that those neonatal centers where enteral feeding is introduced earlier and feeding volume advanced faster have higher incidences of NEC [39]. On the other hand, slow advancement of enteral feeding delays the establishment of full enteral nutrition and extends the duration of total parenteral nutrition with its associated risks [40], that may have adverse consequences for survival, growth and development [41]. A meta-analysis of four trials (496 very low birth weight infants) showed no differences in NEC rates comparing rapid (as 30 to 35 ml/kg/day) versus slow (as 15 to 20 ml/kg/day) advancement feeding strategies (RR 0.91 95% CI 0.47 to 1.75) [42]. Infants fed at faster rate reached the full enteral feeding about two to five days earlier than infants fed slowly, but they did not have a higher risk of NEC. However, these findings should be applied with caution to SGA newborns because the vast majority of the studied infants were appropriate for gestational age. Only in the trial performed by Salhotra et al. [43] more than 95% of the 53 participants were SGA. In this trial, the fast enteral feeding group reached the full enteral feed significantly earlier (mean 10 days) than the slow advancement group (mean 14.8 days), and there were two cases of NEC in the fast advancement group. To date there are no trial that compare slow versus fast feeding regimen in a selected population of SGA newborns.
Mode of feeding
To date there are no studies focused on SGA newborns and the best mode of feeding. The few available data concern premature infants born < 1500 grams that are not able to coordinate sucking, swallowing, and breathing. A systematic review of seven trials published in the Cochrane Library [44] did not detect a statistically significant effect between continuous versus intermittent milk feeding methods in time to achieve full enteral feeding, in feeding intolerance, in somatic growth and in incidence of NEC. At the present time practice appears to be based more on individual assessment rather than on scientific evidence. Continuous feeding may reduce energy expenditure [45] and improve feeding tolerance, nutrient adsorption and growth [46]; on the other hand, intermittent bolus method may be more physiologic, promoting the cyclical pattern of release of gastrointestinal hormones, which are important for gut development [47].
Feeding intolerance
Feeding intolerance is usually characterized by gastric residuals before feeding, emesis and abdominal distention. The gastric residual volume (GRV) is the element of feeding that can be measured and compared most easily. Several authors suggested to use GRV as a marker of feeding intolerance, in order to make early detection of NEC [48–50]. Qualitative and quantitative evaluation of gastric residuals can be performed. To date is difficult to assess a tolerance threshold of GRV beyond which enteral feeding should be withdrawn. Mihatsch et al. [48] tolerated GRV up to 2 mL in newborns ≤ 750 grams and up to 3 mL in newborns from 750 to 1000 grams in their protocol, but concluded that additional research is required to evaluate if GRV threshold could be increased up to 5 ml/kg body weight. Cobb et al. [49] found that GRV > 3.5 mL or 33% of a single meal may be associated with a higher risk for NEC while a GRV <1.5 mL or 25% of a meal is probably normal. Finally the available data on qualitative evaluation of gastric residuals suggest that infants with blood stained or hemorrhagic residuals were at higher risk of NEC, whereas bile stained residuals are not a risk factor by themselves [50].
Quality of the evidence
Being born SGA does not necessarily mean that IUGR has occurred, and infants who are IUGR are not inevitably SGA at birth. Unfortunately, the terms IUGR and SGA have been used interchangeably, creating confusion on the topic. In the absence of congenital malformations or chromosomal abnormalities, small fetal size could be the consequence of two distinct processes: constitutional smallness or pathological growth restriction. Distinguishing one process from the other is challenging, but such distinctions have profound implications toward understanding quality and robustness of evidence provided by available trials. Patients enrolled in the studies are usually selected according to their birth weight (below the 10th or the 3rd percentile) without checking if a growth restriction really occurred. So SGA is a term that is often used as a proxy for restricted growth, thereby combining both constitutionally small and pathologically growth restricted fetuses. It is known that growth restricted fetuses are small because of some underlying pathological conditions (smoking during pregnancy, uteroplacental dysfunction, hypertensive disorders, etc.), and they are therefore at increased risk for neonatal morbidity and mortality. On the other hand, constitutionally small infants can easily have morbidity and mortality very similar to appropriate for gestational age, and considerably lower than pathologically growth restricted ones [51].
Conclusions
There is limited evidence on which to base feeding policy in SGA newborns. Currently available studies on this topic include extremely and very low birth weight neonates, but are not focused specifically on SGA infants. Furthermore there are not RCTs that make a clear distinction between SGA and growth restricted neonates. Future randomized trials on feeding intervention should be targeted on IUGR infants, excluding constitutionally small newborns, in order to provide robust evidence concerning the optimum timing for introduction of enteral feeding, how fast feed volume can be advanced and which feeding method is more appropriate. To date, however, no trials showed any benefits of delayed enteral feeding or slow advancement of enteral feed volumes. Growth restricted newborns are a nutritional emergency that will result in serious short and long term detrimental effects, when left untreated.
Abbreviations
- SGA:
-
Small for gestational age
- IUGR:
-
Intrauterine growth restriction
- NEC:
-
Necrotizing enterocolites
- AEDF:
-
Absent end diastolic flow
- AREDF:
-
Absent and reverse end diastolic flow
- SMA:
-
Superior mesenteric artery
- MEF:
-
Minimal enterale feeding
- GRV:
-
Gastric residual volume.
References
Lee PA, Chernausek SD, Hokken-Koelega AC, Czernichow P, International Small for Gestational Age Advisory B: International Small for Gestational Age Advisory Board consensus development conference statement: management of short children born small for gestational age, April 24-October 1, 2001. Pediatrics. 2003, 111: 1253-1261. 10.1542/peds.111.6.1253.
Saenger P, Czernichow P, Hughes I, Reiter EO: Small for gestational age: short stature and beyond. Endocr Rev. 2007, 28: 219-251.
Gardosi J: New definition of small for gestational age based on fetal growth potential. Horm Res. 2006, 65 (Suppl 3): 15-18.
Thompson JM, Clark PM, Robinson E, Becroft DM, Pattison NS, Glavish N, Pryor JE, Wild CJ, Rees K, Mitchell EA: Risk factors for small-for-gestational-age babies: The Auckland Birthweight Collaborative Study. J Paediatr Child Health. 2001, 37: 369-375. 10.1046/j.1440-1754.2001.00684.x.
Bryan SM, Hindmarsh PC: Normal and abnormal fetal growth. Horm Res. 2006, 65 (Suppl 3): 19-27.
Ahluwalia IB, Merritt R, Beck LF, Rogers M: Multiple lifestyle and psychosocial risks and delivery of small for gestational age infants. Obstet Gynecol. 2001, 97: 649-656. 10.1016/S0029-7844(01)01324-2.
Berman L, Moss RL: Necrotizing enterocolitis: an update. Semin Fetal Neonatal Med. 2011, 16: 145-150. 10.1016/j.siny.2011.02.002.
Garite TJ, Clark R, Thorp JA: Intrauterine growth restriction increases morbidity and mortality among premature neonates. Am J Obstet Gynecol. 2004, 191: 481-487. 10.1016/j.ajog.2004.01.036.
Baserga M, Bertolotto C, Maclennan NK, Hsu JL, Pham T, Laksana GS, Lane RH: Uteroplacental insufficiency decreases small intestine growth and alters apoptotic homeostasis in term intrauterine growth retarded rats. Early Hum Dev. 2004, 79: 93-105. 10.1016/j.earlhumdev.2004.04.015.
Xu RJ, Mellor DJ, Birtles MJ, Reynolds GW, Simpson HV: Impact of intrauterine growth retardation on the gastrointestinal tract and the pancreas in newborn pigs. J Pediatr Gastroenterol Nutr. 1994, 18: 231-240. 10.1097/00005176-199402000-00018.
D’Inca R, Kloareg M, Gras-Le Guen C, Le Huerou-Luron I: Intrauterine growth restriction modifies the developmental pattern of intestinal structure, transcriptomic profile, and bacterial colonization in neonatal pigs. J Nutr. 2010, 140: 925-931. 10.3945/jn.109.116822.
Baschat AA, Hecher K: Fetal growth restriction due to placental disease. Semin Perinatol. 2004, 28: 67-80. 10.1053/j.semperi.2003.10.014.
Baschat AA: Fetal responses to placental insufficiency: an update. BJOG. 2004, 111: 1031-1041. 10.1111/j.1471-0528.2004.00273.x.
Gilbert WM, Danielsen B: Pregnancy outcomes associated with intrauterine growth restriction. Am J Obstet Gynecol. 2003, 188: 1596-1599. 10.1067/mob.2003.384. discussion 1599–1601
Aucott SW, Donohue PK, Northington FJ: Increased morbidity in severe early intrauterine growth restriction. J Perinatol. 2004, 24: 435-440. 10.1038/sj.jp.7211116.
Malcolm G, Ellwood D, Devonald K, Beilby R, Henderson-Smart D: Absent or reversed end diastolic flow velocity in the umbilical artery and necrotising enterocolitis. Arch Dis Child. 1991, 66: 805-807. 10.1136/adc.66.7_Spec_No.805.
Bhatt AB, Tank PD, Barmade KB, Damania KR: Abnormal Doppler flow velocimetry in the growth restricted foetus as a predictor for necrotising enterocolitis. J Postgrad Med. 2002, 48: 182-185. discussion 185
Karsdorp VH, Van Vugt JM, Van Geijn HP, Kostense PJ, Arduini D, Montenegro N, Todros T: Clinical significance of absent or reversed end diastolic velocity waveforms in umbilical artery. Lancet. 1994, 344: 1664-1668. 10.1016/S0140-6736(94)90457-X.
Adiotomre PN, Johnstone FD, Laing IA: Effect of absent end diastolic flow velocity in the fetal umbilical artery on subsequent outcome. Arch Dis Child Fetal Neonatal Ed. 1997, 76: F35-F38. 10.1136/fn.76.1.F35.
Dorling J, Kempley S, Leaf A: Feeding growth restricted preterm infants with abnormal antenatal Doppler results. Arch Dis Child Fetal Neonatal Ed. 2005, 90: F359-F363. 10.1136/adc.2004.060350.
Wilson DC, Harper A, McClure G: Absent or reversed end diastolic flow velocity in the umbilical artery and necrotizing enterocolitis. Arch Dis Child. 1991, 66: 1467-
Kamoji VM, Dorling JS, Manktelow B, Draper ES, Field DJ: Antenatal umbilical Doppler abnormalities: an independent risk factor for early onset neonatal necrotizing enterocolitis in premature infants. Acta Paediatr. 2008, 97: 327-331. 10.1111/j.1651-2227.2008.00671.x.
Manogura AC, Turan O, Kush ML, Berg C, Bhide A, Turan S, Moyano D, Bower S, Nicolaides KH, Galan HL: Predictors of necrotizing enterocolitis in preterm growth-restricted neonates. Am J Obstet Gynecol. 2008, 198: 638-e631-635
Lucas A, Cole TJ: Breast milk and neonatal necrotising enterocolitis. Lancet. 1990, 336: 1519-1523. 10.1016/0140-6736(90)93304-8.
Boyd CA, Quigley MA, Brocklehurst P: Donor breast milk versus infant formula for preterm infants: systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2007, 92: F169-F175. 10.1136/adc.2005.089490.
McGuire W, Anthony MY: Donor human milk versus formula for preventing necrotising enterocolitis in preterm infants: systematic review. Arch Dis Child Fetal Neonatal Ed. 2003, 88: F11-F14. 10.1136/fn.88.1.F11.
Sullivan S, Schanler RJ, Kim JH, Patel AL, Trawoger R, Kiechl-Kohlendorfer U, Chan GM, Blanco CL, Abrams S, Cotten CM: An exclusively human milk-based diet is associated with a lower rate of necrotizing enterocolitis than a diet of human milk and bovine milk-based products. J Pediatr. 2010, 156: 562-567. 10.1016/j.jpeds.2009.10.040. e561
Burrin DG, Stoll B: Key nutrients and growth factors for the neonatal gastrointestinal tract. Clin Perinatol. 2002, 29: 65-96. 10.1016/S0095-5108(03)00065-4.
Camara D: Minimizing risks associated with peripherally inserted central catheters in the NICU. MCN Am J Matern Child Nurs. 2001, 26: 17-21. 10.1097/00005721-200101000-00005. quiz 22
Schutzman DL, Porat R, Salvador A, Janeczko M: Neonatal nutrition: a brief review. World J Pediatr. 2008, 4: 248-253. 10.1007/s12519-008-0046-2.
Morgan J, Young L, McGuire W: Delayed introduction of progressive enteral feeds to prevent necrotising enterocolitis in very low birth weight infants. Cochrane Database Syst Rev. 2011, (3): CD001970-
Karagianni P, Briana DD, Mitsiakos G, Elias A, Theodoridis T, Chatziioannidis E, Kyriakidou M, Nikolaidis N: Early versus delayed minimal enteral feeding and risk for necrotizing enterocolitis in preterm growth-restricted infants with abnormal antenatal Doppler results. Am J Perinatol. 2010, 27: 367-373. 10.1055/s-0029-1243310.
Leaf A, Dorling J, Kempley S, McCormick K, Mannix P, Linsell L, Juszczak E, Brocklehurst P, Abnormal Doppler Enteral Prescription Trial Collaborative G: Early or delayed enteral feeding for preterm growth-restricted infants: a randomized trial. Pediatrics. 2012, 129: e1260-e1268. 10.1542/peds.2011-2379.
McClure RJ: Trophic feeding of the preterm infant. Acta Paediatr Suppl. 2001, 90: 19-21.
Lucas A, Bloom SR, Aynsley-Green A: Gut hormones and ‘minimal enteral feeding’. Acta Paediatr Scand. 1986, 75: 719-723. 10.1111/j.1651-2227.1986.tb10280.x.
Berseth CL: Neonatal small intestinal motility: motor responses to feeding in term and preterm infants. J Pediatr. 1990, 117: 777-782. 10.1016/S0022-3476(05)83343-8.
Bombell S, McGuire W: Early trophic feeding for very low birth weight infants. Cochrane Database Syst Rev. 2009, (3): CD000504-
Van Elburg RM, van den Berg A, Bunkers CM, Van Lingen RA, Smink EW, Van Eyck J, Fetter WP: Minimal enteral feeding, fetal blood flow pulsatility, and postnatal intestinal permeability in preterm infants with intrauterine growth retardation. Arch Dis Child Fetal Neonatal Ed. 2004, 89: F293-F296. 10.1136/adc.2003.027367.
Uauy RD, Fanaroff AA, Korones SB, Phillips EA, Phillips JB, Wright LL: Necrotizing enterocolitis in very low birth weight infants: biodemographic and clinical correlates. National Institute of Child Health and Human Development Neonatal Research Network. J Pediatr. 1991, 119: 630-638. 10.1016/S0022-3476(05)82418-7.
Flidel-Rimon O, Friedman S, Lev E, Juster-Reicher A, Amitay M, Shinwell ES: Early enteral feeding and nosocomial sepsis in very low birthweight infants. Arch Dis Child Fetal Neonatal Ed. 2004, 89: F289-F292. 10.1136/adc.2002.021923.
Stoll BJ, Hansen NI, Adams-Chapman I, Fanaroff AA, Hintz SR, Vohr B, Higgins RD, National Institute of Child H, Human Development Neonatal Research N: Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA. 2004, 292: 2357-2365. 10.1001/jama.292.19.2357.
Morgan J, Young L, McGuire W: Slow advancement of enteral feed volumes to prevent necrotising enterocolitis in very low birth weight infants. Cochrane Database Syst Rev. 2011, (3): CD001241-
Salhotra A, Ramji S: Slow versus fast enteral feed advancement in very low birth weight infants: a randomized control trial. Indian Pediatr. 2004, 41: 435-441.
Premji SS, Chessell L: Continuous nasogastric milk feeding versus intermittent bolus milk feeding for premature infants less than 1500 grams. Cochrane Database Syst Rev. 2011, (11): CD001819-
Grant J, Denne SC: Effect of intermittent versus continuous enteral feeding on energy expenditure in premature infants. J Pediatr. 1991, 118: 928-932. 10.1016/S0022-3476(05)82213-9.
Toce SS, Keenan WJ, Homan SM: Enteral feeding in very-low-birth-weight infants. A comparison of two nasogastric methods. Am J Dis Child. 1987, 141: 439-444.
Aynsley-Green A, Adrian TE, Bloom SR: Feeding and the development of enteroinsular hormone secretion in the preterm infant: effects of continuous gastric infusions of human milk compared with intermittent boluses. Acta Paediatr Scand. 1982, 71: 379-383. 10.1111/j.1651-2227.1982.tb09438.x.
Mihatsch WA, Von Schoenaich P, Fahnenstich H, Dehne N, Ebbecke H, Plath C, Von Stockhausen HB, Muche R, Franz A, Pohlandt F: The significance of gastric residuals in the early enteral feeding advancement of extremely low birth weight infants. Pediatrics. 2002, 109: 457-459. 10.1542/peds.109.3.457.
Cobb BA, Carlo WA, Ambalavanan N: Gastric residuals and their relationship to necrotizing enterocolitis in very low birth weight infants. Pediatrics. 2004, 113: 50-53. 10.1542/peds.113.1.50.
Bertino E, Giuliani F, Prandi G, Coscia A, Martano C, Fabris C: Necrotizing enterocolitis: risk factor analysis and role of gastric residuals in very low birth weight infants. J Pediatr Gastroenterol Nutr. 2009, 48: 437-442. 10.1097/MPG.0b013e31817b6dbe.
Harkness UF, Mari G: Diagnosis and management of intrauterine growth restriction. Clin Perinatol. 2004, 31: 743-764. 10.1016/j.clp.2004.06.006. vi
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
GB and EZ conceived the study and has made substantial contributions in drafting manuscript. LM and AS performed literature review and made contributions in drafting manuscript. CR revised the manuscript critically. AP gave a valuable contribution to the revision of the manuscript according to reviewer’s comments. All authors read and approved the final manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Barone, G., Maggio, L., Saracino, A. et al. How to feed small for gestational age newborns. Ital J Pediatr 39, 28 (2013). https://doi.org/10.1186/1824-7288-39-28
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1824-7288-39-28