Abstract
Isotretinoin (ISO) is a drug which is used for the treatment of severe and refractory acne vulgaris (AV), over the last few decades. The drug has various musculoskeletal side effects. The aim of this study was to investigate relationship between serum 25 hydroxy (OH) vitamin D levels and the ISO-induced musculoskeletal side effects in patients with AV. We included 87 patients receiving ISO and had musculoskeletal symptoms as adverse effect (AE) group. Another 90 patients receiving ISO for AV and had any musculoskeletal complaints were recruited as control (C) group. Locomotor system examination of the patients was performed by the same clinician. Serum 25 OH vitamin D levels of the all participants were measured. Patients in the AE group were divided into three subgroups by serum 25 OH vitamin D levels. Patients with serum 25 OH vitamin D level lower than 10 ng/ml was classified as Group I, the ones between 10–20 ng/ml as Group II and those higher than 20 ng/ml were classified as Group III. AE and C groups were similar in terms of age and sex (p > 0.05). There was no statistically significant difference in the mean serum vitamin D levels between two groups (p = 0.17). Also, there was no significant difference in number of arthralgia (p = 0.30), myalgia (p = 0.29), low back pain (p = 0.10) and sacroiliitis (p = 0.17) between three subgroups in AE group. In addition, we found no statistically significant correlation between the serum vitamin D levels and age, cumulative dose of ISO, arthralgia, myalgia and sacroiliitis parameters in AE group (p > 0.05). Serum 25 OH vitamin D levels between the AE and C groups were similar. We also found that no significant difference in musculoskeletal adverse events between AE subgroups. Therefore, it can be concluded that vitamin D deficiency has no effect on the musculoskeletal adverse events in patients receiving ISO.
Similar content being viewed by others
Introduction
Acne vulgaris (AV) is the most common chronic inflammatory skin disease among the adolescents. It affects more than 80% of teenagers. It is estimated that 9.4% of the world population is affected by AV. AV may cause psychological and social disorders related to anxiety due to facial scarring and reduced self esteem, these are significant burden on the affected patients.
Isotretinoin (ISO) is 13-cis-retinoic acid, a synthetic vitamin A analogue and the most effective drug in treatment of recalcitrant AV for more than three decades1,2,3,4,5. The usual starting dose is 1–2 mg/kg/day to achieve a cumulative dose of 120–150 mg/kg over 4–5 months.
ISO has a wide spectrum of adverse effects on multiorgan systems, including reproductive, cutaneous, ocular, neurological, musculoskeletal, and hepatic. It may cause teratogenicity, hepatitis, dryness of skin, psychological effects and cerebral ischemia. Most of these adverse effects induced by ISO are predictable, dose-dependent and manageable. More than half of all adverse events associated with ISO are mucocutaneous and occur especially in the first weeks of treatment6,7,8. The rheumatic side effects are the most common one which are musculoskeletal pains and arthralgia, occuring in 16% patients receiving ISO. Mild, transient myalgias and arthralgias are very common and do not require cessation of the drug9,10. The other musculoskeletal side effects of ISO are calcification of tendon and ligaments, diffuse idiopathic skeletal hyperostosis (DISH syndrome), elevated creatine phosphokinase and cramps10. There are also several case reports on ISO-induced sacroiliitis in the literature, mostly in recent years11,12,13,14,15,16.
The association ISO and vitamin D levels was evaluated by several studies in the literature17,18,19. However, the relationship between ISO-induced musculoskeletal side effects in AV patients and serum vitamin D levels has not been investigated until now. To the best our knowledge, this is the first study to evaluate relationship between the serum vitamin D levels and ISO-induced musculoskeletal adverse effects.
Methods
Study design
This study was designed as a cross-sectional controlled, single center study at Health Sciences University Ankara Training and Research Hospital, Departments of Physical Medicine- Rehabilitation and Dermatology, between April 2019 and September 2019. The study protocol of the study was approved by institutional clinical trials ethics committee with the number of 74.765,13.03.2019 and registered on ClinicalTrials.gov (NCT04204304). The patients were informed about the study and written consent was obtained from all participants. The study was performed in accordance with the ethical standards specified in the 1964 Declaration of Helsinki and its later amendments.
Eligibility
In this study, 87 patients receiving ISO for AV with musculoskeletal adverse effects were classified as AE group. Age- and sex-matched 90 consecutive patients receiving ISO without any musculoskeletal symptoms were classified as C group. The patients over 18 years of age and receiving ISO for at least one month were included the study.
ISO was started with the dose of 0.5–1 mg/kg/day and continued to achieve a total cumulative dose of 120 mg/kg over 6 months.
The ones using vitamin D and/or calcium supplements for the last three months were not included. Patients who had renal, gastrointestinal, skeletal, psychiatric, hematological, endocrine disorders related with thyroid and bone metabolism, also, patients using drugs such as diuretics, multivitamins, anticonvulsants, glucocorticoids, erythromycin, estrogen compound pills, alcohol, vitamin D and/or calcium preparations in the last 3 months, patients with malignancy, chronic liver and kidney failure, history of psoralen and ultraviolet A (PUVA) and women expecting pregnancy were excluded from the study.
Assessments during the study
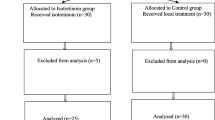
The demographic and clinical characteristics of the participants were noted. Age and sex of the participants, treatment duration and adverse events induced with ISO were recorded. The cumulative ISO dose was calculated. The study flowchart is shown in Fig. 1.
Physical examination of the patients was performed by the same experienced clinician. The musculoskeletal symptoms including arthralgia, low back pain, calcification of tendon and ligaments, polyneuropathy, DISH syndrome, myalgia, cramps and sacroiliitis were assessed. It was queried that whether musculoskeletal symptoms have occurred after ISO treatment. Inflammatory low back pain was evaluated by Assessment of Spondyloarthritis International Society (ASAS) criteria. The ASAS criteria consist of onset at the age of 40, insidious onset, improvement with exercise, no improvement with rest and nocturnal pain (improving with rising). Inflammatory low back pain is diagnosed in the presence of these four criteria. Patients with such criteria were assessed by a clinician in the physical medicine and rehabilitation department. Sacroiliac joint radiography was requested in patients meeting the ASAS criteria. Magnetic resonance imaging of the sacroiliac joints was used to diagnose sacroiliitis in suspected patients. The serum 25 OH vitamin D levels were measured by radioimmunoassay for all the participants. These results showed that patients in AE group were divided into three subgroups according to the serum 25 OH vitamin D levels. The patients with serum 25 OH vitamin D level is lower than 10 ng/ml, was classified as Group I, between 10–20 ng/ml, as Group II, higher than 20 ng/ml as Group III.
Power analysis
The power analysis of the present study was conducted using the software package, G*Power Ver.3.1 (Germany)20. The power analysis revealed that this study had 90% power using type I error (α) = 0.05, effect size = 0.5, and a two-sided t test.
Statistical analysis
Statistical analysis was performed using SPSS version 21.0 (IBM Corp., Armonk, NY, USA). Kolmogorov-Smirnov test was used to evaluate the normality of data distribution. Normal distribution data were expressed as mean (±standard deviation), and data not conforming to normal distribution were expressed as median (interquartile distribution (iqd)). Independent samples t test was used to compare the study groups. Kruskal Wallis test was used to compare cumulative ISO dose between the study groups. The relationship between serum 25 OH vitamin D level and cumulative dose of ISO was calculated by using Spearman’s correlation analysis. Pearson correlation analysis was used to assess the relationship between the serum 25 OH vitamin D level and demographic/clinical characteristics of the patients in AE group. Pearson Chi-square test was used for comparison of the subgroups in terms of arthralgia, myalgia, low back pain and sacroiliitis. p < 0.05 was considered statistically significant for all tests.
Ethics approval and consent to participate
This study was approved by the Health Sciences University, Ankara Training and Research Hospital, Clinical Trials Ethics Committee (no: 74.765, 13.03.2019). Please see Supplementary information.
Consent for publication
Informed consent was obtained from all the participants for publication of this study.
Results
In this study, we evaluated 87 patients with musculoskeletal symptoms related with ISO and 90 patients without any musculoskeletal symptoms in terms of serum 25 OH vitamin D level.
67 of patients in AE group were female and 20 were male. The mean age of the patients in AE group was 20.8 ± 4.0. The C group consisted of 68 females and 22 males. The mean age of the C group was 22.1 ± 4.0 years. There was no significant difference in age and sex between the groups (p = 0.18, p = 0.12, respectively).
The mean serum 25 OH vitamin D level of the patients was 13.5 ± 6.9 ng/ml (range 3.0 to 37.9) in AE group and 12.1 ± 5.6 ng/ml (range 4.0 to 31.5) in C group. There was no statistically significant difference in the serum vitamin D levels between two groups (p = 0.17). The mean duration of ISO treatment was 3.4 ± 1.9 (1–8) months in AE group and 3.7 ± 2.2 (2–7) months in C group. The median cumulative dose of ISO was 2400 (3000) mg for AE group and 2800 (3200) mg for C group. There was no significant difference in cumulative dose of ISO and treatment duration between the groups (p = 0.31, p = 0.43, respectively).
The demographic and clinical characteristics of two groups are presented in Table 1.
The patients in AE group were divided into three subgroups according to the serum vitamin D levels. The patients whose serum 25 OH vitamin D level is lower than 10 ng/ml were classified as Group I, between 10–20 ng/ml as Group II and higher than 20 ng/ml as Group III. There were 32 patients in Group I, 29 patients in Group II and 26 patients in Group III. We found no statistically significant difference in age and sex between the subgroups (p = 0,18, p = 0,20, respectively). The mean serum 25 OH vitamin D levels was 7 ± 1.9 ng/ml in Group I, 14.7 ± 2.6 ng/ml in Group II and 26.1 ± 1.6 ng/ml in Group III. There was a significant difference in serum vitamin D levels between the subgroups (p < 0.001). The characteristics of subgroups in AE group are shown in Table 2.
In AE group, 42 (48.3%) patients had arthralgia, 47 (54%) had myalgia, 59 (67.8%) had low back pain and 12 (12.6%) had sacroiliitis. There was no statistically significant difference between the subgroups in terms of arthralgia (p = 0.30), myalgia (p = 0.29), low back pain (p = 0.10) and sacroiliitis (p = 0.17).
We did not find any correlation between the serum 25 OH vitamin D levels and age, cumulative dose of ISO, treatment duration, arthralgia, myalgia, low back pain and sacroiliitis parameters in AE group (all p > 0.05). The results of correlation analysis between the serum vitamin D levels and demographic and clinical characteristics of the patients in AE group are summarized in Table 3.
Discussion
In this study, we investigated whether there was a relationship between serum vitamin D levels and musculoskeletal adverse effects of ISO in AV patients. We did not find any significant difference in terms of serum vitamin D levels between the AE and C groups. In addition, there was no significant difference in frequency of ISO-induced adverse effects between the subgroups in AE group.
AV is a chronic inflammatory disease of the pilosebaceous unit. Although, its pathogenesis is not clearly understood, follicular hyperkeratinization, increased sebum production, propionibacterium acnes and inflammation have been reported to play a role5,6.
Recently, it is found that vitamin D deficiency is associated with many chronic diseases including cancers, cardiovascular diseases, metabolic syndrome, infectious and autoimmune skin diseases, also, AV19,21,22. It is considered that vitamin D is important not only in calcium homeostasis, but also in immune system regulation, cell growth and differentiation23. Vitamin D modulates the immune system and the proliferation and differentiation of the keratinocytes and sebocytes. Vitamin D is also known as anticomedogenic and antioxidant. The deficiency of vitamin D may facilitate the pathogenesis of AV6,19. The relationship between vitamin D and AV depends on possible anti-inflammatory effects of vitamin D24.
There are several studies to investigate relationship between serum levels of vitamin D and AV with inconsistent results, in the literature. There was no association between serum vitamin D level and AV in some of the studies21,22,23,24,25. Some studies, in contrast, revealed that significantly lower serum vitamin D level in acne patients compared to the healthy controls26,27,28. Yildizgören et al. evaluated a total of 43 patients with newly diagnosed nodulocystic acne and 46 healthy control subjects according to their 25 OH D levels27. The authors found that the patients with nodulocystic acne had significantly lower serum vitamin D levels compared with the control group. Moreover, a review and meta-analysis showed that lower serum vitamin D level and higher prevalence of vitamin D deficiency in patients with AV28. The findings of these studies suggest that there is a relationship between low vitamin D levels and AV. The two study groups also have AV and there was no significant difference in terms of the serum vitamin D levels between the study groups, in our study.
Recently, El-Hamd et al. performed a study including 90 patients with AV and age- and sex-matched 60 healthy controls. They found that the baseline serum 25 OH vitamin D levels were significantly lower in patients with AV than control group. The patients were treated with ISO dose of 0.75 mg/kg/day for a period of 3 months. After 3 months of ISO treatment, serum 25 OH vitamin D levels have increased significantly in patients with AV. The authors also found an inverse correlation between serum level of 25 OH vitamin D and severity of AV, before the treatment. They have reported that vitamin D may play a potential role in pathogenesis of the AV or AV may have a negative impact on vitamin D synthesis19. In contrast to this study, Toossi et al. found no significant difference in serum 25 OH vitamin D levels between AV patients and healthy controls. They also indicated no correlation between serum vitamin D levels and severity of AV25.
The effects of ISO on bone metabolism and bone physiology also have been investigated with several studies. ISO is a synthetic vitamin A analogue. Frankel et al. found that chronically vitamin A overdosed rats had increased osteoclastic activity, reduced osteoid formation, and reduced levels of 25 OH vitamin D29.
Miziolek et al. indicated that excessive intake of vitamin A may deteriorate functioning of vitamin D especially in subjects with a vitamin D deficiency (<50 nmol/l of 25 OH vitamin D), therefore a similar side effect may also appear in patients using ISO. The authors suggested that decreasing the use of ISO after bone injury or continuing the treatment at low dose with a concomitant correction of vitamin D and calcium status30. The vitamin D deficiency may be a condition predisposing to osteoporosis and decreased bone mineral density31. In fact, Boucher suggested that a measurement of serum 25 OH vitamin D and correction of vitamin D deficiency appear to be advisable before starting ISO treatment32. We did not find any correlation between serum vitamin D levels and cumulative ISO dose, ISO-induced musculoskeletal side effects. In our study, Group I had the lowest serum vitamin D level, but there was no significant difference between Group I, II and III in frequency of the musculoskeletal side effects. Therefore, according to our results, we are considering that the measurement or correction of 25 OH vitamin D deficiency is not necessary before ISO treatment for AV.
Ertugrul et al.18 investigated 35 females and 15 males with AV and measured 25 (OH) vitamin D, 1,25 dihydroxy vitamin D, and bone alkaline phosphatase, calcium, phosphate, and parathormone levels before and after 3 months of ISO treatment. They revealed that 1,25 dihydroxy vitamin D, parathormone, and bone alkaline phosphatase levels increased significantly after 3 months of ISO treatment. Hovewer, 25 OH vitamin D and calcium levels were significantly decreased after the treatment. They reported that ISO has an impact on vitamin D metabolism18. We found no correlation between serum vitamin D levels and cumulative ISO dose of the patients with AV.
There are limitations of this study. Since, our study is a cross-sectional study, it is important to support the relationship between the serum level of 25 OH vitamin D and ISO-induced musculoskeletal symptoms with larger patient groups and further prospective randomized controlled trials.
Conclusion
We may conclude according to our results that, there is no relationship between the serum levels of 25 OH vitamin D and musculoskeletal side effects in AV patients. It is indicated that vitamin D deficiency have no effect on the musculoskeletal symptoms in patients receiving ISO for AV. Therefore, the measurement of serum 25 OH vitamin D level or intake of vitamin D supplements is not necessary before ISO treatment in patients with AV.
References
Tan, J. K. & Bhate, K. A global perspective on the epidemiology of acne. Br. J. Dermatol. 172(1), 3–12 (2015).
Wysowski, D. K., Swann, J. & Vega, A. Use of isotretinoin (Accutane) in the United States: Rapid increase from 1992 through 2000. J. Am. Acad. Dermatol. 46(4), 505–509 (2002).
Akman, A. et al. Treatment of acne with intermittent and conventional isotretinoin: a randomized, controlled multicenter study. Arch. Dermatol. Res. 299(10), 467–473 (2007).
Charakida, A., Mouser, P. E. & Chu, A. C. Safety and side effects of the acne drug, oral isotretinoin. Expert Opin. Drug Saf. 3(2), 119–129 (2004).
Leyden, J. J., Del Rosso, J. Q. & Baum, E. W. The Use of Isotretinoin in the Treatment of Acne Vulgaris: Clinical Considerations and Future Directions. J. Clin. Aesthet. Dermatol. 7(2), 3–21 (2014).
Stewart, T. J. & Bazergy, C. Hormonal and dietary factors in acne vulgaris versus controls Dermatoendocrinol, https://doi.org/10.1080/19381980.2018.1442160 (2018).
Demirseren, D. D. et al. The weeks and the cumulative doses of the first adverse events related to oral isotretinoin in acne patients: analysis of 300 patients. Journal of Dermatological Treatment 28(4), 309–313 (2017).
Rademaker, M. Adverse effects of isotretinoin: a retrospective review of 1743 patients started on isotretinoin. Australas J Dermatol. 1, 248–253 (2010).
Knitzer, R. H. & Needleman, B. W. Musculoskeletal syndromes associated with acne. Semin. Arthritis Rheum. 20(4), 247–255 (1991).
Saurat, J. H. Side effects of systemic retinoids and their clinical management. J Am. Acad. Dermatol. 27, 23–28 (1992).
Baykal Selçuk, L., Aksu Arıca, D., Baykal Şahin, H., Yaylı, S. & Bahadır, S. The prevalence of sacroiliitis in patients with acne vulgaris using isotretinoin. Cutan. Ocul. Toxicol. 36(2), 176–179 (2017).
Dawoud, N. M., Elnady, B. M., Elkhouly, T. & Yosef, A. Adalimumab as a successful treatment for acne fulminans and bilateral acute sacroiliitis with hip synovitis complicating isotretinoin therapy. Indian J. Dermatol. Venereol. Leprol. 84(1), 104–107 (2018).
Bachmeyer, C. et al. Isotretinoin-induced bilateral sacroiliitis. Dermatology 206, 285–286 (2003).
Barbareschi, M. et al. Unilateral sacroiliitis associated with systemic isotretinoin treatment. Int. J. Dermatol. 49, 331–333 (2010).
Rozin, A. P., Kagna, O. & Shiller, Y. Sacroiliitis and severe disability due to isotretinoin therapy. Rheumatol Int. 30, 985–986 (2010).
Levinson, M., Gibson, A. & Stephenson, G. Sacroiliitis secondary to isotretinoin. Australas J. Dermatol. 53(4), 298–300 (2012).
Neema, S. et al. Vitamin D Deficiency After Oral Retinoid Therapy for Ichthyosis. Pediatr Dermatol., https://doi.org/10.1111/pde.12614 (2015).
Ertugrul, D. T., Karadag, A. S., Tutal, E. & Akin, K. O. Therapeutic hotline. Does isotretinoin have effect on vitamin D physiology and bone metabolism in acne patients? Dermatol Ther. 24(2), 291–295 (2011).
El-Hamd, M. A., El Taieb, M. A., Ibrahim, H. M. & Aly, S. S. Vitamin D levels in acne vulgaris patients treated with oral isotretinoin. J. Cosmet. Dermatol. 18(1), 16–20 (2019).
Faul, F., Erdfelder, E., Lang, A. G. & Buchner, A. G*Power 3: a flexible statistical power analysis program for the social, behavioral,and biomedicalsciences. Behav Res Methods 39(2), 175–191 (2007).
Holick, M. F. Vitamin D: a D-lightful health perspective. Nutr. Rev. 66, 182–194 (2008).
Hyppönen, E., Boucher, B. J., Berry, D. J. & Power, C. 25-hydroxyvitamin D, IGF-1, and metabolic syndrom at 45 years of age: a cross-sectional study in the 1958 British Birth Cohort. Diabetes 57, 298–305 (2008).
Lee, W. J., Choi, Y. H., Sohn, M. Y., Lee, S. J. & Kim, D. W. Expression of Inflammatory Biomarkers from Cultured Sebocytes was Influenced by Treatment with Vitamin D. Indian J Dermatol. 58(4), 327 (2013).
Al-Taiar, A. et al. Plasma 25-Hydroxy Vitamin D is not Associated with Acne Vulgaris. Nutrients. https://doi.org/10.3390/nu10101525 (2018).
Toosi, P. et al. Serum 25-hydoxy vitamin D levels in patients with acne vulgaris and its association with disease severity. Clin. Cases in Min. Bone Metab. 12(3), 238–242 (2015).
Lim, S. K. et al. Comparison of vitamin D levels in patients with and without acne; A case-control study combined with a randomised controlled trial. Plos One. https://doi.org/10.1371/journal.pone.0161162 (2016).
Yildizgoren, M. T. & Togral, A. K. Preliminary evidence for vitamin D deficiency in nodulocystic acne. Dermatoendocrinol. https://doi.org/10.4161/derm.29799 (2015).
Acharya, P. & Mathur, M. Vitamin D deficiency in patients with acne vulgaris: A systematic review and meta-analysis. Australas J Dermatol. https://doi.org/10.1111/ajd.13165 (2019).
Frankel, T. L., Seshadri, M. S., McDowall, D. B. & Cornish, C. J. Hypervitaminosis A and calcium-regulating hormones in the rat. J Nutr. 116(4), 578–587 (1986).
Miziołek, B., Bergler-Czop, B., Stańkowska, A. & Brzezińska-Wcisło, L. The safety of isotretinoin treatment in patients with bone fractures. Postepy Dermatol Alergol. 36(1), 18–24 (2019).
Bhambri, R. et al. Changes in bone mineral density following treatment of osteomalacia. J Clin Densitom 9, 120–127 (2006).
Boucher, B. J. Serum retinol levels and fracture risk. N Engl J Med. 348(19), 1927–1928 (2003).
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
C.M.: study concept and design; drafting of the manuscript; C.M. and N.K.: data collection; analysis and interpretation of data; all authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mülkoğlu, C., Karaosmanoğlu, N. Effect of Serum 25 Hydroxy Vitamin D Level on Isotretinoin-Induced Musculoskeletal Symptoms: A Cross-Sectional Study. Sci Rep 10, 2245 (2020). https://doi.org/10.1038/s41598-020-59167-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-59167-0
- Springer Nature Limited