Abstract
Economic evaluations are tools for assessing emerging technologies and a complement for decision-making in healthcare systems. However, this topic may not be familiar for doctors and academics, who may be confused when interpreting the results of studies using these tools. Cataract is a disease which has received special attention in healthcare systems due to its high incidence, the great impact that it could have on patients’ quality of life, and the fact that it can be definitively solved in almost all cases through cataract surgery. Historically, economic evaluations in cataract surgery have been conducted for many purposes by simply assessing whether the surgery is cost-effective for specific questions related to the implantation of multifocal intraocular lenses, surgical techniques, optimizing assessments, preventing diseases or complications, etc. Moreover, although there are systematic reviews about cataract surgery and narrative reviews introducing the concept of economic evaluations, as far as we know, no previous study has been conducted that synthesizes and integrates evidence coming from both fields. Thus, the purpose of this narrative review is to introduce doctors and academics to economic evaluation tools, to describe how these have been historically applied to cataract surgery, and to provide special considerations for the correct interpretation of economic studies.
摘要
经济评价是评估新兴技术的工具, 也是医保系统决策的补充。然而, 医生和学者对此并不熟悉, 他们在使用这些工具解释研究结果时可能会感到困惑。白内障是在医疗系统中受到特别关注的眼病, 因为其发病率高, 对患者的生活质量影响大, 几乎所有 (因白内障视力低下的) 病例都可以通过白内障手术解决。从历史上看, 白内障手术的经济评价有很多目的, 通过简单地评估手术是否具有成本效益来解决与多焦人工晶状体植入、手术技术、优化评估、预防疾病或并发症等相关的特定问题。此外, 尽管有关于白内障手术的系统综述和引入经济评价概念的综述, 但目前还没有综合和整合这两个领域证据的研究。因此, 本叙述性综述旨在向医生和学者介绍经济评价工具, 描述这些工具在历史上如何应用于白内障手术, 并提供正确解读经济研究的特别注意事项。
Similar content being viewed by others
Introduction
Economic evaluations of health care arise from the fact that health service resources are scarce. Patients require treatment and doctors can sometimes select between different treatments for the same disease. However, they often have to make choices that maximize health gains using the smallest possible resource consumption [1]. Faced with this problem, it can be considered that reducing costs is the only simple solution. However, decision making in healthcare goes beyond accounting or attempting to reduce costs [1]. Economic evaluation is the tool that economists and healthcare providers use as a source of information considered to make the best decisions.
Although the idea of shedding light on the use of resources and to provide information that enables the improvement of decision-making dates back to the 17th-century [2], the knowledge of many doctors in this area remains vague. Several techniques for economic evaluation have been described, and sometimes these are incorrectly labeled. This fact seems coherent, because the same terms can be used in different evaluations. For instance, as detailed below, cost-effectiveness and cost-utility are two different cost-evaluation techniques, but in both cases, a procedure is or is not cost-effective, independent of the technique used.
Economic studies have provided interesting and useful information on cataract surgery. For instance, it is known that patients are more comfortable paying for potential enhancements in cataract surgery, especially when positive feedback is provided by their family [3]. However, this position to pay for surgery may be below the actual cost of screening, transport, accommodation, and surgery in settings where people are used to free services or in low-income countries [4, 5]. This example provides a clear picture of the complexity of economic analyses, in which conclusions can radically change depending on the timeframe, perspectives, locations, etc.
Substantial evidence exists regarding the cost-effectiveness of cataract surgery. Cataract surgery increased its cost-effectiveness by 41.8% in 2018 compared to 2012 and by 73.7% in comparison to 2000 [6,7,8]. The cost-effectiveness of surgery with intraocular lens (IOL) implantation has been demonstrated not only for high-income [9, 10], but also for low-income countries [11, 12]. Despite these benefits, cataract surgery is still not accessible in some low-income areas with very low willingness-to-pay from patients [5]. Fortunately, these populations and ophthalmologic residents can benefit together, since it has also been demonstrated that resident-performed surgeries are cost-effective [13].
Although there is a general consensus on the cost-effectiveness of cataract surgery [6,7,8], there are some specific topics, such as the economic evaluation types or which procedures related to cataract surgery are cost-effective, that could be confusing or require further studies. Cataract is a topic that has been widely reviewed [14,15,16], but there is a lack of studies synthesizing the findings provided by economic evaluations in this field. The aim of this narrative review is to introduce doctors and academics to economic evaluation tools, to describe how these have been historically applied to cataract surgery, and to provide special considerations for the correct interpretation of economic studies. For achieving these purposes, these findings will be described according to the evaluation type and perspective in such a way that the reader without experience in economic evaluations can understand the advances in the area over the years and the future research opportunities.
Methods
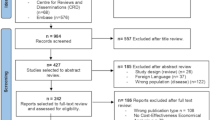
A non-systematic literature search was performed in June 2021 using the following bibliographical databases: The National Library of Medicine (PubMed), EMBASE and Web of Science (WOS). The key words used in the strategy search were (“cost-effectiveness” OR “cost-utility”) AND “cataracts”. A snowball approach was also used to find relevant references. The inclusion criteria encompassed full and partial economic evaluations of original articles conducting a cost-utility analysis or cost-effectiveness analysis related to cataract surgery. No restrictions were applied in terms of study design, with the only exclusion from the narrative review of non-English written papers.
Economic evaluation techniques
Embarking on a full economic evaluation should consider some important points: (1) deciding the intervention of interest, (2) selecting the control intervention/s, (3) defining the viewpoint or perspective, (4) selecting the economic evaluation type, (5) compiling the benefits and costs, (6) selecting the analysis model, and (7) proceeding with the analysis [17]. At this point, it is important to note that some studies on health economics only include the costs or efficacy of only a single intervention, and therefore are partial economic evaluations [18, 19]. Although these partial evaluations can provide valuable information, they cannot guide decision making [18]. For full economic evaluations, both efficacy and costs should be evaluated, as it is indicated in Fig. 1 [20].
Build on basis to the UK Health Security Agency Cost utility analysis definitions [20].
The first two steps, to decide the control and intervention/s of interest, are fundamental in any economic evaluation. The main question at this stage is how many interventions are planned to be analyzed considering a minimum of two. Then, the definition of viewpoint or perspective holds great importance for conducting and interpreting economic evaluations. Interpretation could completely differ depending on the perspective defined. For instance, switching from delayed cataract surgery to immediate sequential could yield benefits from the perspectives of payers, patients and society [21, 22], by minimizing the costs. Conversely, it could result in a loss of benefits from the physician’s perspective [23].
The perspective will be also one of the factors that influence the decision on the next step, which is the selection of the economic evaluation technique among the following: (1) cost-effectiveness, (2) cost-minimization, (3) cost-utility, (4) cost-benefit, and (5) cost-consequence. Some key points are critical to differentiate them. First, two parameters should be considered in the evaluation, the costs associated with the treatment and the outcome, which is the measure of the efficacy endpoint obtained from a clinical trial (i.e. visual acuity, patient-reported outcomes, etc.). Both parameters summarize the first evaluation type “cost-effectiveness” [24]. If there is no difference in effectiveness between interventions, only costs could be considered in a “cost-minimization” study type [25, 26].
An important limitation of cost-effectiveness studies is that decisions can only be made from a narrow perspective. This is due to differences in the measurement units between diseases or procedures, not allowing the comparison between studies from different medical specialties. Another important limitation is that only health care benefits are considered as efficacy end-points.
“Cost-utility” evaluations are a particular extension of cost-effectiveness, but with the main difference in the selected outcome variable. Whereas cost-effectiveness can use outcome variables directly related with the specialty, such as the spectacle dependence in the selection of a monofocal or a multifocal intraocular lens in cataract surgery [27], cost utility evaluations require of an outcome variable common between different specialties. An example of this may be the use of patient-reported outcomes such as the quality of life as efficacy end-point, while considering a timeline period that could be extended up to death [28]. This particular consideration of quality of life adjusted to years of life is known as “QALYs”, and it is accepted as the standard variable for cost-utility analysis. The advantages are the use of a common variable that allows the comparison between interventions, being applicable to decision making from a broad perspective. Unfortunately, patient-reported outcomes are more subjective and less precise than other variables such as visual acuity. Therefore, it might not be able to detect small benefits between interventions.
Broadening the viewpoint to a societal perspective and including other benefits beyond the health care benefits such as productivity increase, well-being, comfort, etc., requires from other economic evaluation type known as “cost-benefit” [29]. The benefits in this type of evaluations are standardized in monetary terms, allowing the comparison in a broad perspective. Conversely, standardization in monetary terms is not easy. Finally, “cost-consequence” analysis shares some characteristics with cost-benefit but with the difference that the benefits included in the analysis are managed separately. This allows the exploration of results only for those benefits of interest, rather than treating them as a whole [30]. Cost-consequence are especially useful at the early stage of the product and with complex products with several benefits, when it is not clear which cost and benefits are the most relevant.
In summary, it is crucial for doctors and academics to recognize that full economic evaluations always compare at least two interventions, the collection of cost and efficacy variables and depending on the perspective, different economic evaluation techniques could be selected. Specifically, these techniques can be selected from cost-efficacy / cost minimization based on a narrow perspective affecting decisions of single patients, group or departments, to cost-utility, cost-benefit and cost-consequences based on a broad perspective that involve different departments, hospitals, society, etc. Figure 1 is shown to help the reader to easily identify the type of analyses in any study involving economic evaluations.
Understanding variables for economic evaluations
In the previous section, one of the differences described between cost-effectiveness and cost-utility techniques was the measurement variable of effectiveness. Whereas for cost-effectiveness, psychophysical variables such as visual acuity can be used, variables that allow the comparison between different specialties or diseases are required for cost-utility (i.e. for the comparison between eye diseases and systemic diseases). Ophthalmologists are very familiar with the use of objective and subjective metrics to characterize the eye’s state, such as optical aberrations and visual acuity, respectively. Even, albeit to a lesser extent, they are familiar with using patient-reported outcomes to measure psychometric domains such as visual function (visual function questionnaire, VF-14). However, they probably find in the “utility” measure a concept required to be described, even though it has been in use for decades [31].
Utility is a cardinal measure of the strength of one’s preference standardized outcome to a range between 0 (poorest health condition) and 1 (perfect health condition) [31, 32]. In other words, utility is the perceived value that individuals receive from the consumption of healthcare goods/services [18]. In Health, the Quality of Life (HRQoL) has been considered as the standard utility variable for making comparison between different actions. Thus, the consumption of healthcare goods/services affect to patient’s HRQoL. In addition, it is relevant to note that a healthcare action can affect to HRQoL during a short/long period of time up to death. Therefore, the HRQoL (also named utilities) could be related to the quantity of life (measured in years), resulting to a bidimensional variable named Quality-Adjusted Life-Years (QALYs) [31]. Figure 2 shows an example of 2.3 QALYs increase due to a longer life expectancy of one year, with an increase in utility of 0.3 points.
For ophthalmologists, HRQoL can be assessed using questionnaires that evaluate the difficulties due to vision in conducting daily tasks. For example, the results of the VF-14 tool can be considered as a HRQoL measurement. The problem of using this questionnaire as a HRQoL tool is that it does not allow the comparison between other health specialties, therefore it can be regarded as an ophthalmic index. Consequently, cost-utility analyses cannot be conducted with these ophthalmic indices and should be described as cost-effectiveness tools. Furthermore, to adjust HRQoL to life-years, it is necessary to know how many life-years patients would be willing to sacrifice for an improvement in HRQoL up to death. To address this issue, the time trade-off (TTO) is estimated by means of doing a previous study before conducting the economic evaluation.
In the field of vision science, TTO has been estimated for improvements of visual acuity (visual trade-offs). This answer the question “how many years of life patients are willing to invest to improve the visual acuity up to the maximum health state (20/20)?” This variable has been used as the “utility” for cost-utility studies [7], and it is calculated as 1 – TTO/(Expect to live). For example, for those patients with 20/40 expecting to live a mean of 20 years, they would invest 2 of each 10 years of life if they can achieve 20/20. The computed utility score for this situation is therefore 1-4/20 = 0.8 [33]. The calculation of utility values from visual acuity has been modeled for prediction [34], but the utility value depending on visual acuity has been reported considerably different between studies for different populations and impairment of visual acuity at several distances [33, 35,36,37]. The utility score would change depending on the baseline state of visual acuity, and therefore a poorer baseline visual acuity will be associated to a lower utility value since patients would invest more years to achieve 20/20 [33, 38, 39].
The TTO method has been historically criticized due to inconsistencies and arbitrariness [40, 41]. This utility score appears to be a forced method to allow the comparison between different specialties, instead of a solid scientifically-based method of measurement. Indeed, other authors have agreed that visual trade-offs limit the comparisons with other medical specialties and limit the use of the standard willingness-to-pay thresholds [42]. Considering the limitations of using other generalized methods of measuring HRQoL, such as EuroQol-5D, the 15-D [43], and the Health Utilities Index Mark 3 (HUI3) [44], which may lack of sensitivity with vision in high-income countries [11, 38], resulting in less utility gains after surgery [35], surgeons should understand that many methods and questionnaires have been used in terms of HRQoL meaning (utility). This could result in important difficulties to interpret economic evaluations. Therefore, these economic evaluations are a complement for taking decisions and not a way for taking decisions due to their potential bias in comparison to other research fields using uniform standardized and less subjective metrics.
Economic evaluations applied to cataract surgery
Surgical techniques
Femtosecond laser cataract surgery (FLACS) has been one of the topics with more studies in comparison to phacoemulsification technique (PCS) [45,46,47,48]. Cost-effectiveness have been conducted in the perspectives of the French [45] and Australian [49] national health-care systems. Also, cost-utility has been evaluated from the United Kingdom [47] national healthcare system perspective. All these studies agreed that FLACS is less cost-effective than PCS for cataract removal in healthy patients[45,46,47]. However, economic evaluations are still required in those groups with a history of trauma, zonulopathy, narrow angles, mature or intumescent cataracts, or Fuchs dystrophy, for which minimizing endothelial cell loss is critical [46]. In addition, the potential benefit of increased refractive accuracy of femtosecond astigmatic keratotomy over manual limbal relaxing incisions should be also evaluated [46].
On the other hand, Jongsareejit et al. [50] and Khan et al. [51] evaluated cost-effectiveness of phacoemulsification versus small incision cataract surgery (MSICS) from societal perspective in Indonesia and India, respectively. Using ophthalmic indices, they concluded that MSICS was more cost-effective than phacoemulsification. These results contrast with those reported by Rochmah et al. [52] using Disability-Adjusted Life Years (DALYs) as effectiveness variable and by Wulandari et al. [53] using the VF-25 tool. On the other hand, Manaf et al. [54] reported a cost of 6$ higher per unit of the VF-14 tool for phacoemulsification surgery in Indonesia. These differences could not be only caused by variables, but also by the context and the time of history in which the evaluation was conducted [55,56,57].
The managing of late in-the-bag intraocular lens dislocation has been also assessed without providing a clear conclusion between repositioning and exchange [58]. Although repositioning was more cost-effective, authors claimed that it was not superior enough to provide recommendations.
Protocols
Immediate sequential has been demonstrated to be more cost-effective than delayed cataract surgery [21, 22, 59, 60] On the other hand, cost-utility for the second eye was suggested to be cost-effective only in the long term unless care costs were included [61]. In the short term, the procedure was not cost-effective for patients with mild preoperative visual dysfunction. These results are in contrast with the cost-utility reported by Busbee et al. [62], who found in a cost-utility analysis that the second-eye cataract surgery was an extremely cost-effective procedure when compared with other interventions across medical specialties. These discrepancies between Sach et al. [61] and Busbee et al. [62] could be explained by the fact of using a general questionnaire and the vision utilities. Thus, Busbee et al. [62] conclusions should be interpreted with caution from a cost-utility analysis, even though questionnaires may be valid from a cost-effectiveness technique, since general questionnaires are more appropriate for drawing general conclusions across specialties. Cataract surgery has been also to be cost-effective for fall prevention [63, 64], even though this efficacy end-point was not improved for the second eye surgery [65].
Beyond surgery protocols, Meltzer et al. [66] reported that the use of telephone calls or transportation subsidies to increase follow-up in low- and middle-income countries of China may not be cost-effective. Jastrzebski et al. [67] proposed a protocol for increasing the cost-effectiveness of the procedure optimizing the patient number of visits from a questionnaire that evaluated the surgery risk. In this line, surgery was even cost-effective in a subpopulation of patients with a lower predicted probability of reporting improved visual functioning after surgery, but a strategy of watchful waiting may be equally effective and considerably less expensive [68]. Cost-effectiveness of tools for grading cataract have been also evaluated [69]. Finally, Hopkins et al. [70] reported that the cost required for reducing waiting times was compensated by means of increasing treatment volumes, resulting in a cost-effective action.
Intraocular lenses
Jain et al. [71] conducted a partial evaluation, only including effectiveness, for small incision cataract surgery with PMMA lenses versus phacoemulsification with foldable lenses. For this purpose, the generic EQ5D-5L questionnaire was used for QALYs and a vision-related questionnaire (IND-VFQ-33). A higher increase of QALYs was reported for foldable lenses. The cost-effectiveness of IOL material has been also evaluated, resulting the hydrophobic acrylic the most cost-effective in 4 European countries [72]. This was mainly due to the lower percentage of required Nd-YAG capsulotomies, but with the limitation of not considering the glistening of this material [73].
Toric intraocular lens implantation for patients with corneal astigmatism higher than 1.25 D in comparison to monofocal IOLs was evaluated by Simons et al. [74]. The authors concluded that from a societal perspective, toric IOLs was not cost-effective, but it is important to highlight that by definition this was a cost-utility study using generic questionnaires for QALYs, which are only sensitive to visual improvements if patients were close to blindness [11].
The use of multifocal IOLs has been also evaluated from the early multifocal IOLs no longer marketed, with a general agreement about its cost-effectiveness [75]. Hu et al. [76] and Bala et al. [77] concluded that multifocal and EDOF IOLs were cost-effective for patients desiring spectacle independence. In any case, it is important to remark some errors in the modeling utilities used. For instance, a decrease in utility of −0.065 for wearing glasses and −0.18 for glare and haloes was stated, which is based on the value of −0.18 for wearing spectacles in a population with cancer [78], which is not transferable to healthy populations, and without knowing from which reference the authors obtained the value of utility decrease for glare and haloes. Lin et al. [79] also reported, using the NEI VFQ-25 for HRQoL, that multifocal IOLs can be highly cost effective for patients who prefer to be spectacle free.
Other authors have also evaluated the cost-effectiveness, but only using the spectacle free variable instead of estimating utilities. De Vries et al. [80] reported that the use of multifocal IOLs reduced 6.4 times the need of buying spectacles, decreasing the lifetime costs compared to monofocal IOL implantation. The willingness-to-pay for a multifocal IOL was set at $5 per day in the 80% of patients according to Maxwell et al. [27], demonstrating that the net benefit of the MF-IOL exceeded its acquisition cost, and the net benefit of the monofocal IOL. This finding was consistent with that from Lafuma et al. [81] who added that any IOL can provide a spectacle independence prevalence rate >80%, and would always yield their average cost savings.
Diseases and cataract planning
Simons et al. [82] investigated the cost-effectiveness of prophylactic treatments against cystoid macular oedema after cataract surgery in patients without diabetes, using the generic health-related quality of life (HRQL) questionnaire for calculating QALYs, and secondary efficacy variables as specific HRQoL questionnaires and visual acuity. After comparing three alternatives, bromfenac, dexamethasone and a combination of both, more cost was associated to the combination, but being more cost-effective due to its higher efficacy.
Detection of diseases could be improved with the incorporation of new technologies as the ocular coherence tomography (OCT). Leung et al. [42] reported in a cost-efficacy analysis including visual trade-offs that the patient and society saved money from deferring a multifocal IOL, and the potential savings of a combined rather than delayed procedure if the patient wanted vitreoretinal surgery.
Conclusions
In this review, doctors and academics without previous knowledge in economic evaluations were introduced in these analyses using examples coming from one of the most studied and familiar topics, cataract surgery. This work aims to establish a general guide that the researcher can use when conducting studies in a context of economic research in the health field. In summary, decision making should involve evaluating both cost and effectiveness, and the viewpoint or perspective (for whom this is cost-effective?) should be considered in the interpretation of the study. Interpretation of economic evaluations is not easy considering the incorrect terms usually used, i.e. several cost-effectiveness studies consulted for this review were really cost-utility evaluations. The difference between these evaluation techniques is mainly managed by the perspective chosen and a graphical conceptual framework was provided in order to easily identify the economic evaluation technique to choose.
On the other hand, the different metrics used to refer to QALYs could challenge the interpretation for the non-expert. For instance, one of the objectives of cost-utility evaluations is to allow the comparison between different diseases or medical specialties, in such a way, information coming from these evaluations could be used for taking decisions from a broad perspective (i.e. societal), however to allow this, general questionnaires should be used such as the EQ-5D or the HUI3. The drawback of these questionnaires is that they are less sensitive to detect visual changes, sometimes required close values to blindness to achieve sensitivity. For this reason, other specific metrics derived from visual acuity such as the visual trade-off or questionnaires for reporting visual outcomes have been used.
It is important to note, that moving from these general questionnaires to the specific questionnaires to define QALYs must be interpreted with caution, and it is more than questionable to talk about cost-utility and broad perspectives, when specific methods of measurement are used. These methods could provide evidence about the cost-effectiveness of a method since these are more sensitive to visual changes but conversely, although the cost-utility could be poorer using general tools of measurement. Considering this, it is reasonable to include both methods in economic evaluations to enable the interpretation from different perspectives. It is essential to consider that, although effectiveness might be maintained on time, prices from technologies decrease and many old cost-efficacy studies should be interpreted with caution at these days, since cost-efficacy could increase with time as it has been reported for cataract surgery in the last 20 years.
Summary
What is known about this topic
-
Economic evaluation is the tool that economists and healthcare providers use as a source of information considered to make the best decisions.
-
There is a general consensus on the cost-effectiveness of cataract surgery but the conclusions in economic analyses can radically change depending on the timeframe, perspectives, locations, etc.
What this study adds
-
Many published economic evaluations wrongly describe the evaluation technique since the perspective chosen does not match the latter.
-
Particular attention should be paid to the variables selected for effectiveness since ophthalmic indices limit comparisons with other medical specialties and generic questionnaires might not be sensitive to visual benefits.
References
Goodacre SW, McCabe C. An introduction to economic evaluation. Emerg Med J 2002;19:198–201.
Jonsson B. Economic evaluation of health care technologies. Acta Endocrinol. 1993;128:50–54.
Ko F, Frick KD, Tzu J, He M, Congdon N. Willingness to pay for potential enhancements to a low-cost cataract surgical package in rural southern China. Acta Ophthalmol. 2012;90:e54–e60. https://www.embase.com/search/results?subaction=viewrecord&id=L51553590&from=export.
Dean WH, Sherwin JC, Kumwenda S, Angeletti M, Wiehler U. Willingness to Pay for Cataract Surgery in Post-operative Cataract Patients in Rural Malawi. Ophthalmic Epidemiol. 2012;19:265–71. https://www.embase.com/search/results?subaction=viewrecord&id=L365658140&from=export.
Shrestha MK. Willingness to pay for cataract surgery in Kathmandu valley. Br J Ophthalmol. 2004;88:319–20. https://www.embase.com/search/results?subaction=viewrecord&id=L38333704&from=export.
Brown GC, Brown MM, Menezes A, Busbee BG, Lieske HB, Lieske PA. Cataract Surgery Cost Utility Revisited in 2012. Ophthalmology. 2013;120:2367–76. https://pubmed.ncbi.nlm.nih.gov/24246824/.
Brown GC, Brown MM, Busbee BG. Cost-utility analysis of cataract surgery in the United States for the year 2018. J Cataract Refract Surg. 2019;45:927–38. https://pubmed.ncbi.nlm.nih.gov/31262482/.
Busbee BG, Brown MM, Brown GC, Sharma S. Incremental cost-effectiveness of initial cataract surgery. Ophthalmology. 2002;109:606–12. https://pubmed.ncbi.nlm.nih.gov/11874769/.
Hiratsuka Y. Cost-utility analysis of cataract surgery in Japan: A probabilistic Markov modeling study. Jpn J Ophthalmol. 2013;57:391–401. https://doi.org/10.1007/s10384-013-0238-8.
Tuominen R, Immonen I, Raivio I. Economic evaluation of cataract surgery: a comparison between IOL and non-IOL techniques. Acta Ophthalmol. 1988;66:577–81.
Griffiths UK, Bozzani FM, Gheorghe A, Mwenge L, Gilbert C. Cost-effectiveness of eye care services in Zambia. Cost Eff Resour Alloc. 2014;12:6 https://pubmed.ncbi.nlm.nih.gov/24568593/.
Marseille E. Cost-effectiveness of cataract surgery in a public health eye care programme in Nepal. Bull World Health Organ. 1996;74:319–24.
Moore DB, Slabaugh MA. Surgical Outcomes and Cost Basis for Resident-Performed Cataract Surgery in an Uninsured Patient Population. JAMA Ophthalmol. 2013;131:891.
Agarwal A, Kumar DA. Cost-effectiveness of cataract surgery. Curr Opin Ophthalmol. 2011;22:15–8.
Schulz CB, Kennedy A, Rymer BC. Trends in ophthalmology journals: a five-year bibliometric analysis (2009-2013). Int J Ophthalmol. 2016;9:1669–75. http://www.ijo.cn/gjyken/ch/reader/view_abstract.aspx?file_no=20161122&flag=1.
Wen P-F, Dong Z-Y, Li B-Z, Jia Y-Q. Bibliometric analysis of literature on cataract research in PubMed (2001–2013). J Cataract Refract Surg 2015;41:1781–3. https://journals.lww.com/02158034-201508000-00031.
Guillemin F, De Wit M, Fautrel B, Grimm S, Joore M, Boonen A. Steps in implementing a health economic evaluation. RMD Open. 2020;6:6–8.
Turner HC, Archer RA, Downey LE, Isaranuwatchai W, Chalkidou K, Jit M, et al. An Introduction to the Main Types of Economic Evaluations Used for Informing Priority Setting and Resource Allocation in Healthcare: Key Features, Uses, and Limitations. Front Public Heal. 2021;9:1–17.
Kapse R, Agarwal S, Rishikeshi N, Deshpande M, Kulkarni S, Deshpand R, et al. Cost analysis of pediatric cataract surgery in a tertiary eye care hospital in Western India. Indian J Ophthalmol. 2022;70:420 https://pubmed.ncbi.nlm.nih.gov/35086208/.
UK Health Security Agency. Cost consequence analysis: health economic studies. Guidance. 2020. Available at: https://www.gov.uk/guidance/cost-consequence-analysis-health-economic-studies. Accessed August 4, 2022.
Neel ST. A cost-minimization analysis comparing immediate sequential cataract surgery and delayed sequential cataract surgery from the payer, patient, and societal perspectives in the United States. JAMA Ophthalmol. 2014;132:1282–8.
Cernat A, Jamieson M, Kavelaars R, Khalili S, Bhambhwani V, Mireskandari K, et al. Immediate versus delayed sequential bilateral cataract surgery in children: a cost-effectiveness analysis. Br J Ophthalmol 2022;106:211–7. https://www.embase.com/search/results?subaction=viewrecord&id=L633488887&from=export.
Neel ST. A cost and policy analysis comparing immediate sequential cataract surgery and delayed sequential cataract surgery from the physician perspective in the United States. JAMA Ophthalmol. 2014;132:1359–62.
UK Health Security Agency. Cost effectiveness analysis: health economic studies. Guidance. 2020. Available at: https://www.gov.uk/guidance/cost-effectiveness-analysis-health-economic-studies. Accessed August 4, 2022.
Quist SW, de Jong LA, van Asten F, Knoester P, Postma MJ, Freriks RD. Cost-minimisation analysis of a treat-and-extend regimen with anti-VEGFs in patients with neovascular age-related macular degeneration. Graefe’s Arch Clin Exp Ophthalmol. 2022;260:1083–95. https://doi.org/10.1007/s00417-021-05359-x.
Ngan K, Fraser E, Buller S, Buller A. A cost minimisation analysis comparing iStent accompanying cataract surgery and selective laser trabeculoplasty versus topical glaucoma medications in a public healthcare setting in New Zealand. Graefe’s Arch Clin Exp Ophthalmol. 2018;256:2181–9. http://link.springer.com/10.1007/s00417-018-4104-8.
Maxwell WA, Waycaster CR, D’Souza AO, Meissner BL, Hileman K. A United States cost–benefit comparison of an apodized, diffractive, presbyopia-correcting, multifocal intraocular lens and a conventional monofocal lens. J Cataract Refract Surg. 2008;34:1855–61. https://pubmed.ncbi.nlm.nih.gov/19006730/.
UK Health Security Agency. Cost utility analysis: health economic studies. Guidance. 2020. Available at: https://www.gov.uk/guidance/cost-utility-analysis-health-economic-studies. Accessed August 4, 2022.
UK Health Security Agency. Cost benefit analysis: health economic studies. Guidance. 2020. Available at: https://www.gov.uk/guidance/cost-benefit-analysis-health-economic-studies. Accessed August 4, 2022.
Webb J, Fife-Schaw C, Ogden J. A randomised control trial and cost-consequence analysis to examine the effects of a print-based intervention supported by internet tools on the physical activity of UK cancer survivors. Public Health. 2019;171:106–15. https://linkinghub.elsevier.com/retrieve/pii/S0033350619301143.
Torrance GW. Utility approach to measuring health-related quality of life. J Chronic Dis. 1987;40:593–600.
Drummond MF. Economic aspects of cataract. Ophthalmology. 1988;95:1147–53. https://pubmed.ncbi.nlm.nih.gov/3148114/.
Brown GC. Vision and quality-of-life. Trans. Am Ophthalmol Soc. 1999;97:473–511.
Lansingh VC. Use of Global Visual Acuity Data in a Time Trade-off Approach to Calculate the Cost Utility of Cataract Surgery. Arch Ophthalmol. 2009;127:1183 https://pubmed.ncbi.nlm.nih.gov/19752429/.
Eye Care Comparative Effectiveness Research Team (ECCERT). Cost-effectiveness of cataract surgery in Japan. Jpn J Ophthalmol. 2011;55:333–42. https://doi.org/10.1007/s10384-011-0041-3.
Tahhan N, Papas E, Fricke T, Frick K, Holden B. Utility and uncorrected refractive error. Investig. Ophthalmol Vis Sci. 2013;54. Available at: https://www.embase.com/search/results?subaction=viewrecord&id=L628731005&from=export.
Kobelt G, Lundström M, Stenevi U. Cost-effectiveness of cataract surgery. J Cataract Refract Surg. 2002;28:1742–9. https://journals.lww.com/02158034-200210000-00021.
Brown GC, Brown MM, Chaudhry I, Stein JD. Opportunities to Reduce Potential Bias in Ophthalmic Cost-Utility Analysis. JAMA Ophthalmol. 2021;139:389 https://pubmed.ncbi.nlm.nih.gov/33538789/.
Weale M. A cost-benefit analysis of cataract surgery based on the English Longitudinal Survey of Ageing. J Health Econ. 2011;30:730–9.
Lugnér AK, Krabbe PFM. An overview of the time trade-off method: concept, foundation, and the evaluation of distorting factors in putting a value on health. Expert Rev Pharmacoeconomics Outcomes Res. 2020;20:331–42. https://doi.org/10.1080/14737167.2020.1779062.
Arnesen TM, Norheim OF. Quantifying quality of life for economic analysis: Time out for time trade off. Med Humanit. 2003;29:81–6.
Leung EH, Gibbons A, Koch DD. Cost-Effectiveness of Preoperative OCT in Cataract Evaluation for Multifocal Intraocular Lens. Ophthalmology. 2020;127:859–65. https://pubmed.ncbi.nlm.nih.gov/32173111/.
Räsänen P, Krootila K, Sintonen H, Leivo T, Koivisto AM, Ryynänen OP, et al. Cost-utility of routine cataract surgery. Health Qual Life Outcomes. 2006;4:74.
Asakawa K, Rolfson D, Senthilselvan A, Feeny D, Johnson JA. Health Utilities Index Mark 3 showed valid in Alzheimer Disease, arthritis, and cataracts. J Clin Epidemiol. 2008;61:733–9.
Schweitzer C, Brezin A, Cochener B, Monnet D, Germain C, Roseng S, et al. Femtosecond laser-assisted versus phacoemulsification cataract surgery (FEMCAT): a multicentre participant-masked randomised superiority and cost-effectiveness trial. Lancet. 2020;395:212–24.
Lin CC, Rose-Nussbaumer JR, Al-Mohtaseb ZN, Pantanelli SM, Steigleman WA, Hatch KM, et al. Femtosecond Laser-Assisted Cataract Surgery. Ophthalmology. 2022;129:946–54. https://pubmed.ncbi.nlm.nih.gov/35570159/.
Day AC, Burr JM, Bennett K, Dore CJ, Bunce C, Hunter R, et al. Femtosecond laser-assisted cataract surgery compared with phacoemulsification cataract surgery: randomized noninferiority trial with 1-year outcomes. J Cataract Refract Surg. 2020;46:1360–7.
Larco P, Larco C, Borroni D, Godin F, Piñero DP, Rocha-de-Lossada C, et al. Efficacy of femtosecond laser for anterior capsulotomy in complex white cataracts. J Fr Ophtalmol. 2023;46:501–9. https://linkinghub.elsevier.com/retrieve/pii/S0181551223000487.
Abell RG, Vote BJ. Cost-Effectiveness of Femtosecond Laser-Assisted Cataract Surgery versus Phacoemulsification Cataract Surgery. Ophthalmology. 2014;121:10–16. https://pubmed.ncbi.nlm.nih.gov/24120324/.
Jongsareejit A, Wiriyaluppa C, Kongsap P, Phumipan S. Cost-effectiveness analysis of manual small incision cataract surgery (MSICS) and phacoemulsification (PE). J Med Assoc Thail. 2012;95:212–20. https://pubmed.ncbi.nlm.nih.gov/22435252/.
Khan A, Amitava A, Rizvi SA, Siddiqui Z, Kumari N, Grover S. Cost-effectiveness analysis should continually assess competing health care options especially in high volume environments like cataract surgery. Indian J Ophthalmol. 2015;63:496. https://www.embase.com/search/results?subaction=viewrecord&id=L615153888&from=export.
Rochmah TN, Wulandari A, Dahlui M, Ernawaty, Wulandari RD. Cost Effectiveness Analysis Using Disability-Adjusted Life Years for Cataract Surgery. Int J Environ Res Public Health. 2020;17:6010. https://pubmed.ncbi.nlm.nih.gov/32824872/.
Wulandari A, Dahlui M, E, Wulandari RD, Rochmah TN. Cost effectiveness analysis between small incision cataract surgery and phacoemulsification. J Heal Transl Med. 2020;23:231–7. https://jummec.um.edu.my/index.php/jummec/article/view/25860.
Manaf MRA, Aljunid SM, Annuar FH, Leong CK, Mansor N. Cost-effectiveness analysis of cataract surgery with intraocular lens implantation: Extracapsular cataract extraction versus phacoemulsification. Med J Indones. 2007;16:25–31.
Baltussen R, Sylla M, Mariotti SP. Cost-effectiveness analysis of cataract surgery: a global and regional analysis. Bull World Health Organ. 2004;82:338–45.
Rizal AM, Aljunid SM, Normalina M, Hanom AF, Chuah KL, Suzainah Y, et al. Cost analysis of cataract surgery with intraocular lens implantation: a single blind randomised clinical trial comparing extracapsular cataract extraction and phacoemulsification. Med J Malays. 2003;58:380–6. https://pubmed.ncbi.nlm.nih.gov/14750378/.
Asimakis P, Coster DJ, Lewis DJ. Cost effectiveness of cataract surgery. A comparison of conventional extracapsular surgery and phacoemulsification at Flinders Medical Centre. Aust N Z J Ophthalmol. 1996;24:319–25.
Kristianslund O, Dalby M, Moe MC, Drolsum L. Cost‐effectiveness analysis in a randomized trial of late in‐the‐bag intraocular lens dislocation surgery: repositioning versus exchange. Acta Ophthalmol. 2019;97:771–7. https://www.embase.com/search/results?subaction=viewrecord&id=L627183345&from=export.
Malvankar-Mehta MS, Filek R, Iqbal M, Shakir A, Mao A, Si F, et al. Immediately sequential bilateral cataract surgery: a cost-effective procedure. Can J Ophthalmol 2013;48:482–8. https://pubmed.ncbi.nlm.nih.gov/24314408/.
Lundström M, Albrecht S, Roos P. Immediate versus delayed sequential bilateral cataract surgery: an analysis of costs and patient value. Acta Ophthalmol. 2009;87:33–8.
Sach TH, Foss AJE, Gregson RM, Zaman A, Osborn F, Masud T, et al. Second-eye cataract surgery in elderly women: a cost-utility analysis conducted alongside a randomized controlled trial. Eye. 2010;24:276–83. https://pubmed.ncbi.nlm.nih.gov/19444295/.
Busbee BG, Brown MM, Brown GC, Sharma S. Cost-utility analysis of cataract surgery in the second eye. Ophthalmology. 2003;110:2310–7. https://pubmed.ncbi.nlm.nih.gov/14644712/.
Boyd M, Kvizhinadze G, Kho A, Wilson G, Wilson N. Cataract surgery for falls prevention and improving vision: modelling the health gain, health system costs and cost-effectiveness in a high-income country. Inj Prev. 2020;26:302–9. https://www.embase.com/search/results?subaction=viewrecord&id=L628439610&from=export.
Boyd M, Kho A, Wilson G, Wilson N. Expediting cataract surgery in New Zealand is cost-effective for falls prevention and improving vision-so what might be the next steps? N Z Med J. 2019;132:73–8. https://www.embase.com/search/results?subaction=viewrecord&id=L629200987&from=export.
Frampton G, Harris P, Cooper K, Lotery A, Shepherd J, GF, et al. The clinical effectiveness and cost-effectiveness of second-eye cataract surgery: a systematic review and economic evaluation. Health Technol Assess. 2014;18:1–206. https://www.journalslibrary.nihr.ac.uk/hta/hta18680/.
Meltzer ME, Congdon N, Kymes SM, Yan X, Lansingh VC, Sisay A, et al. Cost and Expected Visual Effect of Interventions to Improve Follow-up After Cataract Surgery. JAMA Ophthalmol. 2017;135:85 https://pubmed.ncbi.nlm.nih.gov/27978578/.
Jastrzebski A, Villafranca A, Sethi S, Bellan L. Safety and comparative costs of preoperative assessments for cataract surgery: traditional mandatory assessment versus a novel graded assessment system. Can J Anesth. 2016;63:842–50.
Naeim A, Keeler EB, Gutierrez PR, Wilson MR, Reuben D, Mangione CM. Is cataract surgery cost-effective among older patients with a low predicted probability for improvement in reported visual functioning? Med Care. 2006;44:982–9.
Dimock J, Robman LD, McCarty CA, Taylor HR. Cost-effectiveness of digital cataract assessment. Aust N Z J Ophthalmol. 1999;27:208–10. https://doi.org/10.1046/j.1440-1606.1999.00207.x.
Hopkins RB, Tarride J-E, Bowen J, Blackhouse G, O’Reilly D, Campbell K, et al. Cost-effectiveness of reducing wait times for cataract surgery in Ontario. Can J Ophthalmol. 2008;43:213–7. https://pubmed.ncbi.nlm.nih.gov/18347625/.
Jain S, Chauhan A, Rajshekar K, Vashist P, Gupta P, Mathur U, et al. Generic and vision related quality of life associated with different types of cataract surgeries and different types of intraocular lens implantation. PLoS One. 2020;15:e0240036.
Smith AF, Lafuma A, Berdeaux G, Berto P, Brueggenjuergen B, Magaz S, et al. Cost-effectiveness analysis of PMMA, silicone, or acrylic intra-ocular lenses in cataract surgery in four European countries. Ophthalmic Epidemiol. 2005;12:343–51. https://pubmed.ncbi.nlm.nih.gov/16272054/.
Colin J, Praud D, Touboul D, Schweitzer C. Incidence of glistenings with the latest generation of yellow-tinted hydrophobic acrylic intraocular lenses. J Cataract Refract Surg. 2012;38:1140–6. https://doi.org/10.1016/j.jcrs.2012.01.031.
Simons RWP, Visser N. van den Biggelaar FJHM, Nuijts RMMA, Webers CAB, Bauer NJC, et al. Trial-based cost-effectiveness analysis of toric versus monofocal intraocular lenses in cataract patients with bilateral corneal astigmatism in the Netherlands. J Cataract Refract Surg. 2019;45:146–52.
Orme ME, Paine AC, Teale CW, Kennedy LM. Cost-effectiveness of the AMOArray Multifocal Intraocular Lens in Cataract Surgery. J Refract Surg. 2002;18:162–8. https://pubmed.ncbi.nlm.nih.gov/30471848/.
Hu JQ, Sarkar R, Murphy J, Afshari NA. Cost-effectiveness of multifocal intraocular lenses compared to monofocal intraocular lenses in cataract surgery. Investig Ophthalmol Vis Sci. 2018;59. https://www.embase.com/search/results?subaction=viewrecord&id=L628536790&from=export.
Athanasiov P, Bala C, Holland J, Dhariwal M, Gupta A, Rathi H. A cost-effectiveness analysis of AcrySof IQ vivity intraocular lens from private health fund perspective in Australia. Clin Ophthalmol. 2022;49:878–9.
Dobrez DG, Calhoun EA. Testing subject comprehension of utility questionnaires. Qual Life Res. 2004;13:369–76.
Lin J-C, Yang M-C. Cost-Effectiveness Comparison Between Monofocal and Multifocal Intraocular Lens Implantation for Cataract Patients in Taiwan. Clin Ther. 2014;36:1422–30. https://pubmed.ncbi.nlm.nih.gov/25146366/.
De Vries NE, Laurendeau C, Lafuma A, Berdeaux G, Nuijts RMMA. Lifetime costs and effectiveness of ReSTOR compared with a monofocal IOL and Array-SA40 in the Netherlands. Eye. 2010;24:663–72. https://pubmed.ncbi.nlm.nih.gov/19575029/.
Lafuma A, Berdeaux G. Modelling lifetime cost consequences of ReSTOR in cataract surgery in four European countries. BMC Ophthalmol. 2008;8:12.
Simons RWP, Wielders LHP, Nuijts RMMA, Veldhuizen CA, van den Biggelaar FJHM, Winkens B, et al. Economic evaluation of prevention of cystoid macular edema after cataract surgery in diabetic patients: ESCRS PREMED study report 6. J Cataract Refract Surg. 2022;48:555–63. https://pubmed.ncbi.nlm.nih.gov/33009281/.
Author information
Authors and Affiliations
Contributions
Concept and design: Ginel, Burguera, Fernández; Acquisition of data: Ginel, Burguera; Analysis and interpretation of data: Ginel, Burguera, Piñero, Sáez-Martín, Haro De Rosario, Fernández; Drafting of the manuscript: Ginel, Burguera, Fernández; Critical revision of the paper for important intellectual content: Piñero, Sáez-Martín, Haro De Rosario; Obtaining funding: Fernández; Administrative, technical, or logistic support: Fernández; Supervision: Piñero, Sáez-Martín, Haro De Rosario, Fernández.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ginel, J., Burguera, N., Piñero, D. et al. Economic evaluations in cataract surgery: a narrative review. Eye 38, 1418–1424 (2024). https://doi.org/10.1038/s41433-024-02965-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-024-02965-x
- Springer Nature Limited