Abstract
Background
This study aimed to retrospectively investigate our experience of surgical treatment for acute type A aortic dissection in patients older than 70 years.
Methods
From September 2005 to January 2012, eleven patients who were older than 70 years underwent surgical treatment for type A aortic dissection at our center and were included in this study. Total arch replacement was performed in three patients, seven patients underwent subtotal arch replacement and one with single-branched stent graft implantation. One patient underwent a valve-sparing (David) procedure while another underwent a concomitant aortic valve replacement (Wheat procedure). One patient required coronary artery bypass grafting. All operations were performed under deep hypothermic circulatory arrest and selective antegrade cerebral perfusion.
Results
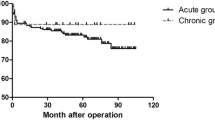
There was one in-hospital death (9.1%) and no operative mortality within 30 days. Cardiopulmonary bypass time, myocardial ischemic time and antegrade cerebral perfusion time accounted for 151.4±33.5 minutes, 68.5±41.4 minutes and 30.3±12.9 minutes, respectively. Overall in-hospital duration, intensive care unit (ICU) time and mean ventilation time were 40.9±40.3 days, 16.5±22.5 days and 90.5±139.4 hours, respectively. New postoperative permanent neurological dysfunction and temporary neurological dysfunction were observed in one patient (9.1%) and in three patients (27.3%), respectively. Mean follow-up was 49.0±19.9 months and nine patients are still alive, one patient died of cancer after 24 months postoperation.
Conclusions
Surgical management for acute type A dissection in patients older than 70 years is a safe alternative with acceptable risk of death and the early and late results are satisfactory.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Although the outcomes of surgical treatment for acute type A aortic dissection have greatly improved in recent years, it is still associated with high mortality and morbidity [1, 2]. Hospital mortality for surgical treatment is reported from 5% to 27.4%. If left untreated or only treated medically, it is estimated to be 65% to 90% in the first two weeks after onset of symptoms [3, 4]. For patients who present with acute uncomplicated type B aortic dissection, in-hospital survival approaches 90% with medical therapy alone [5, 6]. International Registry of Acute Aortic Dissection (IRAD) reported that in-hospital mortality in patients undergoing surgical repair of type B aortic dissection was 29.3% [7]. Additionally, advanced age is an established independent risk factor for early and late mortality and morbidity after surgery for aortic dissection [4, 8]. Therefore, some centers and surgeons suggest taking conservative surgical strategy or medicine to palliate this life-threatening conditoin in elderly patients [9].
However, as life expectancy has been continuing to increase, there are an increasing number of elderly patients with type A aortic dissection [10]. Thus, it is necessary to objectively evaluate the early and late surgical outcomes of acute type A dissection in elderly patients.
In this study, we retrospectively reviewed our experience with patients older than 70 years undergoing open aortic arch reconstruction for type A aortic dissection.
Methods
The study protocol was approved by the Committee for the Protection of Human Subjects at the Zhongshan Hospital Fudan University. Informed consent was obtained from each patient involved in this study.
Patient demographics and characteristics
From September 2005 to January 2012, eleven elderly patients with acute type A aortic dissection underwent surgical treatment at the cardiovascular center of Zhongshan Hospital (Shanghai, China). The mean age of these patients was 72.4±1.4 years, (range, 71–75 years), and six patients were male. Among them, one patient had been transferred to our center for surgical treatment for retrograde type A aortic dissection (RTAD) after endovascular stent graft placement for type B dissection. The most common medical disorder was hypertension, present in all patients. Retrosternal chest pain and back pain were the common presenting symptoms. The diagnosis was based on computed tomography (CT) scanning and echocardiography. The primary intimal tears were located in the ascending aorta in two patients, in the arch in three patients, in the proximal descending aorta in one patient and five patients were inspected with multiple intimal tears. Preoperative patient characteristics are listed in Table 1.
All eleven patients were in the acute phase of type A aortic dissection. Emergency open aortic arch surgery was successfully performed in all of these patients. The indications for open aortic arch reconstruction were the following conditions: (1) primary tear in the large curve of transverse arch or the proximal descending aorta; (2) symptoms of inadequate cerebral perfusion [1, 11]. The patients with severe preoperative neurological dysfunction or those with significant hemodynamic disturbance (shock) were excluded.
Surgical technique
Our approach for open aortic arch reconstruction has been described previously [12, 13]. All patients were performed under general anesthesia and through a standard median sternotomy. The arterial blood pressure of both the upper and lower limbs was monitored. The key techniques for aortic dissection operation included total cardiopulmonary bypass, deep hypothermia, circulatory arrest, and unilateral or bilateral selective cerebral perfusion (SCP). Right axillary artery, or both right axillary artery and right femoral artery were used for arterial perfusion, and the right atrium was cannulated with a single atriocaval cannula. Circulatory arrest was initiated when the nasopharyngeal temperature reached 16-20 degree centigrade. For cerebral protection, we usually use SCP, pharmacologic agents (thiamylal sodium, phenytoin, and mannitol) and ice packs placed around the head. Unilateral SCP was performed through right axillary artery, while bilateral SCP was usually performed through right axillary artery and left common carotid artery. The flow rate and perfusion pressure were maintained at 8 ml/kg/min to 10 ml/kg/min and 40 mmHg to 50 mmHg, respectively. The arch reconstruction strategy was mainly based on intraoperative inspection, including location of primary tear, the extent of tear, texture of vascular wall and situation of of supra-arch vessels. The proximal aortic repair was performed during the systemic rewarming period and based on the surgical inspection of the involvement of the aortic root, including the aortic valve leaflets as well as the coronary ostia.
Data collection and follow-up
Hospital records were retrospectively reviewed for all patients and were entered into a dedicated Microsoft Excel table. Continuous variables were presented as mean±SD, and categorical variables as numbers and percentages. All live patients were followed up by telephone or direct interviews in our outpatient department to evaluate their clinical status.
Results
Operative data
Total arch replacement with a four-branched vascular graft was performed in three patient. One patient underwent total arch reconstruction by using 3-branched Dacron graft combined with a single-branched stent graft. Seven patients underwent subtotal arch replacement with or without 1-branched graft. Six patients were applied with stented elephant implantation, and one patient (retrograde type A aortic dissection, RTAD) with a procedure mimicking the frozen elephant trunk procedure. The intimal tears were identified and resected in all of patients. Due to aortic valve or coronary ostial involvement, a Wheat procedure or coronary artery by-pass grafting (CABG) was performed in two patients. Detailed surgical strategies are summarized in Table 2.
Table 3 summarizes the surgical data, perfusion data, and postoperative ICU information, including cardiopulmonary bypass (CPB) time, myocardial ischemic time, in-hospital time and ventilation time, and drainage on the first postoperative day. These results are comparable to previously reported results on a large sample of type A aortic dissection patients [12].
Blood product usage
Mean blood product usage included packed red blood cells 1740.9±1413.8 ml (range, 600-5800 ml), and serum 1036.4±585.3 ml (range, 200-2000 ml). Seven patients (63.6%) needed platelet transfusion. The human prothrombin complex concentrate (200 IU, Laishi, Shanghai) was used in all the patients.
In-hospital mortality and morbidity
There was one in-hospital death (9.1%), but no operative death within 30 days. The patient who died in hospital was emergently transferred to our department for surgery for RTAD, and she had been in respiratory distress preoperatively. On postoperative day 50, the patient died as a result of multiple organ failure.
One patient was discharged with permanent neurological dysfunction (PND) and paraplegia. Temporary neurological dysfunction (TND) was observed in three patients, and recovered when they were discharged. Six patients had respiratory dysfunction, including severe hypoxemia requiring re-ventilation in one patient, tracheotomy in three patients and mild hypoxemia in two patients. Five patients were successfully weaned from the ventilator after prolonged ventilation periods, except one in-hospital death. Three patients developed renal failure requiring hemodialysis. Two patients had transient elevation of serum creatinine but did not need dialysis. No patient required reoperation to control bleeding. One patient had phlebothrombosis of left leg and recovered after treatment for 11 days (Table 4).
Late mortality and follow-up
The median follow-up was 49.0±19.9 months (19-81 months). Follow-up was 100% complete. One patient died of cancer without cardiac cause at 24 months following aortic dissection surgery. One patient had a stroke and lost the vision in his right eye six years after his surgery. One patient needed to continue diuretics. All live patients were in good state and free form aortic reoperation till the follow-up.
Discussion
Owing to the age-related alteration of physiological reserves, age is recognized as an independent predictor of mortality in patients with acute type A aortic dissection, and any complication during the early postoperative period may compromise the survival of elderly patients [2, 4, 14]. The International Registry of Aortic Dissection (IRAD) has shown that patients aged 70 years or older accounted for 31.6% of patients presenting with type A aortic dissection, and as long as life expectancy increases, this number is bound to increase further [10]. Therefore, much more attention should be paid to elderly patients with type A aortic dissection, including clinical characteristics, therapeutic methods, early and late survival. We reviewed the early and late results for eleven elderly patients with acute type A aortic dissection in this study and reported our experience.
There are still many controversies which have been discussed for many years [8, 10, 15].
First, can elderly patients with acute type A aortic dissection benefit more from surgical repair than medicine alone? Many physicians believe that the risk of a surgical repair is too high in older patients to justify such aggressive approach [9, 10]. However, our results clearly show that acceptable results can be obtained with emergency repair in patients 70 years and older; the overall in-hospital mortality in this study is 9.1%, which is comparable to previous reports of surgery on younger patients (5% to 27.4%) [3, 15, 16]. As demonstrated by IRAD, 70% patients die within 1 week without intervention and 40% die with medical treatment alone [17]. Therefore, advanced age should not be considered an absolute contraindication for surgery of acute type A dissection.
Second, is a conservative surgical strategy more justified in the elderly? We hold the opinion that the object of the operation is not to replace the entire area of involved aorta, but to improve supra-arch vessels perfusion, prevent rupture, and recover the aortic valve normal function. Extended aortic arch resection is usually advocated for youger patients, but not for elderly patients: on one aspect, the tissues of elderly patients are more fragile than those of younger patients; on the other aspect, avoiding the hypothermic circulatory arrest (HCA) and only replacing ascending aorta can indeed decrease the morbidity of neurological and respiratory dysfunction. Kawahito and coworkers [18] reported in their study that the morbidity of renal insufficiency and respiratory dysfuncion were 22% and 25%, respectively, which were much lower than our 45.5% and 54.5%, respectively. However, they reported most elderly patients died of rupture of the residual false lumen in the aortic arch after ascending aorta replacement. In our study, there were no early or late postoperative secondary aortic ruptures. Recently, Chen et al.[11, 19] reported their excellent results with using single- or triple branched stent grafts to extensively repair acute type A aortic dissections with less HCA time.
Thirdly, what kind of cerebral protection strategy is more suitable for elderly patients? Kruger and coworkers [20] reported that HCA alone and antegrade cerebral perfusion (ACP) led to similar result for circulatory arrest time of less than 30 minutes, and for longer arrest time, outcomes with unilateral and bilateral antegrade cerebral perfusion were equivalent. In the elderly patients, atherosclerosis is more common than youger patients. So, avoiding direct cannulation of supra-arch vessels for cerebral perfusion may decrease the incidence of neurological events. In our early stage, we also used bilateral ACP through right axillary artery and left common carotid artery, but now we think that unilateral ACP by right axillary artery combined with HCP may be a good choice for elderly patients.
This study is limited by its retrospective design. This study also represents a single center approach to a relatively small number of patients. As such, unrecognized confounding factors and selection bias may have also affected our outcomes.
Conclusions
In conclusion, surgical repair for acute type A dissection can be performed in patients over 70 years-old with a acceptable risk of death and the early and late results are satisfactory. However, with the development of surgical techniques, minimally invasive cardiac surgeries should be the direction of the management of acute type A aortic dissection in patients older than 70 years.
References
Sun L, Qi R, Zhu J, Liu Y, Zheng J: Total arch replacement combined with stented elephant trunk implantation: a new “standard” therapy for type a dissection involving repair of the aortic arch?. Circulation. 2011, 123: 971-978. 10.1161/CIRCULATIONAHA.110.015081.
Lee WA, Daniels MJ, Beaver TM, Klodell CT, Raghinaru DE, Hess PJ: Late outcomes of a single-center experience of 400 consecutive thoracic endovascular aortic repairs. Circulation. 2011, 123: 2938-2945. 10.1161/CIRCULATIONAHA.110.965756.
Zizza A, Pano M, Zaccaria S, Villani M, Guido M: Outcome of acute type A aortic dissection: single-center experience from 1998 to 2007. J Prev Med Hyg. 2009, 50: 152-158.
Stevens LM, Madsen JC, Isselbacher EM, Khairy P, MacGillivray TE, Hilgenberg AD, Agnihotri AK: Surgical management and long-term outcomes for acute ascending aortic dissection. J Thorac Cardiovasc Surg. 2009, 138: 1349-1357. 10.1016/j.jtcvs.2009.01.030. e1341
Tsai TT, Fattori R, Trimarchi S, Isselbacher E, Myrmel T, Evangelista A, Hutchison S, Sechtem U, Cooper JV, Smith DE, Pape L, Froehlich J, Raghupathy A, Januzzi JL, Eagle KA, Nienaber CA: Long-term survival in patients presenting with type B acute aortic dissection: insights from the International Registry of Acute Aortic Dissection. Circulation. 2006, 114: 2226-31. 10.1161/CIRCULATIONAHA.106.622340.
Szeto WY, McGarvey M, Pochettino A, Moser GW, Hoboken A, Cornelius K, Woo EY, Carpenter JP, Fairman RM, Bavaria JE: Results of a new surgical paradigm: endovascular repair for acute complicated type B aortic dissection. Ann Thorac Surg. 2008, 86: 87-94. 10.1016/j.athoracsur.2008.04.003.
Trimarchi S, Nienaber CA, Rampoldi V, Myrmel T, Suzuki T, Bossone E, Tolva V, Deeb MG, Upchurch GR, Cooper JV, Fang J, Isselbacher EM, Sundt TM, Eagle KA: Role and results of surgery in acute type B aortic dissection: insights from the International Registry of Acute Aortic Dissection (IRAD). Circulation. 2006, 114 (1 suppl): I357-64.
Caus T, Frapier JM, Giorgi R, Aymard T, Riberi A, Albat B, Chaptal PA, Mesana T: Clinical outcome after repair of acute type A dissection in patients over 70 years-old. Eur J Cardiothorac Surg. 2002, 22: 211-217. 10.1016/S1010-7940(02)00275-0.
Neri E, Toscano T, Massetti M, Capannini G, Carone E, Tucci E, Diciolla F, Scolletta S, Morello R, Sassi C: Operation for acute type A aortic dissection in octogenarians: is it justified?. J Thorac Cardiovasc Surg. 2001, 121: 259-67. 10.1067/mtc.2001.112205.
Mehta RH, O’Gara PT, Bossone E, Nienaber CA, Myrmel T, Cooper JV, Smith DE, Armstrong WF, Isselbacher EM, Pape LA, Eagle KA, Gilon D: Acute type A aortic dissection in the elderly: clinical characteristics, management, and outcomes in the current era. J Am Coll Cardiol. 2002, 40: 685-692. 10.1016/S0735-1097(02)02005-3.
Chen LW, Wu XJ, Lu L, Zhang GC, Yang GF, Yang ZW, Dong Y, Cao H, Chen Q: Total arch repair for acute type A aortic dissection with 2 modified techniques: open single-branched stent graft placement and reinforcement of the dissected arch vessel stump with stent graft. Circulation. 2011, 123: 2536-2541. 10.1161/CIRCULATIONAHA.110.008656.
Lu S, Sun X, Hong T, Yang S, Song K, Lai H, Hu K, Wang C: Bilateral versus unilateral antegrade cerebral perfusion in arch reconstruction for aortic dissection. Ann Thorac Surg. 2012, 93: 1917-1920. 10.1016/j.athoracsur.2012.02.090.
Lu S, Lai H, Wang C, Sun X, Hong T, Song K, Yuan Z, Liu X: Surgical treatment for retrograde type A aortic dissection after endovascular stent graft placement for type B dissection. Interact Cardiovasc Thorac Surg. 2012, 14: 538-542. 10.1093/icvts/ivs043.
Patel HJ, Nguyen C, Diener AC, Passow MC, Salata D, Deeb GM: Open arch reconstruction in the endovascular era: analysis of 721 patients over 17 years. J Thorac Cardiovasc Surg. 2011, 141: 1417-1423. 10.1016/j.jtcvs.2011.02.020.
Minakawa M, Fukuda I, Yamauchi S, Watanabe K, Kawamura T, Taniguchi S, Daitoku K, Suzuki Y, Fukui K: Early and long-term outcome of total arch replacement using selective cerebral perfusion. Ann Thorac Surg. 2010, 90: 72-77. 10.1016/j.athoracsur.2010.03.047.
Zierer A, Detho F, Dzemali O, Aybek T, Moritz A, Bakhtiary F: Antegrade cerebral perfusion with mild hypothermia for aortic arch replacement: single-center experience in 245 consecutive patients. Ann Thorac Surg. 2011, 91: 1868-1873. 10.1016/j.athoracsur.2011.02.077.
Tsai TT, Trimarchi S, Nienaber CA: Acute aortic dissection: perspectives from the International Registry of Acute Aortic Dissection (IRAD). Eur J Vasc Endovasc Surg. 2009, 37: 149-159. 10.1016/j.ejvs.2008.11.032.
Kawahito K, Adachi H, Yamaguchi A, Ino T: Early and late surgical outcomes of acute type A aortic dissection in patients aged 75 years and older. Ann Thorac Surg. 2000, 70: 1455-1459. 10.1016/S0003-4975(00)01934-2.
Chen LW, Dai XF, Lu L, Zhang GC, Cao H: Extensive primary repair of the thoracic aorta in acute type a aortic dissection by means of ascending aorta replacement combined with open placement of triple-branched stent graft: early results. Circulation. 2010, 122: 1373-1378. 10.1161/CIRCULATIONAHA.110.946012.
Kruger T, Weigang E, Hoffmann I, Blettner M, Aebert H: Cerebral protection during surgery for acute aortic dissection type A: results of the German Registry for Acute Aortic Dissection Type A (GERAADA). Circulation. 2011, 124: 434-443. 10.1161/CIRCULATIONAHA.110.009282.
Acknowledgements
This work is supported by National Natural Science Foundation of China (grant 81000105) and National “Twelfth Five-Year” Plan for Science & Technology Support (grant 2011BAI11B20).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
JYZ and SYL carried out data collection, and drafted the manuscript. XNS and SGY participated in the operations and helped in drafting the manuscript. TH and HL carried out data analysing and helped in revising the manuscript critically. CSW did the operations, conceived of the study, and helped in revising the manuscript critically. All authors read and approved the final manuscript.
Jiayu Zheng, Shuyang Lu contributed equally to this work.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Zheng, J., Lu, S., Sun, X. et al. Surgical management for acute type A aortic dissection in patients over 70 years-old. J Cardiothorac Surg 8, 78 (2013). https://doi.org/10.1186/1749-8090-8-78
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1749-8090-8-78