Abstract
Background
Pancreatico-biliary adenocarcinomas (PBA) have a poor prognosis. Diagnosis is usually achieved by imaging and/or endoscopy with confirmatory cytology. Cytological interpretation can be difficult especially in the setting of chronic pancreatitis/cholangitis. Immunohistochemistry (IHC) biomarkers could act as an adjunct to cytology to improve the diagnosis. Thus, we performed a meta-analysis and selected KOC, S100P, mesothelin and MUC1 for further validation in PBA resection specimens.
Methods
Tissue microarrays containing tumour and normal cores in a ratio of 3:2, from 99 surgically resected PBA patients, were used for IHC. IHC was performed on an automated platform using antibodies against KOC, S100P, mesothelin and MUC1. Tissue cores were scored for staining intensity and proportion of tissue stained using a Histoscore method (range, 0–300). Sensitivity and specificity for individual biomarkers, as well as biomarker panels, were determined with different cut-offs for positivity and compared by summary receiver operating characteristic (ROC) curve.
Results
The expression of all four biomarkers was high in PBA versus normal ducts, with a mean Histoscore of 150 vs. 0.4 for KOC, 165 vs. 0.3 for S100P, 115 vs. 0.5 for mesothelin and 200 vs. 14 for MUC1 (p < .0001 for all comparisons). Five cut-offs were carefully chosen for sensitivity/specificity analysis. Four of these cut-offs, namely 5%, 10% or 20% positive cells and Histoscore 20 were identified using ROC curve analysis and the fifth cut-off was moderate-strong staining intensity. Using 20% positive cells as a cut-off achieved higher sensitivity/specificity values: KOC 84%/100%; S100P 83%/100%; mesothelin 88%/92%; and MUC1 89%/63%. Analysis of a panel of KOC, S100P and mesothelin achieved 100% sensitivity and 99% specificity if at least 2 biomarkers were positive for 10% cut-off; and 100% sensitivity and specificity for 20% cut-off.
Conclusion
A biomarker panel of KOC, S100P and mesothelin with at least 2 biomarkers positive was found to be an optimum panel with both 10% and 20% cut-offs in resection specimens from patients with PBA.
Similar content being viewed by others
Background
Pancreatic ductal adenocarcinoma (PDAC) is the fifth most common cause of cancer death in the UK with a 5-year survival of only 2% [1]. This poor prognosis is partly due to late clinical presentation with advanced disease, when the treatment options are limited and relatively ineffective [2]. Surgical resection is the only curative option but is only available to 15-20% patients with localised disease [3, 4]. The remainder with locally advanced and/or metastatic disease are offered palliative chemotherapy, radiotherapy and/or best supportive management [2, 3]. Adenocarcinomas of the head of pancreas and extra-hepatic cholangiocarcinomas (CCC) present similarly most often with jaundice, pain or weight loss [5]. Morphological similarities in addition to generally poor prognosis for both diseases enable PDAC to be grouped with extrahepatic CCC to form so-called pancreatico-biliary adenocarcinomas (PBA).
Diagnosis of PBA relies upon a combination of radiological and cytology or pathology findings [6–10]. Confirmatory tissue diagnosis is necessary before chemotherapy or radiotherapy treatment, however a biopsy specimen is not always required for resection when the suspicion of cancer is high; as generally, the resection will provide therapeutic benefit, and substantially delaying surgery to confirm a diagnosis may deny potentially curative treatment [9, 11–15].
Endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) is normally used to obtain cytological samples from pancreatic mass lesions, while endoscopic retrograde cholangio-pancreato-graphy (ERCP) biliary brushings are used for cytology collection from strictures of pancreatico-biliary (PB) ducts [16–18]. Cytological analysis requires the distinction of malignant PB epithelial cells from reactive pancreatic and bile duct cells as well as other gastrointestinal contaminants. This task requires tremendous expertise and can be difficult for both quantitative and qualitative reasons [19]. Quantitatively, the cytological sample obtained may be of low cellularity with few, or even no malignant epithelial cells amongst a variety of cell types. Qualitatively, PBA cells can be morphologically similar to reactive PB cells, especially in well-differentiated adenocarcinomas. Chronic reactive changes arising from atrophy or inflammation in pancreatitis or cholangitis are common, and also make diagnosis of adenocarcinoma difficult.
Expressing these issues statistically, the reported sensitivity of EUS-FNA ranges from 78%-95% with specificity reported to be 75-100% [17, 18, 20–25]. Though the specificity of biliary brush cytology is high, the sensitivity can be low with ranges of 46% to 73% reported [10, 16, 26, 27]. The sensitivity of EUS-FNA cytology decreases to 62% in chronic pancreatitis and to only 50% in cases of chronic pancreatitis with obstructive jaundice [28]. Thus, a tissue diagnosis is not achieved in a significant proportion of PBA cases. Hence, an unmet clinical need exists for the diagnosis of PBA from cytological samples obtained at EUS-FNA and ERCP.
One potential way of improving cytological diagnosis is to use immunohistochemical (IHC) biomarkers as an adjunct to cytology in difficult to diagnose cases. IHC is a technique widely used in diagnostic pathology that enables the observation and localisation of protein expression simultaneously in tissue and cellular compartments [29]. Diagnostic IHC biomarkers have been investigated both as single biomarkers and as part of biomarker panels to improve the diagnosis of PDAC, but to date none has entered into routine clinical practice [30–37]. We performed a meta-analysis of potential PDAC IHC diagnostic biomarkers [38] aiming to generate a list of biomarkers assessed in either surgical or cytology specimens, where PDAC was compared with normal pancreas and/or chronic pancreatitis. Meta-analytical results showed KOC, S100P, mesothelin and MUC1 to be high-ranking candidates. These biomarkers have not entered into routine clinical practice partly because they were investigated in separate studies with relatively small sample sizes and without uniform and clinically appropriate thresholds for positivity.
We sought to investigate the utility of these four candidate biomarkers in the characterisation of PBA, including both PDAC and CCC. CCC has been included because it often enters the clinical and pathological differential diagnosis; and its positive biomarkers are generally shared with PDAC [39–42]. The aim was to identify a clinically useful diagnostic biomarker or panel of biomarkers with a robust cut-off for positivity that could potentially be taken forward for validation in PBA cytology samples.
A biomarker panel of KOC, S100P and mesothelin with at least 2 biomarkers positive was found to be an optimum panel with both 10% and 20% cut-off achieving almost 100% sensitivity and specificity in resection specimens from patients with PBA.
Methods
Tissue Microarrays
Histological sections from tissue microarrays (TMAs) containing samples from 99 surgically resected PBA patients (PDAC = 85, CCC = 14) were used for IHC. All resectional surgery was performed in the West of Scotland Pancreatic Unit, Glasgow Royal Infirmary, UK, during a 10-year period (1st June 1995 to 31st July 2004). Formalin fixed paraffin embedded (FFPE) tumour specimens were archived in the Department of Pathology, Glasgow Royal Infirmary and were used for the construction of TMAs. The construction and use of these TMAs has been previously described [43]. Ethical approval has been granted by the North Glasgow University Hospitals NHS Trust Ethics Committee and by the National Health Service Greater Glasgow and Clyde Ethics Committee. This ethics approval includes the use of archival pathology specimens, where the patients were not given the opportunity to donate their tissue. These TMAs contain five tissue cores (3 tumours and 2 normal) for each patient. Tumour cores are adenocarcinoma cores from PBA patients, whereas normal cores are from adjacent normal pancreatic ducts and acini.
Immunohistochemistry
IHC was performed for KOC, S100P, mesothelin and MUC1 on our TMA cohort, on an automated platform. Details of the antibodies, antibody concentrations and IHC conditions are shown in Table 1.
Scoring of tissue specimens
Stained TMA sections were scanned (Hamamatsu Slide Scanner) and images uploaded in Distiller 2.2 (Leica Biosystems). Microscopic analysis was undertaken blinded to diagnosis or other parameters. IHC staining of all cores was assessed by one author (AA); a second author (KAO) double-scored approximately 15% of cores, in a blinded fashion, as audit. All scores were exported in an Excel spreadsheet from Distiller 2.2 for analysis. A semi-quantitative Histoscore [0 ×% negative cells + 1 ×% weakly stained cells + 2 ×% moderately stained cells + 3 ×% strongly stained cells] was generated for statistical analysis. This Histoscore thus has a range of possible scores between 0 and 300.
Statistics and data analysis
The mean expression of each biomarker in the PBA tumour cores was compared with the mean expression in normal tissue cores. Statistical significance was calculated using the independent sample t-test to generate the p value. The independent sample t test was used rather than the paired sample t test because a full set of matching tumour and normal tissue cores was not available for approximately 5% of patients. This was due to loss of tissue cores during processing, which is expected in a proportion of samples. Sensitivity/specificity analyses were carried out for biomarkers, both individually and in panels of 2–4 biomarkers, and compared. We used two different panel approaches for sensitivity/specificity analysis. One approach assigns the case into the positive category if the tumour expresses only one biomarker in the panel. The other approach assigns the case into the positive category if the tumour shows staining for at least 2 biomarkers in the panel.
A combined summary receiver operating characteristic (SROC) curve was generated to compare different panels of biomarkers. P value <0.05 was considered statistically significant. SPSS-19 and RevMan-5.1 were used for statistical analysis.
Results
We first performed IHC for each of the four biomarkers on microarrays of normal and tumour tissue from patients with PBA. To fully assess the clinical usefulness of these biomarkers we wanted to analyse the expression of all four biomarkers in PBA versus normal tissue. Moreover, by combining various biomarkers in panels, we hypothesised that we would be able to determine the combination of biomarkers that would deliver the best diagnostic sensitivity and specificity.
Staining characteristics of biomarkers
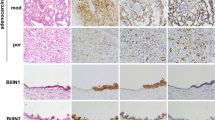
For each marker assessed in the PB TMAs, IHC staining was seen only in epithelial cells. As expected, KOC expression was observed in the cytoplasm; S100P was expressed in the cytoplasm and nucleus, while mesothelin and MUC1 expression was cytoplasmic and membranous (Figure 1). In general, we observed moderate to strong intensity of staining for KOC, mesothelin, S100P and MUC1 in PBA. Moreover, for all four biomarkers we observed significantly higher expression in tumour versus normal tissue (non-neoplastic ducts or pancreatic acinar tissue). The mean percentage positivity for biomarkers in tumour vs. normal tissue was as follows: for KOC 74% vs. 0.4%; for S100P 75% vs. 0.3%; for mesothelin 75% vs. 4%; and for MUC1 75% vs. 18% (Table 2, p < 0.0001 for all tumour vs. normal comparisons). When scored simply as the percentage of positive staining cells per tumour core, we observed similar results for all four biomarkers in tumour tissue. As shown in Table 2, the mean percentage of positive carcinoma cells in tumour tissue was 74% for KOC, 75% for S100P, 73% for mesothelin and 75% for MUC1.
By employing a Histoscore scoring method, which takes into account both the extent of expression across the tissue core, and the staining intensity, we were able more to perform a more comprehensive analysis of our biomarkers. Utilizing this method to score the degree and intensity of staining revealed variance of expression of the different biomarkers. As shown in Table 2, the mean tumour tissue versus mean normal tissue Histoscore for MUC1 was 193 vs. 48, while for S100P, KOC and mesothelin, the mean tumour tissue versus mean normal tissue Histoscores were 165 vs. 0.3, 150 vs. 0.5 and 115 vs. 4 respectively.
Although one biomarker, MUC1, was expressed in normal tissue as evidenced by the mean percentage positivity of 16% of normal cells in normal tissues, the expression of the other three biomarkers was very low in normal tissue (Table 2). Furthermore, there were no significant differences in biomarker expression between normal ducts only and normal ducts and acini together (see Additional file 1). Thus, IHC staining using these markers could greatly facilitate interpretation of cytology samples.
Biomarkers expression was also assessed in PDAC compared to CCC as shown in Additional file 2. The expression of all four biomarkers is similar in PDAC and CCC and thus there is no statistically significant difference in the mean expression of biomarkers between these two tumour types (p > 0.05, independent sample t test). Therefore, for sensitivity and specificity analyses PDAC and CCC were grouped as PBA.
Sensitivity and specificity analysis
Establishing cut-offs from ROC curve analysis
The sensitivity and specificity of these four biomarkers were evaluated using five cut-offs (thresholds) for positivity as follows: 5% positive cells of any staining intensity; 10% positive cells of any staining intensity; 20% positive cells of any staining intensity; moderate or strong staining of any cells; and Histoscore ≥20. Three of these cut-offs were based on percentage of positive cells and identified by ROC curve analysis. The sensitivity of each biomarker was plotted against 1 – specificity, and ROC curves with coordinates were generated for all four biomarkers (Figure 2). The area under the curve was 0.93 (0.88-0.97, 95% CI) for KOC, 0.92 (0.85-0.99, 95% CI) for S100P, 0.95 (0.92-0.99, 95% CI) for mesothelin, and 0.87 (0.81-0.93, 95% CI) for MUC1. Based on percentage of positive cells in the tumour compared with normal cores, ROC curve analysis allowed us to assess potential cut-offs, from 5% positive cells to 95% positive cells, with their corresponding sensitivity and specificity values for all four biomarkers (Figure 2 and Additional file 3). Three best cut-offs; 5%; 10% or 20% of positive cells of any staining intensity were selected based on their sensitivity and specificity values.
The fourth cut-off was based on moderate to strong staining intensity (+2/+3 staining) in any of the cells. This was selected as moderate to strong staining was expected to be easily interpreted by pathologists. Interestingly, cases with +2/+3 staining for all four biomarkers have more than 20% cells positive for each of the four biomarkers. Indeed patients with +2/+3 staining have only 5 cases with less than 50% of cells positive for MUC1, 2 cases in which KOC was expressed in fewer than 50% of cells, and only 1 case each for mesothelin and S100P staining with less than 50% positivity.
The fifth cut-off was based on a Histoscore value of 20 (HS20), and was selected from ROC curve analysis (see Additional file 4).
Sensitivity and specificity of candidate biomarkers
The sensitivities and specificities of all four biomarkers were calculated using these five cut-offs, as shown in Figure 3. KOC expression appears to show reasonably high sensitivity and specificity for all cut-offs except for the cut-off based on +2/+3 staining, which resulted in low sensitivity of only 67%. The 20% positive cells cut-off achieves marginally better sensitivity (84%) and specificity (100%) values compared with other cut-offs for KOC (Figure 3A). S100P appears to have similar sensitivity and specificity values for all five cut-offs with the 20% cut-off again achieving better combination of specificity and sensitivity, with values of 83% sensitivity and 100% specificity (Figure 3B).Applying the five cuts-offs to the analysis of mesothelin expression resulted in significantly different sensitivity and specificity values, however, the best combination was again achieved using the 20% cut-off, with 88% sensitivity and 92% specificity (Figure 3C). Although the sensitivity of MUC1 as biomarker is high across all cut-offs, its specificity is unacceptably low for all cut-offs, with a range of 18%-63% compromising the diagnostic accuracy of MUC1 (Figure 3D).
Sensitivity and specificity analysis of biomarkers for the diagnosis of pancreatico-biliary adenocarcinoma compared to normal tissue , based on five cut - offs for positivity: 5 % positive cells of any staining intensity; 10% positive cells of any staining intensity; 20 % positive cells of any staining intensity ; 2 OR 3 intensity i.e. moderate or strong staining of cells ; and Histoscore 20. Analysis is presented for A) KOC, B) S100P, C) mesothelin and D) MUC1.
Sensitivity and specificity analysis using biomarker panels
We next wanted to assess the sensitivity and specificity achieved using panels of biomarkers. The 10% and 20% cut-offs were selected for this investigation, based on their diagnostic performance.
Analysis based on one positive biomarker in a panel
We first assessed the sensitivity and specificity achieved when one biomarker in a panel is positive, using four different panels (Table 3). These panels were: a panel comprising all four biomarkers; a panel of three biomarkers (KOC, S100P and mesothelin); and two panels of two biomarkers (KOC and mesothelin, KOC and S100P). As expected, a panel of all four biomarkers achieved very low specificity of 40% and 65% respectively for 10% and 20% cut-offs, due to the low specificity of MUC1 as a biomarker. A panel of KOC, S100P and mesothelin achieved sensitivity/specificity of 100%/88% for the 10% cut-off and 99%/94% for the 20% cut-off. A panel of KOC and mesothelin achieved sensitivity/specificity of 97%/87% and 96%/93% for the 10% cut-off and 20% cut-offs, respectively. Finally, a panel of KOC and S100P achieved sensitivity/specificity of 98%/96% for the 10% cut-off and 99%/99% for the 20% cut-off.These panels were compared by combined SROC curve, using both the 10% cut-off (Figure 4A) and 20% cut-offs (Figure 4B). The combined SROC curve shows that a panel of KOC and S100P is superior to the other panels for both 10% and 20% cut-offs.
* Combined Summary ROC curves for 10 % (A) and 20% (B) cut-offs if only one biomarker was required to be positive in a panel. Four panels of biomarkers were compared. Panel 1 - KOC, S100P, Mesothelin and MUC1; Panel 2 - KOC, S100P, Mesothelin; Panel 3 - KOC, S100P; Panel 4 - KOC, Mesothelin. *Summary ROC curves plot sensitivity against specificity and draw a summary line depicting combined sensitivity and specificity of a panel. Combined Summary ROC curves compare different panels to show the most “accurate” panel. The summary line at the top left corner shows the biomarker which is most accurate compared to others lying lower and further to the right. This enables the most accurate panel to be identified.
Analysis based on two or more positive biomarkers in a panel
Finally, one biomarker panel comprising KOC, S100P and mesothelin was tested for sensitivity and specificity when at least 2 biomarkers in the panel are positive. This panel achieved almost 100% sensitivity/specificity for both 10% and 20% cut-offs (Table 3). Taken together, our results show that this panel could be used to improve diagnosis of PBA in difficult to diagnose cases.
Discussion
Four potentially diagnostic biomarkers, KOC, S100P, mesothelin and MUC1, were investigated in a relatively large cohort of PB patients (n = 99). The expression levels of KOC, S100P and mesothelin were high in tumour tissue compared with normal tissue. The diagnostic accuracy (sensitivity and specificity) of KOC and S100P individually was greater than that of mesothelin and MUC1. A panel of KOC, S100P and mesothelin with at least 2 biomarkers positive achieved almost perfect diagnostic accuracy in the differentiation of carcinoma from normal tissue.
IHC biomarkers have previously been investigated in surgical and cytological cohorts but none is yet routinely used for improving the diagnosis of PBA [35–37, 41, 44–46]. There are six significant reasons delaying the clinical translation of diagnostic biomarkers in PBA and other cancers. These reasons and our approach to address them are outlined below.
Firstly, a plethora of research exists on diagnostic IHC biomarkers coming from the bench assessed in pilot studies. There are many excellent papers but fewer validation studies for biomarkers that have shown promising results. Clearly, validation is important for future clinical application. Therefore, we performed a meta-analysis on diagnostic IHC biomarkers for PDAC [38], to review, quantify and assess the performance of already existing biomarkers and to try and identify superior candidate biomarkers.
The biomarkers derived from the meta-analysis in PDAC were applied in our study to both PDAC and CCC samples. Separate meta-analysis was not performed for CCC, because there are relatively few published papers on biomarkers in CCC (approximately 20-fold fewer than for PDAC; PubMed search in June 2014, unpublished data). However, those papers which are available for CCC suggest that the biomarker expression profile is similar to PDAC. To our knowledge, all of the known positive biomarkers for PDAC (versus corresponding normal tissue), including MUC1, P53, CK17, mesothelin, fascin, MUC4, 14-3-3σ and prostate stem cell antigen, show similar IHC expression in CCC (versus corresponding normal tissue) [39–42].
For these reasons, we focused on PDAC for the identification of potential diagnostic biomarkers then tested the resulting candidates in TMAs containing tissue from both PDAC and CCC using IHC. From our meta-analysis, we selected KOC [36, 37, 44, 47], S100P [32, 35, 48], mesothelin [30, 49, 50] and MUC1 [31, 40, 51] for investigation.
We found that expression of these biomarkers was similar in PDAC and CCC (Additional File 2): our results therefore supporting the previous literature [39–42].
Second, the sample size for studies investigating diagnostic biomarkers for PDAC is relatively small (median sample size, n = 48 from 57 articles). Moreover, matched normal tissue for most of the carcinoma case is not always available, leading to even smaller sample sizes for calculating biomarker specificity. Therefore, statistical power is relatively low and subsequently potentially useful biomarkers may be ignored. Our relatively larger sample size of 99 PBA cases (n = 99 adenocarcinomas and n = 99 matched normal tissue for each case; total n = 198) provided a solid platform for investigating these diagnostic IHC biomarkers.
Third, the lack of a standardised scoring system and absence of a uniform cut-off (threshold) for the interpretation of IHC remains problematic. Thus, researchers use a variety of traditional and novel scoring systems and diverse cut-offs, making the adoption of scoring systems and cut-offs potentially challenging for the pathologists [30, 35, 37, 41, 46, 49, 52–54]. We systematically chose cut-offs from ROC curve analysis to fully explore the diagnostic potential of all four biomarkers. These cut-offs provide an opportunity for the pathologists to select the best threshold that is more clinically applicable and has the potential to be routinely used in pathology. Three of these cut-offs are based on proportion of positive cells (5%, 10% and 20%) with staining of any intensity. The fourth cut-off is based on any proportion of cells exhibiting moderate and strong staining intensity, and the fifth cut-off is based on a Histoscore of 20. Notably, the 20% cut-off and Histoscore 20 provide reasonable sensitivity and specificity values for PBA diagnosis. A higher Histoscore value could potentially lead to more false negatives in tumour cases, therefore, a low cut-off value of 20 was chosen. Clearly, this cut-off will remove the probability of false negative and should increase the diagnostic confidence of pathologists for higher Histoscore values. For example, a Histoscore value of 200 for a biomarker in a suspicious case might help the pathologist to diagnose a tumour with confidence and with a much higher specificity.
Fourth, most of the IHC diagnostic biomarkers have been investigated individually [32, 46, 47, 55, 56], with few studies reporting the utility of biomarker panels [30, 36]. We carefully selected candidate biomarkers reported in different studies (KOC, mesothelin, S100P and MUC1) for investigation in a single experimental setting. Investigation of these biomarkers in a single cohort gave us the opportunity to compare biomarkers, and then further explore their diagnostic accuracy in a panel. Expectation from an ideal diagnostic biomarker is its ability to identify the diseased population (sensitivity) and exclude the normal population (specificity) in 100% cases. However, no single biomarker is 100% perfect; therefore these biomarkers were investigated in various combinations, to select an optimum panel for potential clinical application. For example, the individual sensitivity/specificity of KOC and S100P at a cut-off of 20% positive cells was 84%/100% and 83%/100% respectively. However, using a panel of KOC and S100P improved sensitivity to 99% without compromising the specificity (99%).
Furthermore, using a panel of KOC, S100P and mesothelin with at least 2 positive biomarkers achieved almost 100% sensitivity and specificity for both 10% and 20% cut-offs. This approach would assign a patient into the tumour positive category if 2 or more biomarkers are positive, possibly giving more assurance to the pathologist before assigning patient into positive category. Moreover, a combination of KOC, S100P and mesothelin antibodies should stain all major cellular compartments (cell membrane, nucleus and cytoplasm). Clinically, a cytology sample comprises a mixed population of cells and this panel will stain malignant cells more intensely making the interpretation of IHC convenient for the pathologist. The possible additional advantage of KOC is that it is not expressed in the contaminating gastrointestinal epithelial cells that are usually present in cytological samples [44, 57]. Our data also confirm the lack of expression of KOC in normal duodenum. Taken together, our results reinforce the reported sensitivity/specificity values for KOC, S100P and mesothelin [30, 35, 37, 57] and further explores their utility as a panel.
The fifth reason is that different research groups use different IHC experimental conditions, primary antibodies, clones, dilutions and manual/automated platforms that could potentially lead to a diverse range of sensitivity and specificity values for biomarkers [30, 45, 54, 58–60]. We thoroughly searched the literature for IHC parameters for KOC, S100P, mesothelin and MUC1. Those IHC parameters that achieved superior diagnostic accuracy were selected and further optimised in our histology laboratory before staining our cohort.
Finally, an important requirement for biomarker translation to the clinic is independent validation with the aim of improving already existing diagnosis. Purposeful validation in surgical and cytological tissue from PBA cohorts and subsequent prospective clinical study on cytological samples is deficient. Therefore, as an important step for potential clinical translation we investigated KOC, S100P, mesothelin and MUC1 in a surgical cohort of PBA patients with promising results for KOC, S100P and mesothelin as a biomarker panel.
The next step forward is to possibly investigate these biomarkers in a retrospective and then in a prospective cohort of cytology samples. This manuscript systematically attempted to answer all six major reasons hindering the clinical translation of diagnostic IHC biomarkers for pancreatic cancer. It also provides future direction and work packages to be performed before these diagnostic biomarkers can be used in day-to-day pathology practice.
Conclusions
Our results demonstrate that a biomarker panel of KOC, S100P and mesothelin is capable of categorising PB malignancy with high diagnostic accuracy in resection specimens. We plan to investigate this panel in archival cytological samples. As an adjunct to cytology, this panel has the potential to augment the categorisation for challenging diagnostic cases in routine clinical practice.To our knowledge, this is the first study of PB literature that identified cut-offs systematically for diagnostic purposes and used stringent panels to identify an optimum biomarker panel.
Abbreviations
- PDAC:
-
Pancreatic ductal adenocarcinoma
- PBA:
-
Pancreatico-biliary adenocarcinomas
- ERCP:
-
Endoscopic retrograde cholangio-pancreato-graphy
- EUS-FNA:
-
Endoscopic ultrasound-guided fine needle aspiration
- IHC:
-
immunohistochemistry
- ROC curve:
-
receiver operating characteristic curve
- TMA:
-
tissue microarrays
- SROC:
-
summary receiver operating characteristic.
References
Cancer Research UK. London: News and Resources [cited. 2012, Available from: http://info.cancerresearchuk.org/cancerstats/keyfacts/pancreatic-cancer/, April24]. Pancreatic cancer statistics- Key facts
Hidalgo M: Pancreatic cancer. N Engl J Med. 2010, 362 (17): 1605-1617.
Ferrone CR, Pieretti-Vanmarcke R, Bloom JP, Zheng H, Szymonifka J, Wargo JA, Thayer SP, Lauwers GY, Deshpande V, Mino-Kenudson M, Fernández-del Castillo C, Lillemoe KD, Warshaw AL: Pancreatic ductal adenocarcinoma: long-term survival does not equal cure. Surgery. 2012, 152 (3 Suppl 1): S43-S49.
Richter A, Niedergethmann M, Sturm JW, Lorenz D, Post S, Trede M: Long-term results of partial pancreaticoduodenectomy for ductal adenocarcinoma of the pancreatic head: 25-year experience. World J Surg. 2003, 27 (3): 324-329.
Woo SM, Ryu JK, Lee SH, Yoo JW, Park JK, Kim YT, Jang JY, Kim SW, Kang GH, Yoon YB: Recurrence and prognostic factors of ampullary carcinoma after radical resection: comparison with distal extrahepatic cholangiocarcinoma. Ann Surg Oncol. 2007, 14 (11): 3195-3201.
Bond-Smith G, Banga N, Hammond TM, Imber CJ: Pancreatic adenocarcinoma. Br Med J. 2012, 344: e2476-
Dabizzi E, Assef MS, Raimondo M: Diagnostic management of pancreatic cancer. Cancer. 2011, 3 (1): 494-509.
Karmazanovsky G, Fedorov V, Kubyshkin V, Kotchatkov A: Pancreatic head cancer: accuracy of CT in determination of resectability. Abdom Imaging. 2005, 30 (4): 488-500.
Miura F, Takada T, Amano H, Yoshida M, Furui S, Takeshita K: Diagnosis of pancreatic cancer. HPB. 2006, 8 (5): 337-342.
Van Beers BE: Diagnosis of cholangiocarcinoma. HPB. 2008, 10 (2): 87-93.
Adler D, Max Schmidt C, Al-Haddad M, Barthel JS, Ljung BM, Merchant NB, Romagnuolo J, Shaaban AM, Simeone D, Bishop Pitman M, Field A, Layfield LJ: Clinical evaluation, imaging studies, indications for cytologic study, and preprocedural requirements for duct brushing studies and pancreatic FNA: the Papanicolaou Society of Cytopathology recommendations for pancreatic and biliary cytology. Diagn Cytopathol. 2014, 42 (4): 325-332.
Chang KJ: State of the art lecture: endoscopic ultrasound (EUS) and FNA in pancreatico-biliary tumors. Endoscopy. 2006, 38 (Suppl 1): S56-S60.
Iqbal S, Friedel D, Gupta M, Ogden L, Stavropoulos SN: Endoscopic-ultrasound-guided fine-needle aspiration and the role of the cytopathologist in solid pancreatic lesion diagnosis. Pathol Res Int. 2012, 2012: 317167-
Kudo T, Kawakami H, Kuwatani M, Eto K, Kawahata S, Abe Y, Onodera M, Ehira N, Yamato H, Haba S, Kawakubo K, Sakamoto N: Influence of the safety and diagnostic accuracy of preoperative endoscopic ultrasound-guided fine-needle aspiration for resectable pancreatic cancer on clinical performance. World J Gastroenterol. 2014, 20 (13): 3620-3627.
Raut CP, Grau AM, Staerkel GA, Kaw M, Tamm EP, Wolff RA, Vauthey JN, Lee JE, Pisters PW, Evans DB: Diagnostic accuracy of endoscopic ultrasound-guided fine-needle aspiration in patients with presumed pancreatic cancer. J Gastrointest Surg. 2003, 7 (1): 118-126. discussion 127–118
Stewart CJ, Mills PR, Carter R, O'Donohue J, Fullarton G, Imrie CW, Murray WR: Brush cytology in the assessment of pancreatico-biliary strictures: a review of 406 cases. J Clin Pathol. 2001, 54 (6): 449-455.
Wakatsuki T, Irisawa A, Bhutani MS, Hikichi T, Shibukawa G, Takagi T, Yamamoto G, Takahashi Y, Yamada Y, Watanabe K, Obara K, Suzuki T, Sato Y: Comparative study of diagnostic value of cytologic sampling by endoscopic ultrasonography-guided fine-needle aspiration and that by endoscopic retrograde pancreatography for the management of pancreatic mass without biliary stricture. J Gastroenterol Hepatol. 2005, 20 (11): 1707-1711.
Yoshinaga S, Suzuki H, Oda I, Saito Y: Role of endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) for diagnosis of solid pancreatic masses. Dig Endosc. 2011, 23 (Suppl 1): 29-33.
Harewood GC, Wiersema LM, Halling AC, Keeney GL, Salamao DR, Wiersema MJ: Influence of EUS training and pathology interpretation on accuracy of EUS-guided fine needle aspiration of pancreatic masses. Gastrointest Endosc. 2002, 55 (6): 669-673.
Agarwal B, Abu-Hamda E, Molke KL, Correa AM, Ho L: Endoscopic ultrasound-guided fine needle aspiration and multidetector spiral CT in the diagnosis of pancreatic cancer. Am J Gastroenterol. 2004, 99 (5): 844-850.
Eloubeidi MA, Chen VK, Eltoum IA, Jhala D, Chhieng DC, Jhala N, Vickers SM, Wilcox CM: Endoscopic ultrasound-guided fine needle aspiration biopsy of patients with suspected pancreatic cancer: diagnostic accuracy and acute and 30-day complications. Am J Gastroenterol. 2003, 98 (12): 2663-2668.
Horwhat JD, Paulson EK, McGrath K, Branch MS, Baillie J, Tyler D, Pappas T, Enns R, Robuck G, Stiffler H, Jowell P: A randomized comparison of EUS-guided FNA versus CT or US-guided FNA for the evaluation of pancreatic mass lesions. Gastrointest Endosc. 2006, 63 (7): 966-975.
Hwang CY, Lee SS, Song TJ, Moon SH, Lee D, Park do H, Seo DW, Lee SK, Kim MH: Endoscopic ultrasound guided fine needle aspiration biopsy in diagnosis of pancreatic and peripancreatic lesions: a single center experience in Korea. Gut Liver. 2009, 3 (2): 116-121.
Touchefeu Y, Le Rhun M, Coron E, Alamdari A, Heymann MF, Mosnier JF, Matysiak T, Galmiche JP: Endoscopic ultrasound-guided fine-needle aspiration for the diagnosis of solid pancreatic masses: the impact on patient-management strategy. Aliment Pharmacol Ther. 2009, 30 (10): 1070-1077.
Varadarajulu S, Tamhane A, Eloubeidi MA: Yield of EUS-guided FNA of pancreatic masses in the presence or the absence of chronic pancreatitis. Gastrointest Endosc. 2005, 62 (5): 728-736. quiz 751, 753
Bellizzi AM, Stelow EB: Pancreatic cytopathology: a practical approach and review. Arch Pathol Lab Med. 2009, 133 (3): 388-404.
Logrono R, Kurtycz DF, Molina CP, Trivedi VA, Wong JY, Block KP: Analysis of false-negative diagnoses on endoscopic brush cytology of biliary and pancreatic duct strictures: the experience at 2 university hospitals. Arch Pathol Lab Med. 2000, 124 (3): 387-392.
Krishna NB, Mehra M, Reddy AV, Agarwal B: EUS/EUS-FNA for suspected pancreatic cancer: influence of chronic pancreatitis and clinical presentation with or without obstructive jaundice on performance characteristics. Gastrointest Endosc. 2009, 70 (1): 70-79.
Taylor CR: Standardization in immunohistochemistry: the role of antigen retrieval in molecular morphology. Biotech Histochem. 2006, 81 (1): 3-12.
Agarwal B, Ludwig OJ, Collins BT, Cortese C: Immunostaining as an adjunct to cytology for diagnosis of pancreatic adenocarcinoma. Clin Gastroenterol Hepatol. 2008, 6 (12): 1425-1431.
Chhieng DC, Benson E, Eltoum I, Eloubeidi MA, Jhala N, Jhala D, Siegal GP, Grizzle WE, Manne U: MUC1 and MUC2 expression in pancreatic ductal carcinoma obtained by fine-needle aspiration. Cancer. 2003, 99 (6): 365-371.
Deng H, Shi J, Wilkerson M, Meschter S, Dupree W, Lin F: Usefulness of S100P in diagnosis of adenocarcinoma of pancreas on fine-needle aspiration biopsy specimens. Am J Clin Pathol. 2008, 129 (1): 81-88.
Giorgadze TA, Peterman H, Baloch ZW, Furth EE, Pasha T, Shiina N, Zhang PJ, Gupta PK: Diagnostic utility of mucin profile in fine-needle aspiration specimens of the pancreas: an immunohistochemical study with surgical pathology correlation. Cancer. 2006, 108 (3): 186-197.
Jhala N, Jhala D, Vickers SM, Eltoum I, Batra SK, Manne U, Eloubeidi M, Jones JJ, Grizzle WE: Biomarkers in Diagnosis of pancreatic carcinoma in fine-needle aspirates. Am J Clin Pathol. 2006, 126 (4): 572-579.
Kosarac O, Takei H, Zhai QJ, Schwartz MR, Mody DR: S100P and XIAP expression in pancreatic ductal adenocarcinoma: potential novel biomarkers as a diagnostic adjunct to fine needle aspiration cytology. Acta Cytol. 2011, 55 (2): 142-148.
Ligato S, Zhao H, Mandich D, Cartun RW: KOC (K homology domain containing protein overexpressed in cancer) and S100A4-protein immunoreactivity improves the diagnostic sensitivity of biliary brushing cytology for diagnosing pancreaticobiliary malignancies. Diagn Cytopathol. 2008, 36 (8): 561-567.
Toll AD, Witkiewicz AK, Bibbo M: Expression of K homology domain containing protein (KOC) in pancreatic cytology with corresponding histology. Acta Cytol. 2009, 53 (2): 123-129.
Ali A, Ul-Haq Z, Mohamed M, MacKay DF, Duthie F, Oien K: Abstract 1142: systematic review and meta-analysis of immunohistochemical diagnostic markers for pancreatic ductal adenocarcinoma. Cancer Res. 2013, 73 (8 Supplement): 1142-
Argani P, Shaukat A, Kaushal M, Wilentz RE, Su GH, Sohn TA, Yeo CJ, Cameron JL, Kern SE, Hruban RH: Differing rates of loss of DPC4 expression and of p53 overexpression among carcinomas of the proximal and distal bile ducts. Cancer. 2001, 91 (7): 1332-1341.
Chu PG, Schwarz RE, Lau SK, Yen Y, Weiss LM: Immunohistochemical staining in the diagnosis of pancreatobiliary and ampulla of Vater adenocarcinoma: application of CDX2, CK17, MUC1, and MUC2. Am J Surg Pathol. 2005, 29 (3): 359-367.
Hassan R, Laszik ZG, Lerner M, Raffeld M, Postier R, Brackett D: Mesothelin is overexpressed in pancreaticobiliary adenocarcinomas but not in normal pancreas and chronic pancreatitis. Am J Clin Pathol. 2005, 124 (6): 838-845.
Swierczynski SL, Maitra A, Abraham SC, Iacobuzio-Donahue CA, Ashfaq R, Cameron JL, Schulick RD, Yeo CJ, Rahman A, Hinkle DA, Hruban RH, Argani P: Analysis of novel tumor markers in pancreatic and biliary carcinomas using tissue microarrays. Hum Pathol. 2004, 35 (3): 357-366.
Denley SM, Jamieson NB, McCall P, Oien KA, Morton JP, Carter CR, Edwards J, McKay CJ: Activation of the IL-6R/Jak/stat pathway is associated with a poor outcome in resected pancreatic ductal adenocarcinoma. J Gastrointest Surg. 2013, 17 (5): 887-898.
Yantiss RK, Cosar E, Fischer AH: Use of IMP3 in identification of carcinoma in fine needle aspiration biopsies of pancreas. Acta Cytol. 2008, 52 (2): 133-138.
Lim YJ, Lee JK, Jang WY, Song SY, Lee KT, Paik SW, Rhee JC: Prognostic significance of maspin in pancreatic ductal adenocarcinoma. Kor J Intern Med. 2004, 19 (1): 15-18.
Maass N, Hojo T, Ueding M, Luttges J, Kloppel G, Jonat W, Nagasaki K: Expression of the tumor suppressor gene Maspin in human pancreatic cancers. Clin Cancer Res. 2001, 7 (4): 812-817.
Yantiss RK, Woda BA, Fanger GR, Kalos M, Whalen GF, Tada H, Andersen DK, Rock KL, Dresser K: KOC (K homology domain containing protein overexpressed in cancer): a novel molecular marker that distinguishes between benign and malignant lesions of the pancreas. Am J Surg Pathol. 2005, 29 (2): 188-195.
Lin F, Shi J, Liu H, Hull ME, Dupree W, Prichard JW, Brown RE, Zhang J, Wang HL, Schuerch C: Diagnostic utility of S100P and von Hippel-Lindau gene product (pVHL) in pancreatic adenocarcinoma - With implication of their roles in early tumorigenesis. Am J Surg Pathol. 2008, 32 (1): 78-91.
Argani P, Iacobuzio-Donahue C, Ryu B, Rosty C, Goggins M, Wilentz RE, Murugesan SR, Leach SD, Jaffee E, Yeo CJ, Cameron JL, Kern SE, Hruban RH: Mesothelin is overexpressed in the vast majority of ductal adenocarcinomas of the pancreas: Identification of a new pancreatic cancer marker by serial analysis of gene expression (SAGE). Clin Cancer Res. 2001, 7 (12): 3862-3868.
McCarthy DM, Maitra A, Argani P, Rader AE, Faigel DO, Van Heek NT, Hruban RH, Wilentz RE: Novel markers of pancreatic adenocarcinoma in fine-needle aspiration: mesothelin and prostate stem cell antigen labeling increases accuracy in cytologically borderline cases. Appl Immunohistochem Mol Morphol. 2003, 11 (3): 238-243.
Wang Y, Gao J, Li Z, Jin Z, Gong Y, Man X: Diagnostic value of mucins (MUC1, MUC2 and MUC5AC) expression profile in endoscopic ultrasound-guided fine-needle aspiration specimens of the pancreas. Int J Cancer. 2007, 121 (12): 2716-2722.
Awadallah NS, Shroyer KR, Langer DA, Torkko KC, Chen YK, Bentz JS, Papkoff J, Liu W, Nash SR, Shah RJ: Detection of B7-H4 and p53 in pancreatic cancer: potential role as a cytological diagnostic adjunct. Pancreas. 2008, 36 (2): 200-206.
Boltze C, Schneider-Stock R, Aust G, Mawrin C, Dralle H, Roessner A, Hoang-Vu C: CD97, CD95 and Fas-L clearly discriminate between chronic pancreatitis and pancreatic ductal adenocarcinoma in perioperative evaluation of cryocut sections. Pathol Int. 2002, 52 (2): 83-88.
Cao D, Zhang Q, Wu LSF, Salaria SN, Winter JW, Hruban RH, Goggins MS, Abbruzzese JL, Maitra A, Ho L: Prognostic significance of maspin in pancreatic ductal adenocarcinoma: tissue microarray analysis of 223 surgically resected cases. Mod Pathol. 2007, 20 (5): 570-578.
Baruch AC, Wang H, Staerkel GA, Evans DB, Hwang RF, Krishnamurthy S: Immunocytochemical study of the expression of mesothelin in fine-needle aspiration biopsy specimens of pancreatic adenocarcinoma. Diagn Cytopathol. 2007, 35 (3): 143-147.
Swartz MJ, Batra SK, Varshney GC, Hollingsworth MA, Yeo CJ, Cameron JL, Wilentz RE, Hruban RH, Argani P: MUC4 expression increases progressively in pancreatic intraepithelial neoplasia. Am J Clin Pathol. 2002, 117 (5): 791-796.
Zhao H, Mandich D, Cartun RW, Ligato S: Expression of K homology domain containing protein overexpressed in cancer in pancreatic FNA for diagnosing adenocarcinoma of pancreas. Diagn Cytopathol. 2007, 35 (11): 700-704.
Argani P, Rosty C, Reiter RE, Wilentz RE, Murugesan SR, Leach SD, Ryu B, Skinner HG, Goggins M, Jaffee EM, Yeo CJ, Cameron JL, Kern SE, Hruban RH: Discovery of new markers of cancer through serial analysis of gene expression: prostate stem cell antigen is overexpressed in pancreatic adenocarcinoma. Cancer Res. 2001, 61 (11): 4320-4324.
Bhardwaj A, Marsh WL, Nash JW, Barbacioru CC, Jones S, Frankel WL: Double immunohistochemical staining with MUC4/p53 is useful in the distinction of pancreatic adenocarcinoma from chronic pancreatitis: a tissue microarray-based study. Arch Pathol Lab Med. 2007, 131 (4): 556-562.
Ordonez NG: Application of mesothelin immunostaining in tumor diagnosis. Am J Surg Pathol. 2003, 27 (11): 1418-1428.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1472-6890/14/35/prepub
Acknowledgements
We thank Clare Orange and Roderick Ferrier for their technical assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
KAO, AA, FRD and VB participated in the conception and study design. AA, VB, SD carried out data collection. AA, VB and CN carried out immunostaining. AA, NBJ, JPM, JSG and KAO contributed in data analysis and interpretation. NBJ, JPM, OJS, CRC, CJM, FRD, JSG, AA, KAO were involved in manuscript preparation and provided their critical comments from surgical, pathological and scientific perspectives. All authors have read and approved the final manuscript.
Electronic supplementary material
12907_2014_180_MOESM1_ESM.pdf
Additional file 1:Summary statistics of KOC, S100P, mesothelin and MUC1 expression on a per core basis comparing pancreatico-biliary adenocarcinomas with normal ducts and normal ducts & acini together.(PDF 47 KB)
12907_2014_180_MOESM2_ESM.pdf
Additional file 2:Summary statistics of KOC, S100P, mesothelin and MUC1 expression on a per core basis comparing pancreatic ductal adenocarcinoma with cholangiocarcinoma.(PDF 42 KB)
12907_2014_180_MOESM3_ESM.pdf
Additional file 3:Cut-offs resulting from ROC curve analysis based on the percentage of positive cells of any staining intensity (weak, moderate or strong) in tumour and normal cases for four biomarkers KOC, S100P, mesothelin and MUC1.(PDF 35 KB)
12907_2014_180_MOESM4_ESM.pdf
Additional file 4:ROC curves based on histoscores, in tumour and normal cases, for four biomarkers A) KOC, B) S100P, C) mesothelin and D) MUC1.(PDF 497 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Ali, A., Brown, V., Denley, S. et al. Expression of KOC, S100P, mesothelin and MUC1 in pancreatico-biliary adenocarcinomas: development and utility of a potential diagnostic immunohistochemistry panel. BMC Clin Pathol 14, 35 (2014). https://doi.org/10.1186/1472-6890-14-35
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1472-6890-14-35