Abstract
Background
A standard contrast enema for Hirschsprung's disease can sometimes be inconclusive in delineating a transition zone especially in neonates and infants. The aim of this study was to determine the utility and diagnostic accuracy of a plain abdominal radiograph transition zone (PARTZ) in predicting the level of aganglionosis.
Methods
A prospective observational study of neonates and infants with biopsy proven Hirschsprung's disease was carried out from March 2004 through March 2006. All patients underwent a plain abdominal radiograph and a contrast enema followed by a rectal biopsy. The transition zone on a plain radiograph (PARTZ) and contrast enema (CETZ) were compared with operative and pathology reports. Results were analyzed by chi square test and expressed as their p values and 95% confidence intervals.
Results
PARTZ and CETZ suggestive of Hirschsprung's disease was seen in 24(89%) and 18(67%) patients respectively. The PARTZ and CETZ matched with the pathologic level of transition zone in 22(92%) and 13(72%) patients, p = 0.001, 95% CI (-1.87 to -0.79). In the 9 (33%) patients in whom contrast enema failed to reveal a transition zone, PARTZ was seen in 6/9(66%) patients and correlated with the pathological level of aganglionosis in 4/6(67%) patients, p = 0.001 95% CI (-1.87 to -0.79). The overall accuracy of PARTZ and CETZ was 96% and 84% respectively, p = 0.008, 95% CI (-6.09 to -3.6).
Conclusion
A plain abdominal radiographic transition zone is reliable in predicting the level of transition zone in cases of inconclusive contrast enema. It may be particularly helpful developing countries where laparoscopic techniques are not available to accurately identify the transition zone.
Similar content being viewed by others
Background
Hirschsprung's Disease (HD) is a common cause of pediatric intestinal obstruction [1]. A funnel shaped transition zone on a contrast enema (CETZ) at the junction of aganglionic and ganglionic gut is considered a hallmark for its diagnosis [2, 3]. In recent years, primary pull-through procedures, especially the transanal pull through, has become popular for the treatment of rectosigmoid Hirschsprung's disease [4, 5]. Knowledge of the extent of aganglionic bowel on contrast enema is important for preoperative planning of trans-anal surgery [6]. Although CETZ remains a reliable diagnostic sign, some investigators have found its accuracy to range between 80% to 94%, with a 20% false negative result in neonates and infants [7, 8]. The usefulness and accuracy of a transition zone visible on a plain abdominal radiograph (PARTZ) has not yet been evaluated. We therefore conducted a prospective study to investigate whether PARTZ could reliably predict the level of transition zone.
Methods
From March 2004 to February 2006, neonates and infants with clinical suspicion of Hirschsprung's disease were enrolled in this prospective observational study that was approved by the Ethics committee of B.P Koirala Institute of Health Sciences, Nepal.
Patients inclusion criteria
1) Delayed passage of meconium (beyond 48 hours for a full term neonate and beyond 72 hours for a preterm neonate).
2) Patients with defecation problems since birth and abdominal distension.
Patients exclusion criterion
1) The modified Bell staging criteria [9] in which a composite of clinical signs and symptoms (eg, abdominal distention, bloody stools, or hypotension), biochemical parameters (eg, thrombocytopenia or neutropenia), and radiographic signs (eg, pneumatosis or pneumoperitoneum) was used to grade the severity of NEC.
2. Abdominal radiograph showing multiple air fluid levels.
Written and verbal informed consent was taken from the patients who satisfied the inclusion criteria to undergo further investigations. Data on gestational age and first passage of meconium after birth were collected. Prior to per rectal examination, all patients underwent a plain abdominal radiograph and a contrast enema.
Plain abdominal radiograph transition zone
A plain abdominal erect radiograph was taken to visualize tapering and abrupt cutoff of left colon gas shadow above the pelvis, which indicated the level of PARTZ. All plain abdominal radiographs were read by the same radiologist (A.T).
Contrast enema
Pediatric radiologists performed the contrast enema in a routine manner using standard CE techniques. Dilute barium sulfate was administered rectally using a # 6 infant feeding tube placed just within the rectum. No balloon catheters were used. All CE images were read by the same pediatric radiologist (A.T). The classical finding of a transition zone [2] (CETZ) was considered being a positive result.
Rectal biopsy
The final diagnosis of HD was made by the absence of ganglion cells in a full thickness biopsy (FTB). Biopsy specimens were obtained at 2 cm above the dental line, posteriorly. These specimens were examined for ganglion cells with a hematoxylin-eosin staining and acetylcholinesterase activity was determined as previously described by Karnovsky and Roots [10]. A biopsy was considered to be positive when the acetylcholinesterase activity was elevated in combination with an absence of ganglion cells. An experienced histopathologist with specific interest and expertise evaluated the biopsies for HD (A.S).
The decision to perform a single stage transanal pull through was determined by the patient's general condition, and the presence of a rectosigmoid or midsigmoid transition zone on a plain abdominal radiograph or CE. Transanal pull through was performed using the operative technique described previously [4]. Following the surgery, the location of PARTZ and CETZ was compared with pathology reports documenting the level of aganglionosis. For the purpose of this comparison, the bowel was divided into 9 segments: rectosigmoid, midsigmoid colon, descending colon, splenic flexure, transverse colon, hepatic flexure, ascending colon, and cecum/small bowel (total colon). The PARTZ and CETZ were determined to be concordant if located in the same/adjoining bowel segment as the pathologic level of aganglionosis or discordant if they were separated from the level of aganglionosis by at least one intervening bowel segment.
Statistical analysis
We tested for the concordance between the radiographic transition zone (PARTZ and CETZ) and the pathologic extent of aganglionic bowel using chi square test with a 95% confidence interval. In all analyses, P values <0.05 were considered to be statistically significant. Statistical analyses were performed using the SPSS software (version 12.01, Chicago, IL, USA).
Results
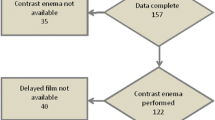
Twenty seven patients (20 neonates and 7 infants) were included in the study, Table 1. A total of 24 transanal pull through procedures were performed. Data of the results of the tests and their concordance with pathological level of aganglionosis are shown in Table 2.
Correlation of plain abdominal radiograph transition zone and its pathologic location
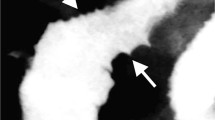
A plain abdominal radiograph showed tapering of left colon gas with an abrupt cutoff indicative of a transition zone (PARTZ) in 24/27 (89%) patients. The PARTZ was located at rectosigmoid in 21(88%), midsigmoid in 2(8%) and at descending colon in 1(4%), Fig 1A,1B,1C respectively. Of the 24 patients with a PARTZ, 22 (92%) had a matching level of aganglionosis [p = 0.00, 95% CI (-4.4 to -3.93)]
A: Plain abdominal radiograph showing a PARTZ at rectosigmoid, arrow. B: Plain abdominal radiograph showing a PARTZ at midsigmoid, arrow. C: Plain abdominal radiograph showing a PARTZ at descending colon, arrow. D: Contrast enema showing a CETZ at rectosigmoid, arrow. E: Contrast enema showing a CETZ at midsigmoid, arrow. F: Contrast enema showing a CETZ at descending colon, arrow.
Correlation of contrast enema transition zone and its pathologic location
A CETZ was seen in 18/27(67%) patients. The CETZ was located at rectosigmoid in 14(78%), midsigmoid in 2(11%) and descending colon in 2(11%), Fig 1D,1E,1F. Of the 18 patients with CETZ, 13 (72%) had a matching level of aganglionosis [p = 0.6, 95% CI (-0.85 to 0.52)].
Inconclusive contrast enema versus PARTZ
Contrast enema failed to reveal a transition zone in 9/27(33%) patients. A PARTZ was seen in 6/9(66%) of these patients. PARTZ correlated with the pathological level of aganglionosis in 4/6(67%) patients, p = 0.001 95% CI (-1.87 to -0.79).
Comparison of PARTZ with CETZ
The overall accuracy of PARTZ and CETZ concordant to the pathological level of aganglionosis was 92% and 72% respectively, p = 0.008, 95% CI (-6.09 to -3.6).
Discussions and Conclusion
The hallmark radiological feature of HD is the presence of a transition zone on a contrast enema (CETZ) [2]. One of the requisites for successful pullthrough surgery for Hirschsprung's disease is identification of the transition zone, for which a contrast enema is relied upon. Although CETZ remains the most accurate diagnostic sign for Hirschsprung's disease, it is not specific enough to delineate the transition zone in neonates and infants [7, 8, 11]. Other radiographic signs to improve the diagnostic yield, including delayed and abnormal contractions of distal aganglionic segment also appear to be of limited value [2, 12]. There has been a recent trend in the use of preoperative endoscopic marking of the transition zone, and laparoscopy-assisted suction colonic biopsy (SCBx) to provide accurate identification of the transition zone[13, 14]. However, these investigations are not available in most developing countries. A plain abdominal radiograph, which is routinely done to evaluate any intestinal obstruction including HD, may provide more information than just the diagnosis. Its utility to locate a plain abdominal radiograph transition zone (PARTZ), especially when CETZ is inconclusive, has not been previously studied. In this study, PARTZ was clearly seen in 89% of the patients, which accurately corresponded with the pathological level of aganglionosis in 92% of the patients undergoing a pull through procedure. A CETZ on the other hand was conclusive in only 67% of the patients. Importantly, for this subset of patients with inconclusive CETZ (9 patients), a PARTZ accurately correlated with the pathological level of aganglionosis in 4(67%) patients. A false negative or inconclusive CE may be attributable to technical factors, too much or forceful instillation of contrast, a small caliber of neonatal bowel, prior colonic washouts or a long segment disease[15, 14]. These factors may obliterate the transition zone. On the other hand, visualization of PARTZ relies on the physiological tapering of bowel gas in the transition zone above the distal collapsed gasless aganglionic segment, which is left undisturbed by avoiding instillation of any contrast in the rectum. Although in cases with inconclusive CE studies, retention of barium seen on radiographs obtained 24 hours after a barium enema is considered suggestive of Hirschsprung's disease [2], the level of transition zone remains uncertain unless laparoscopy is employed [14]. If facilities of laparoscopy are not available, an umbilical incision provides an excellent, safe, and versatile alternative to laparoscopy or other abdominal incisions [17]. In conclusion, our study underscores the importance of combining the information of a transition zone on a plain abdominal radiograph and contrast enema to decide the surgical approach for the correction of Hirschsprung's in developing countries where laparoscopic facilities are not available. The small incidence of discordance between anticipated level of aganglionosis and operative findings should be recognized, particularly when planning a one-stage transanal pull-through.
Abbreviations
- 1. HD:
-
Hirschsprung's disease
- 2. CE:
-
contrast enema
- 3. CETZ:
-
contrast enema transition zone
- 4. PARTZ:
-
Plain abdominal radiograph transition zone
- 5. FTRB:
-
Full thickness rectal biopsy
- 6. PLAG:
-
Pathological level of aganglionosis
References
Klein MD, Coran AG, Wesley JR, Drongowski RA: Hirschsprung's disease in the newborn. J Pediatr Surg. 1984, 19: 370-374. 10.1016/S0022-3468(84)80255-9.
Rosenfield NS, Ablow RC, Markowitz RI, DiPietro M, Seashore JH, Touloukian RJ, Cicchetti DV: Hirschsprung disease: accuracy of the barium enema examination. Radiology. 1984, 150: 393-400.
O'Donovan AN, Habra G, Somers S, Malone DE, Rees A, Winthrop AL: Diagnosis of Hirschsprung's disease. AJR Am J Roentgenol. 1996, 167: 517-520.
De la Torre-Mondragon L, Ortega-Salgado JA: Transanal endorectal pull-through for Hirschsprung's disease. J Pediatr Surg. 1998, 33: 1283-6. 10.1016/S0022-3468(98)90169-5.
Langer JC, Durrant AC, de la Torre L, Teitelbaum DH, Minkes RK, Caty MG, Wildhaber BE, Ortega SJ, Hirose S, Albanese CT: One-stage transanal Soave pullthrough for Hirschsprung disease: a multicenter experience with 141 children. Ann Surg. 2003, 238: 569-583.
Proctor ML, Traubici J, Langer JC, Gibbs DL, Ein SH, Daneman A, Kim PC: Correlation between radiographic transition zone and level of aganglionosis in Hirschsprung's disease: Implications for surgical approach. J Pediatr Surg. 2003, 38: 775-778. 10.1016/jpsu.2003.50165.
Taxman TL, Yulish BS, Rothstein FC: How useful is the barium enema in the diagnosis of infantile Hirschsprung's disease?. Am J Dis Child. 1986, 140: 881-884.
Jamieson DH, Dundas SE, Belushi SA, Cooper M, Blair GK: Does the transition zone reliably delineate aganglionic bowel in Hirschsprung's disease?. Pediatr Radiol. 2004, 34: 811-815. 10.1007/s00247-004-1292-7.
Walsh MC, Kliegman RM: Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am. 1986, 33: 179-201.
Karnovsky MJ, Roots LA: "Direct-coloring" thiocholine method for cholinesterases. J Histochem Cytochem. 1964, 12: 219-221.
Mozes YN, Rachmel A, Schonfeld T, Schwarz M, Steinberg R, Ashkenazi S: Difficulties in making the diagnosis of Hirschsprung's disease in early infancy. J Paediatr Child Health. 2004, 40: 716-10.1111/j.1440-1754.2004.00519.x.
Siegel MJ, Shackelford GD, McAlister WH: The rectosigmoid index. Radiology. 1981, 139: 497-499.
Kohno M, Ikawa H, Fukumoto H, Okamoto S, Masuyama H, Konuma K: Usefulness of endoscopic marking for determining the location of transanal endorectal pull-through in the treatment of Hirschsprung's disease. Pediatr Surg Int. 2005, 21: 873-877. 10.1007/s00383-005-1505-7.
Antao B, Roberts J: Laparoscopic-assisted transanal endorectal coloanal anastomosis for Hirschsprung's disease. J Laparoendosc Adv Surg Tech. 2005, 15: 75-9. 10.1089/lap.2005.15.75.
Blake NS: Diagnosis of Hirschsprung's disease and allied disorders. Hirschsprung's disease and allied disorders. New York: Harwood Academic Publishers, 223-290.
Das NL, Hingsbergen EA: Case 22: total colonic aganglionosis – long-segment Hirschsprung disease. Radiology. 2000, 215: 391-394.
Sauer CJ, Langer JC, Wales PW: The versatility of the umbilical incision in the management of Hirschsprung's disease. J Pediatr Surg. 2005, 40: 385-389. 10.1016/j.jpedsurg.2004.10.025.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2431/7/5/prepub
Acknowledgements
The authors and coauthors sincerely acknowledge the cooperation and help extended by the radiology and surgical staff during this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
AP and DKG have been involved in the design of the study, acquisition, analysis and interpretation of data. AT and AKS performed the radiological and pathological analysis.
SNS provided anesthesia support for surgery. NB, CSA and SA helped to perform statistical analysis, and revising the manuscript critically.
All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Pratap, A., Gupta, D.K., Tiwari, A. et al. Application of a plain abdominal radiograph transition zone (PARTZ) in Hirschsprung's disease. BMC Pediatr 7, 5 (2007). https://doi.org/10.1186/1471-2431-7-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2431-7-5