Abstract
The disease burden of respiratory syncytial virus (RSV) infection in the adult population has not been well characterized compared to children. Investigation of the clinical characteristics and disease burden of adult RSV infection would help to establish public health policy and a future vaccine strategy. We retrospectively collected medical records of hospitalized adult patients who were diagnosed with RSV infection from January 2012 to December 2015 from three tertiary hospitals. Baseline characteristics, clinical outcomes and economic charge during hospitalization were compared by age groups (19–49 years, 50–64 years, and ≥ 65 years) using Chi-square test. The odds of risk factors of RSV pneumonia were calculated using binary logistic regression. A total of 204 patients from three hospitals were enrolled. Patients who older than 65 years were 132 (64.7%). 118 (57.8%) patients had clinically confirmed pneumonia and 22 (10.8%) died in a hospital. The median medical cost of RSV pneumonia was 2,855.26 USD (interquartile range, 1,561.85–5,379.55) per each admission. Solid cancer (adjusted OR, 3.85; 95% CI, 1.65–9.02, p = 0.002) and hematologic malignancy (all patients had pneumonia) were shown to be risk factors for RSV pneumonia. RSV infection in South Korea seemed to have a significant burden among adults as pneumonia, care in the intensive care unit and mortality. Nationwide awareness and further effort to recognize the current burden, prepare specific treatment, and prevent adult RSV infection would be necessary.
Similar content being viewed by others
Introduction
Respiratory syncytial virus (RSV) belongs to the family of Paramyxoviridae and is the most important cause of lower respiratory tract infection in infants and young children. The virus causes common cold, bronchiolitis and pneumonia which are spread by close contact and large droplets. However, the clinical impact of RSV infection in adult populations had been underestimated until outbreaks in hospitals and healthcare facilities were identified. The infection may induce serious outcome especially in the elderly, patients with chronic cardiopulmonary disease and immunocompromised individuals1. Also, the disease burden of RSV is not negligible compared to influenza among adults at high risk or the elderly2,3. In the United States, annually 2–10% of community-dwelling older adults are infected and approximately 11,000 persons die due to the illness4. In South Korea, RSV was detected in 1.1% of all adult respiratory infections and shows similar seasonal occurrence during childhood5,6.
Recently, the Strategic Advisory Group of Experts of the World Health Organization presented an issue of RSV vaccine production in April 2016, and stated that the elderly, pregnant women and immunocompromised patients would be the target populations of the RSV vaccine. Therefore, a precise investigation of the epidemiology and disease burden of adult RSV infection is key to establishing an accurate vaccine strategy. Furthermore, the increasing elderly population with debilitated host immune response and underlying comorbidities is nowadays a public health problem in developed countries. Unfortunately, large-scale intensive research regarding adult RSV infection is lacking in South Korea. The aim of this study was to reveal the clinical manifestations, epidemiology and disease burden of adult RSV infections in South Korea, especially in elderly and at-risk groups. It may be useful to contemplate the eligible target population of RSV vaccination.
Methods
Study subjects and data collection
From January 2012 to December 2015, all adult patients over 19-years-old diagnosed to RSV infection were enrolled retrospectively from three tertiary hospitals: Korea University Guro Hospital, Korea University Ansan Hospital, and Hallym University Kangnam Sacred Heart Hospital. Each hospital has an emergency room, inpatient facility and intensive care unit (ICU) and is located in Seoul and its suburban area.
Participants included all hospitalized RSV-diagnosed patients. The diagnosis of RSV infection was confirmed by viral culture or respiratory viruses multiplex real-time polymerase chain reaction (PCR) kit using respiratory specimens. The viral culture method in the laboratory could not distinguish the serotype of RSV in contrast to real-time PCR kit. We retrospectively reviewed the medical charts of the patients using case report forms, and extracted data regarding epidemiology, duration of admission, ICU admission rate, symptoms, laboratory results, underlying diseases, complications, and clinical outcomes such as pneumonia and use of a mechanical ventilator. Pneumonia was defined as concomitant clinical symptoms, elevation of inflammatory markers and pneumonic infiltration on chest radiograph as confirmed by a radiologist7. The ages of the patients were categorized into young adult (19–49 years old), middle-aged adult (50–64 years old), and elderly (65 years old or more).
Medical cost was calculated as all direct healthcare costs including the charge for room and meals, the cost of medicines and expendables, and the cost of any medical procedures8,9. The duration of cost summation was from the date of performance of diagnostic test to the date when the patient was transferred to another hospital, discharged or died10. Each patient’s cost was extracted in Korean Won (KRW) and presented as U.S. dollars (USD) reflecting the exchange rate at the time (1 USD = 1,128.30 KRW, on 16th October 2018).
This study was approved by the Korea University Institutional Review Board (IRB No. 2019GR0127 in Guro hospital, IRB No. AS16203 in Ansan hospital) and the Kangnam Sacred Heart Hospital Institutional Review Board (IRB No. HKS2019-09-017). The study was performed in accordance with the ethical standards of the Declaration of Helsinki. Informed consent was waived because of the retrospective design of the study.
Statistical analysis
Each nonparametric variable in baseline characteristics and clinical outcomes was compared using the chi-square test with Fisher’s exact test. Continuous variable such as length of hospital stay was compared using the analysis of variance. The odds of risk factors of RSV pneumonia were calculated using binary logistic regression analysis. Any continuous independent variables were assumed to be a linear relationship with a dependent variable in the logistic regression analysis. A P value of < 0.05 was considered to indicate statistical significance. All statistical analyses were performed using SPSS Statistics version 20 for Windows (IBM Corp., Armonk, NY, USA).
Ethical approval
2019GR0127 approved by Korea University Institutional Review Board at April 11th, 2019.
Results
A total of 204 patients were enrolled from the three hospitals: 146 from Guro Hospital, 44 from Ansan Hospital, and 14 from Kangnam Sacred Heart Hospital. Most patients underwent diagnostic tests for RSV because of their newly developed respiratory symptoms and/or lung infiltrations on chest radiograph, except four patients. These four participants were in chronic bedridden states and were incidentally diagnosed with RSV infection during work-up for altered states of consciousness. The demographic characteristics of the patients are shown in Table 1. Sore throat and nasal congestion/rhinorrhea was more dominant in 19–49 years-old group (sore throat: 5 (25.0%); nasal congestion/rhinorrhea: 7 (35.0%)) than in 50–64 years-old group (sore throat: 4 (7.7%); nasal congestion/rhinorrhea: 14 (26.9%)) and ≥ 65 years-old group (sore throat: 6 (4.5%); nasal congestion/rhinorrhea: 21 (15.9%)). All proportions of underlying diseases were not significantly different between age groups. There was no human immunodeficiency virus infection in the study population.
The general admission rate and proportions of mechanical ventilation, pneumonia and mortality were not significantly different between age groups. There were 12 (60.0%) cases of RSV pneumonia were in the young adult group, 31 (59.6%) in the middle-aged adult group, and 75 (56.8%) in the elderly group. All patients with hematologic malignancies had RSV pneumonia. The rate of ICU admission was higher among the elderly (25.0%) than among young adults (10.0%) and middle-aged adults (11.5%), but also showed no significant difference (p = 0.060) (Table 1).
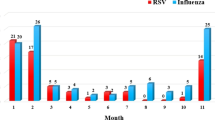
189 (92.6%) were diagnosed by multiplex real-time PCR and 15 (7.4%) were diagnosed by viral culture. The results of RSV serotype in 17 patients were undefined, including two missed data in PCR group. The dominant serotype of RSV changed annually and prevailed from winter to early spring. RSV serotype A was dominant in 2012–2013 and 2013–2014 winter seasons (Fig. 1). More than half of patients enrolled in the study were in the elderly group (65 years old or more, 64.7%) and the mean age ± standard deviation was 67.77 ± 13.94 (Fig. 2).
The median medical cost of RSV pneumonia per each admission seemed to be increasing by the age groups: 1,957.33 USD in the young adult group, 2,116.43 USD in the middle-aged group, and 2,933.17 USD in the elderly group. The differences in mean medical cost were not statistically significant between age groups and underlying diseases (data not shown). Admission rate, mortality and length of hospital stay also showed no statistical difference between age groups (Table 2).
To evaluate which risk factors contribute to the occurrence of pneumonia in RSV infection, odds ratios (ORs) were calculated for each age group, sex, symptoms, RSV serotype and underlying disease (Table 3). Age group, sex, RSV serotype and symptoms were not related to RSV pneumonia. Regarding underlying diseases, solid cancer (adjusted OR, 3.85; 95% CI, 1.65–9.02, p = 0.002) and hematologic malignancy (all patients had pneumonia) appeared to be significantly associated with RSV pneumonia.
Discussion
Our findings suggested that considerable mortality and economic burden of RSV infection in the adult population exist in South Korea. In addition, solid cancer and hematologic malignancy displayed significant relationships with RSV pneumonia.
Recently, the importance of RSV infection in the adult population is increasing globally. However, there have been insufficient studies about the clinical characteristics and disease burden of adult RSV infection. In contrast, studies of RSV infection in childhood are well known and actively conducted in various countries and groups. Hall et al. showed that 18% of children with acute respiratory infections under the age of 5 years had RSV infection. This high infection rate is a serious problem in pediatric public health because it leads to a substantial disease burden regardless of individual underlying illnesses11,12. On the other hand, RSV infection in adults seems to be associated with the elderly population and chronic diseases despite the lower rate than in childhood. In a study conducted in the U.S., RSV infection comprised 8.3% of acute respiratory illnesses among the elderly; this proportion was 4% in a French study13,14. In Korean studies, laboratory-confirmed RSV infection accounted for 2.8% of all respiratory viral infections and 12.7% of hospitalizations on account of respiratory viral infection15,16. However, the percentage of RSV among all respiratory illnesses including bacterial infection in Korean adults had not been reported.
The seasonal trend of RSV serotype predominance seemed to be alternated biannually, which was also shown in other countries17. This pattern might be explained by the acquisition of transient herd immunity of average duration 2 years18. It is controversial in children and infants that the serotype variability has an impact on clinical course and outcome of RSV infection19. However, none of studies in our knowledge presented precise difference of clinical manifestations between RSV serotype A and B in adults. In our study, the RSV serotype did not seem to be a risk factor of RSV pneumonia. Further clinical and physiologic research would be necessary to clarify the effect of RSV serotype to clinical outcomes.
Most RSV patients were over 65 years of age. Nonhospitalized RSV infected patients were excluded in our study, but they might impose a considerable burden on local clinics as influenza-like illnesses. Nevertheless, the high rates of ICU admission (25.0%), pneumonia (56.8%) and in-hospital mortality (10.6%) in the elderly population signify the severity of adult RSV infection. Lee et al. also reported that 71.9% of adults with RSV infection had lower respiratory complications, and 9.1% died within 30 days7. The rate of mortality in our study was elevated from 10.8 to 13.6% when the population was confined to that with pneumonia, which seems to be important in determining the prognosis of RSV infections.
The economic burden of adult RSV infection is not well known in contrast to that among children. In the U.S., RSV infection had similar burden and clinical outcomes to influenza infection in the adult population2. Han et al. calculated almost 20 years ago that the mean cost of RSV pneumonia during hospitalization was $11,00020. The relatively low cost in our study may be attributed to the discrepancy of medical charge and national insurance systems between the two countries. We set the median medical cost to amend the skewed distribution of individual medical costs. The median medical cost was similar between age groups which may reflect a high prevalence of underlying diseases in all groups. However, a larger and more intensive study of the economic burden of adult RSV infection would be necessary to clarify this pattern. The entire domestic cost of adult RSV infection would be much more increased because of easy diagnosis, aging of the population, and an increasing prevalence of concomitant chronic diseases.
The presence of underlying disease affected the poor outcome of RSV infection in previous studies, especially cancerous or immunocompromised status. Solid organ transplantation and hematopoietic stem cell transplantation were related to increased burden of RSV infection in many studies, and the outcomes worsened when the patients had lower respiratory diseases21,22. A study of South Korean adults also showed that chronic lung disease, bacterial co-infection and lower respiratory infection could be associated with increased mortality23. Our data revealed that solid cancer and hematologic malignancy were significantly related to the occurrence of RSV pneumonia; however, other underlying illnesses, RSV serotype, sex, and age were not related. This suggests that even young adults could suffer severe RSV infection and bear considerable disease burden.
The study has several limitations. First, we could not obtain the general incidence of RSV infection in the entire population due to the retrospective study design and the limited area of residence among the participants. In addition, the unbalanced sampling from each participating hospital might lead to selection bias because most of cases were collected from one hospital [Guro hospital: 146 (70.2%)]. Differences of baseline characteristics between three hospitals were shown in Supplementary Table 1. Second, RSV infections with mild symptoms would be overlooked by low rate of PCR performance, clinicians’ unawareness and lack of active antiviral agents24. This ignorance might underestimate the burden of RSV infection. Third, cases of some underlying diseases and other variables like liver disease and HIV infection were so few that related data might be unreliable. Nevertheless, our study would be helpful to recognize the magnitude of RSV infection in the hospital and to facilitate to make an appropriate countermeasure against adult RSV infection through vaccine development, novel antiviral agents and control of nosocomial transmission.
In conclusion, RSV infection in the adult population showed significant clinical and economic burden and largely related to lower respiratory tract complications and mortality. Solid cancer and hematologic malignancies contributed to the occurrence of RSV pneumonia. The substantial burden of adult RSV infection should be considered to establish public health policies and the target of the future RSV vaccine.
References
Falsey, A. R. & Walsh, E. E. Respiratory syncytial virus infection in adults. Clin. Microbiol. Rev. 13, 371–384 (2000).
Falsey, A. R., Hennessey, P. A., Formica, M. A., Cox, C. & Walsh, E. E. Respiratory syncytial virus infection in elderly and high-risk adults. N. Engl. J. Med. 352, 1749–1759. https://doi.org/10.1056/NEJMoa043951 (2005).
Widmer, K. et al. Rates of hospitalizations for respiratory syncytial virus, human metapneumovirus, and influenza virus in older adults. J. Infect. Dis. 206, 56–62. https://doi.org/10.1093/infdis/jis309 (2012).
Branche, A. R. & Falsey, A. R. Respiratory syncytial virus infection in older adults: an under-recognized problem. Drugs Aging 32, 261–269. https://doi.org/10.1007/s40266-015-0258-9 (2015).
Seo, Y. B. et al. Epidemiologic differences of four major respiratory viruses between children, adolescents, and adults in Korea. J. Infect. Chemother. 20, 672–677. https://doi.org/10.1016/j.jiac.2013.07.009 (2014).
Seo, Y. B. et al. Etiology and clinical outcomes of acute respiratory virus infection in hospitalized adults. Infect. Chemother. 46, 67–76. https://doi.org/10.3947/ic.2014.46.2.67 (2014).
Lee, N. et al. High morbidity and mortality in adults hospitalized for respiratory syncytial virus infections. Clin. Infect. Dis. 57, 1069–1077. https://doi.org/10.1093/cid/cit471 (2013).
Choi, W. S. et al. Disease burden of herpes zoster in Korea. J. Clin. Virol. 47, 325–329. https://doi.org/10.1016/j.jcv.2010.01.003 (2010).
Suh, M. et al. Socioeconomic burden of influenza in the Republic of Korea, 2007–2010. PLoS ONE 8, e84121. https://doi.org/10.1371/journal.pone.0084121 (2013).
Emukule, G. O. et al. The burden of influenza and RSV among inpatients and outpatients in rural western Kenya, 2009–2012. PLoS ONE 9, e105543. https://doi.org/10.1371/journal.pone.0105543 (2014).
Hall, C. B. et al. The burden of respiratory syncytial virus infection in young children. N. Engl. J. Med. 360, 588–598. https://doi.org/10.1056/NEJMoa0804877 (2009).
Heikkinen, T., Ojala, E. & Waris, M. Clinical and socioeconomic burden of respiratory syncytial virus infection in children. J. Infect. Dis. 215, 17–23. https://doi.org/10.1093/infdis/jiw475 (2017).
Sundaram, M. E., Meece, J. K., Sifakis, F., Gasser, R. A. Jr. & Belongia, E. A. Medically attended respiratory syncytial virus infections in adults aged >/= 50 years: clinical characteristics and outcomes. Clin. Infect. Dis. 58, 342–349. https://doi.org/10.1093/cid/cit767 (2014).
Loubet, P. et al. Clinical characteristics and outcome of respiratory syncytial virus infection among adults hospitalized with influenza-like illness in France. Clin. Microbiol. Infect. 23, 253–259. https://doi.org/10.1016/j.cmi.2016.11.014 (2017).
Noh, J. Y. et al. Laboratory surveillance of influenza-like illness in seven teaching hospitals, South Korea: 2011–2012 season. PLoS ONE 8, e64295. https://doi.org/10.1371/journal.pone.0064295 (2013).
Choi, H. S. et al. Laboratory-based surveillance of hospital-acquired respiratory virus infection in a tertiary care hospital. Am. J. Infect. Control 45, e45–e47. https://doi.org/10.1016/j.ajic.2017.01.009 (2017).
Sato, M. et al. Molecular epidemiology of respiratory syncytial virus infections among children with acute respiratory symptoms in a community over three seasons. J. Clin. Microbiol. 43, 36–40. https://doi.org/10.1128/JCM.43.1.36-40.2005 (2005).
White, L. J., Waris, M., Cane, P. A., Nokes, D. J. & Medley, G. F. The transmission dynamics of groups A and B human respiratory syncytial virus (hRSV) in England and Wales and Finland: seasonality and cross-protection. Epidemiol. Infect. 133, 279–289. https://doi.org/10.1017/s0950268804003450 (2005).
Vandini, S., Biagi, C. & Lanari, M. Respiratory syncytial virus: the influence of serotype and genotype variability on clinical course of infection. Int. J. Mol. Sci. https://doi.org/10.3390/ijms18081717 (2017).
Han, L. L., Alexander, J. P. & Anderson, L. J. Respiratory syncytial virus pneumonia among the elderly: an assessment of disease burden. J. Infect. Dis. 179, 25–30. https://doi.org/10.1086/314567 (1999).
Neemann, K. & Freifeld, A. Respiratory syncytial virus in hematopoietic stem cell transplantation and solid-organ transplantation. Curr. Infect. Dis. Rep. 17, 490. https://doi.org/10.1007/s11908-015-0490-9 (2015).
Whimbey, E. et al. Respiratory syncytial virus pneumonia in hospitalized adult patients with leukemia. Clin. Infect. Dis. 21, 376–379 (1995).
Park, S. Y. et al. Factors predicting life-threatening infections with respiratory syncytial virus in adult patients. Infect. Dis. (Lond) 49, 333–340. https://doi.org/10.1080/23744235.2016.1260769 (2017).
Datta, S., Walsh, E. E., Peterson, D. R. & Falsey, A. R. Can Analysis of routine viral testing provide accurate estimates of respiratory syncytial virus disease burden in adults?. J. Infect. Dis. 215, 1706–1710. https://doi.org/10.1093/infdis/jix196 (2017).
Author information
Authors and Affiliations
Contributions
J.G.Y., J.Y.N., J.Y.S., W.J.K. and H.J.C. designed the study. W.S.C., J.J.P. and Y.B.S. supported data collection and analysis. J.G.Y. also analyzed data and wrote the paper. All authors contributed to the discussion, edited the paper and confirmed the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yoon, J.G., Noh, J.Y., Choi, W.S. et al. Clinical characteristics and disease burden of respiratory syncytial virus infection among hospitalized adults. Sci Rep 10, 12106 (2020). https://doi.org/10.1038/s41598-020-69017-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-69017-8
- Springer Nature Limited