Abstract
Background
Severe obesity is associated with important morbidity and increased mortality. The successes of lifestyle modifications and drug therapy have been partial and mostly unsustained in reducing obesity and its comorbidities. Bariatric surgery, particularly biliopancreatic diversion with duodenal switch reduces efficiently excess body weight and improves metabolic and cardiovascular functions.
Case presentation
A 56-year-old man with severe clinical obesity underwent a biliopancreatic diversion with a duodenal switch after unsuccessful treatment with weight loss pharmacotherapy. He had diabetes, hypertension and sleep apnea syndrome and was on three medications for hypertension and two hypoglycemic agents in addition to > 200 insulin units daily. Eleven months after the surgery, he had lost 40% of his body weight. The lipid profile showed great improvement and the hypertension and diabetes were more easily controlled with no more insulin needed. The pseudonormalized pattern of left ventricular diastolic function improved and ventricular walls showed decreased thickness.
Conclusion
Biliopancreatic diversion may bring metabolic and cardiovascular benefits in severely obese patients from a cardiovascular perspective.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Case presentation
A 56-year-old man was referred for biliopancreatic diversion with a duodenal switch (BPD-DS) for intractable complications associated with morbid obesity. He had been unable to lose weight with orlistat 120 mg three times a day for three months. The patient had diabetes mellitus for twenty years associated with hypertension, "mal perforant" and hepatic steatosis. He had all features of the metabolic syndrome and was treated for sleep apnea with a nocturnal continuous positive airway pressure device (C-PAP). His body mass index (BMI) at the time of the surgery was 48.7 kg/m2, weighting 157.7 kg.
The patient's blood tests showed normal electrolytes and a creatinine of 110 μmol/L. The hemoglobin level was 134 g/L, white blood cell and platelet counts were normal. The glycated hemoglobin was 7.1% (normal range 4.4–6.5%) with fasting glucose values ranging from 7 to 11 mmol/L. A 24-hour blood pressure monitoring was normal under medication. His total cholesterol was 4.41 mmol/L, the triglyceride level was 1.74 mmol/L with LDL-cholesterol and HDL-cholesterol levels of 2.63 and 0.99 mmol/L respectively. The total cholesterol/HDL ratio was 4.45. Rest and exercise electrocardiograms were normal as well as a cardiac dobutamine stress echocardiography. A pseudonormalized pattern of left ventricular filling was present on a standard echocardiogram and a 24-hour Holter was normal except for a slight decrease in heart rate variability. His medications before surgery consisted of metformin 850 mg TID, rosiglitazone 8 mg daily, irbesartan 300 mg daily, diltiazem 120 mg daily, orlistat 120 mg TID and furosemide 20 mg every other day. He was on insulin Humalog TID (42–46 U) with insulin NPH 90 U at bed time, for a total of > 200 U of insulin daily.
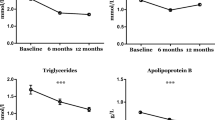
He underwent a modified Scoparino's biliopancreatic diversion with a duodenal switch [1–5]. Appendicectomy and cholecystectomy were concurrently performed. The patient had an hemodynamically stable pulmonary emboli on the day 12 after surgery and was anticoagulated. Otherwise he had no other complication. Anthropometric measurements before and eleven months after the surgery are presented in the Table 1 and Figure 1 and metabolic improvements and echocardiographic findings are depicted in Tables 2 and 3 respectively. Eleven months after the surgery, the medication consisted of metformin 850 mg TID, irbesartan 150 mg daily, 50 000 U of vitamin D2, ferrous sulfate 300 mg daily, 25 000 U of vitamin A, calcium 500 mg and one tablet of vitamins and mineral supplements daily (Centrum Forte®). No insulin was needed anymore to control his metabolic profile.
Discussion
Obesity is associated with an increased risk of coronary artery disease (CAD) and mortality [6–8]. Morbidity and mortality rates rise proportionally to the degree of obesity in men and women and the impact of excess body fat is more significant in younger subjects than older ones [9–12]. In a 10-year follow-up, men and women with a BMI ≥ 35.0 kg/m2 had a relative increased risk of developing diabetes of ~23 and ~17 fold respectively compared to a control group with a BMI between 18.5 and 24.9 kg/m2 [13]. Independently of the BMI, the relative risk of developing diabetes mellitus increases with weight gain as shown in the Nurse's Health Study [14]. Moreover, in that study, women who voluntary lost more than 5.0 kg reduced their risk of diabetes by 50%. Weight loss also lowers blood pressure. In a 3-year follow-up of non-morbidly obese patients with a mean BMI of 31 kg/m2, patients who maintained a 4.5 kg weight loss had a relative risk of hypertension of 0.35 or, a reduction of 0.45 mmHg in systolic blood pressure and 0.35 mmHg in diastolic pressure per kg of weight lost [15].
Heart function is directly influenced by excess body fat [16]. In addition to higher cardiac output in obese patients, left ventricular volume and filling pressures are higher than normal. This usually results in the development of left ventricular strain, which leads to hypertrophy, often of the eccentric type [17, 18]. Left ventricular diastolic function is thus frequently impaired [17, 19].
Weight loss has a beneficial impact on the functional and the structural cardiac status. In a study of obese patients with a mean BMI of 32.7 kg/m2, weight loss of 8 kg over a period of 25 weeks was associated with a significant decrease in left ventricular mass [20]. Weight loss lowers oxygen consumption at any given work rate, decreases cardiac output and blood pressure while left ventricular filling pressures decreased as left ventricular stroke volume diminishes [21, 22]. In a study of obese patients with a BMI > 40 kg/m2 in whom surgical weight loss with vertical gastric banding (VGB) induced a decrease in body weight of 20% at six months, left ventricular wall thickness, particularly the septal and posterior walls, decreased [23].
The National Institutes of Health (NIH) suggested that surgical therapy be proposed to those patients with a BMI level > 40 kg/m2 or > 35 kg/m2 with serious medical conditions including hypertension and obstructive sleep apnea [24]. Surgical intervention, when indicated, brings significant improvement such as a decrease in excess weight and comorbidities; these include hypertension, diabetes, dyslipidemia [3, 14, 25–28] and sleep-related disorders [18, 29]. One can expect a mean reduction of 60 to 75% of excess body weight with biliopancreatic diversion which can persist for 4 to 8 years after surgery [3–5, 30, 31]. The duodenal switch operation, introduced by Hess in 1988 [5], variant of the biliopancreatic diversion of Scopinaro [1, 2], helps in preserving normal eating habits, and the majority of patients undergoing the procedure will have normalization of glucose levels, triglyceride levels and blood pressure early weeks after the surgery [3–5]. Indeed, in a review of 440 obese patients (mean weight of 183 kg) who underwent biliopancreatic diversion with duodenal switch, all of the 36 type 2 diabetic patients discontinued their medication over a 7-year follow-up period [5]. Operative mortality is between 0.5% and 2% [3, 5, 30, 32] and early complications include pulmonary embolus (0.5%) and anastomotic leaks (1–2.5%) [3, 4, 32, 33]. Late complications presents in the form of anemia, anastomotic ulcerations, bone demineralization, neurological complications and protein malabsorption; all of which can be addressed with appropriate supplements. Moreover, significant nutritional and metabolic complications may be less frequent than previously thought [30]. Surgical revisions are needed in 0.1% to 4% of cases [3, 5].
Eleven months after the surgery, our patient had lost 40% of his body weight, and body fat mass was reduced by 41 % (Figure 1). The medication was greatly lightened while the patient maintained fasting glucose values ranging from 5 to 7 mmol/L and a blood pressure less than 130/80 mmHg (Table 2). Indeed, rosiglitazone was discontinued, the insulin that averaged > 200 U daily was no more necessary, diltiazem was discontinued and the dose of irbesartan was halved. The 25% decreased in waist circumference is probably clinically significant [34, 35] albeit waist circumference may be less reliable in patients with a BMI > 35 kg/m2 [36]. Finally, sleep apnea syndrome improved as the patient was no longer on C-PAP.
Left ventricle hypertrophy is recognized as a strong independent risk factor for cardiovascular morbidity and death and changes in cardiac structure following surgical weight loss have been observed [37, 38]. In the present case, the left ventricle mass index decreased by 15% and the thickness of the septal and posterior walls of the left ventricle were reduced (Table 3). Moreover, using Doppler mitral flow velocity with the E/A ratio, we demonstrated that left ventricular diastolic dysfunction actually improved. Before the operation, the E/A ratio was higher than 1 with a significant decrease during the Valsalva maneuver which corresponds to a pseudonormal ventricular filling or grade 2 filling pattern [39, 40]. After the operation, the E/A ratio was smaller than 1 indicating a delayed relaxation of grade 1 filling pattern, representing an improvement in the diastolic function [39, 41] (Table 4).
This case report emphasizes the improvement in cardiovascular parameters, including the diastolic function (demonstrated by a pseudonormal ventricular filling or grade 2 filling pattern) and sleep apnea syndrome, following weight loss-induced by the biliopancreatic diversion with duodenal switch.
Abbreviations
- BPD-DS:
-
biliopancreatic diversion with a duodenal switch
- C-PAP:
-
continuous positive airway pressure device
- BMI:
-
body mass index
- VGB:
-
vertical gastric banding
- NIH:
-
National Institutes of Health
- E/A ratio:
-
early/atrial transmitral filling velocity
References
Scopinaro N, Gianetta E, Civalleri D, Bonalumi U, Bachi V: Bilio-pancreatic bypass for obesity: II. Initial experience in man. Br J Surg. 1979, 66: 618-620.
Scopinaro N, Gianetta E, Civalleri D, Bonalumi U, Bachi V: Two years of clinical experience with biliopancreatic bypass for obesity. Am J Clin Nutr. 1980, 33: 506-514.
Marceau P, Hould FS, Simard S, Lebel S, Bourque RA, Potvin M, Biron S: Biliopancreatic diversion with duodenal switch. World J Surg. 1998, 22: 947-954. 10.1007/s002689900498.
Marceau P, Hould FS, Potvin M, Lebel S, Biron S: Biliopancreatic diversion (duodenal switch procedure). Eur J Gastroenterol Hepatol. 1999, 11: 99-103.
Hess DS, Hess DW: Biliopancreatic diversion with a duodenal switch. Obes Surg. 1998, 8: 267-282. 10.1381/096089298765554476.
Poirier P, Eckel RH: Obesity and cardiovascular disease. Curr Atheroscler Rep. 2002, 4: 448-453.
Allison DB, Fontaine KR, Manson JE, Stevens J, VanItallie TB: Annual deaths attributable to obesity in the United States. JAMA. 1999, 282: 1530-1538. 10.1001/jama.282.16.1530.
Drenick EJ, Bale GS, Seltzer F, Johnson DG: Excessive mortality and causes of death in morbidly obese men. JAMA. 1980, 243: 443-445. 10.1001/jama.243.5.443.
Manson JE, Willett WC, Stampfer MJ, Colditz GA, Hunter DJ, Hankinson SE, Hennekens CH, Speizer FE: Body weight and mortality among women. N Engl J Med. 1995, 333: 677-685. 10.1056/NEJM199509143331101.
Stevens J, Cai J, Pamuk ER, Williamson DF, Thun MJ, Wood JL: The effect of age on the association between body-mass index and mortality. N Engl J Med. 1998, 338: 1-7. 10.1056/NEJM199801013380101.
Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath C.W.,Jr: Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999, 341: 1097-1105. 10.1056/NEJM199910073411501.
Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH: The disease burden associated with overweight and obesity. JAMA. 1999, 282: 1523-1529. 10.1001/jama.282.16.1523.
Field AE, Coakley EH, Must A, Spadano JL, Laird N, Dietz WH, Rimm E, Colditz GA: Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Arch Intern Med. 2001, 161: 1581-1586. 10.1001/archinte.161.13.1581.
Colditz GA, Willett WC, Rotnitzky A, Manson JE: Weight gain as a risk factor for clinical diabetes mellitus in women. Ann Intern Med. 1995, 122: 481-486.
Stevens VJ, Obarzanek E, Cook NR, Lee IM, Appel LJ, Smith West D., Milas NC, Mattfeldt-Beman M, Belden L, Bragg C, Millstone M, Raczynski J, Brewer A, Singh B, Cohen J: Long-term weight loss and changes in blood pressure: results of the Trials of Hypertension Prevention, phase II. Ann Intern Med. 2001, 134: 1-11.
Alpert MA, Hashimi MW: Obesity and the heart. Am J Med Sci. 1993, 306: 117-123.
Ku CS, Lin SL, Wang DJ, Chang SK, Lee WJ: Left ventricular filling in young normotensive obese adults. Am J Cardiol. 1994, 73: 613-615. 10.1016/0002-9149(94)90347-6.
Poirier P, Eckel RH: The heart and obesity. Hurst's The Heart. Edited by: FusterV, AlexanderRW, KingS, O'RourkeRA, RobertsR and WellensHJJ. 2000, New York, McGraw-Hill Companies, 83: 2289-2303. 10
Alpert MA, Lambert CR, Panayiotou H, Terry BE, Cohen MV, Massey CV, Hashimi MW, Mukerji V: Relation of duration of morbid obesity to left ventricular mass, systolic function, and diastolic filling, and effect of weight loss. Am J Cardiol. 1995, 76: 1194-1197. 10.1016/S0002-9149(99)80338-5.
MacMahon SW, Wilcken DE, Macdonald GJ: The effect of weight reduction on left ventricular mass. A randomized controlled trial in young, overweight hypertensive patients. N Engl J Med. 1986, 314: 334-339.
Backman L, Freyschuss U, Hallberg D, Melcher A: Cardiovascular function in extreme obesity. Acta Med Scand. 1973, 193: 437-446.
Backman L, Freyschuss U, Hallberg D, Melcher A: Reversibility of cardiovascular changes in extreme obesity. Effects of weight reduction through jejunoileostomy. Acta Med Scand. 1979, 205: 367-373.
Kanoupakis E, Michaloudis D, Fraidakis O, Parthenakis F, Vardas P, Melissas J: Left ventricular function and cardiopulmonary performance following surgical treatment of morbid obesity. Obes Surg. 2001, 11: 552-558. 10.1381/09608920160556715.
NIH conference. Gastrointestinal surgery for severe obesity. Consensus Development Conference Panel. Ann Intern Med. 1991, 115: 956-961.
Livingston EH: Obesity and its surgical management. Am J Surg. 2002, 184: 103-113. 10.1016/S0002-9610(02)00914-5.
Sjostrom CD, Peltonen M, Wedel H, Sjostrom L: Differentiated long-term effects of intentional weight loss on diabetes and hypertension. Hypertension. 2000, 36: 20-25.
Sileo F, Bonassi U, Bolognini C, Miglioranzi A, Possenti A, Svanoni F, Tengattini F, Tentorio A, Pagani G: [Biliopancreatic bypass in the treatment of severe obesity: long-term clinical, nutritional and metabolic evaluation]. Minerva Gastroenterol Dietol. 1995, 41: 149-155.
Noya G, Cossu ML, Coppola M, Tonolo G, Angius MF, Fais E, Ruggiu M: Biliopancreatic diversion preserving the stomach and pylorus in the treatment of hypercholesterolemia and diabetes type II: results in the first 10 cases. Obes Surg. 1998, 8: 67-72. 10.1381/096089298765555088.
Scheuller M, Weider D: Bariatric surgery for treatment of sleep apnea syndrome in 15 morbidly obese patients: long-term results. Otolaryngol Head Neck Surg. 2001, 125: 299-302. 10.1067/mhn.2001.119139.
Anthone GJ, Lord RV, DeMeester TR, Crookes PF: The duodenal switch operation for the treatment of morbid obesity. Ann Surg. 2003, 238: 618-627. 10.1097/01.sla.0000090941.61296.8f.
Baltasar A, Bou R, Bengochea M, Arlandis F, Escriva C, Miro J, Martinez R, Perez N: Duodenal switch: an effective therapy for morbid obesity--intermediate results. Obes Surg. 2001, 11: 54-58. 10.1381/096089201321454114.
Scopinaro N, Adami GF, Marinari GM, Gianetta E, Traverso E, Friedman D, Camerini G, Baschieri G, Simonelli A: Biliopancreatic diversion. World J Surg. 1998, 22: 936-946. 10.1007/s002689900497.
Byrne TK: Complications of surgery for obesity. Surg Clin North Am. 2001, 81: 1181-viii.
Lemieux I, Pascot A, Couillard C, Lamarche B, Tchernof A, Almeras N, Bergeron J, Gaudet D, Tremblay G, Prud'homme D, Nadeau A, Despres JP: Hypertriglyceridemic waist: A marker of the atherogenic metabolic triad (hyperinsulinemia; hyperapolipoprotein B; small, dense LDL) in men?. Circulation. 2000, 102: 179-184.
St Pierre J, Lemieux I, Vohl MC, Perron P, Tremblay G, Despres JP, Gaudet D: Contribution of abdominal obesity and hypertriglyceridemia to impaired fasting glucose and coronary artery disease. Am J Cardiol. 2002, 90: 15-18. 10.1016/S0002-9149(02)02378-0.
Poirier P, Despres JP: Waist circumference, visceral obesity, and cardiovascular risk. J Cardiopulm Rehabil. 2003, 23: 161-169. 10.1097/00008483-200305000-00001.
Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP: Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med. 1990, 322: 1561-1566.
Himeno E, Nishino K, Nakashima Y, Kuroiwa A, Ikeda M: Weight reduction regresses left ventricular mass regardless of blood pressure level in obese subjects. Am Heart J. 1996, 131: 313-319.
Poirier P, Bogaty P, Garneau C, Marois L, Dumesnil JG: Diastolic dysfunction in normotensive men with well-controlled type 2 diabetes: importance of maneuvers in echocardiographic screening for preclinical diabetic cardiomyopathy. Diabetes Care. 2001, 24: 5-10.
Poirier P, Bogaty P, Philippon F, Garneau C, Fortin C, Dumesnil JG: Preclinical diabetic cardiomyopathy: relation of left ventricular diastolic dysfunction to cardiac autonomic neuropathy in men with uncomplicated well-controlled type 2 diabetes. Metabolism. 2003, 52: 1056-1061. 10.1016/S0026-0495(03)00091-X.
Rakowski H, Appleton C, Chan KL, Dumesnil JG, Honos G, Jue J, Koilpillai C, Lepage S, Martin RP, Mercier LA, O'Kelly B, Prieur T, Sanfilippo A, Sasson Z, Alvarez N, Pruitt R, Thompson C, Tomlinson C: Canadian consensus recommendations for the measurement and reporting of diastolic dysfunction by echocardiography: from the Investigators of Consensus on Diastolic Dysfunction by Echocardiography. J Am Soc Echocardiogr. 1996, 9: 736-760.
Guidelines from the Canadian Cardiovascular Society and the Canadian Hypertension Society on the echocardiographic determination of left ventricular mass. Task Force of the Echocardiography Section. Can J Cardiol. 1995, 11: 391-395.
Acknowledgement
The authors want to express their gratitude to Suzie Laroche, Louise Marois and Claudette Fortin for the quality of their intervention and the work on this particular population. Written consent was obtained from the patient for publication of the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared.
Authors' contributions
PP envisioned the paper and PW, PP prepared the initial draft of the article. The other authors critically revised the manuscript for important intellectual content. All authors read and approved the final version of the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Woods, P., Paquette, C., Martin, J. et al. Metabolic and cardiovascular improvements after biliopancreatic diversion in a severely obese patient. Cardiovasc Diabetol 3, 5 (2004). https://doi.org/10.1186/1475-2840-3-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1475-2840-3-5