Abstract
Background
The prevalence and clinical relevance of incidental findings (IF(s)) on imaging assessing the pelvis in children has not been well documented.
Methods
Three-thousand two-hundred thirty-one children (mean age 10.2 (range 8.6–12.9) years) were evaluated with MRI of the hips, pelvis, and lumbar spine, as part of a prospective population-based pediatric cohort study. Scans were reviewed by trained medical staff for abnormalities. IFs were categorized by clinical relevance and need for further clinical evaluation.
Results
8.3% (n = 267) of children featured at least one IF. One or more musculoskeletal IFs were found in 7.9% (n = 254) of children, however, only 0.8% (n = 2) of musculoskeletal IFs required clinical evaluation. Most frequent abnormalities were simple bone cysts 6.0% (n = 195), chondroid lesions 0.6% (n = 20), and perineural cysts 0.5% (n = 15). Intra-abdominal IFs were detected in 0.5% (n = 17) of children, with over half (n = 9) of these requiring evaluation. The three most common intra-abdominal IFs were a duplex collecting system 0.09% (n = 3), significant ascites 0.06% (n = 2), and hydroureteronephrosis 0.06% (n = 2).
Conclusions
IFs on MRI of the lower abdominal and hip region are relatively common in children aged 8–13 years, most of these can be confidently categorized as clinically irrelevant without the need for additional clinical or radiologic follow up.
Impact
-
Our research contributes greatly to the knowledge of the prevalence of (asymptomatic) pathology in children. We evaluated MR images of 3231 children, covering hip joints, pelvic skeleton, lower and mid-abdomen, and lumbar and lower thoracic spine as part of a population study.
-
One or more musculoskeletal incidental finding were found in 7.9% of children. Most of these can be confidently categorized as clinically irrelevant without the need for additional follow up. However 0.8% of musculoskeletal findings required further evaluation.
-
Intra-abdominal incidental findings were detected in 0.5% of children, with over half of the abdominal and urogenital findings requiring further evaluation.
Similar content being viewed by others
Introduction
With the advances in magnetic resonance imaging (MRI) techniques, an increasing number of research studies are performed in which MRI is used to assess normal development, disease outcome, or the natural history of disease. As no ionizing radiation is involved, MRI is increasingly used in pediatric research. In keeping with this increased utilization of MRI for research purposes, an increasing amount of incidental finding(s) (IF(s)) are being detected, especially on MR images that cover a large area of the body. IFs are defined as previously unknown imaging abnormalities that are unrelated to the purpose of the study.1,2,3,4
Adequate management of IFs is especially relevant for population-based research that includes body MRI5,6 in which children are typically assumed to not be afflicted by any known health condition and therefore are unlikely to be undergoing alternative health monitoring. Depending on the type of IF, it could be potentially clinically relevant, prompting the need for systematic screening of IFs, as well as a protocol for reporting clinically relevant IFs to pediatric research participants and/or their parents for further evaluation. Previous studies involving MRI have focused mainly on IFs in the brain of healthy pediatric7,8 or adult populations,9 with limited research data on IFs found in body imaging of healthy adult subjects.10,11 In children, IFs in body MRI have only been reported in pediatric patients on scans acquired for unrelated pathology.12,13,14 To our knowledge, the prevalence of clinically relevant musculoskeletal and soft-tissue IFs on MR images that cover the hip joints, pelvic skeleton, lower and mid-abdomen, and lumbar and lower thoracic spine in the general pediatric population has yet to be assessed. Given their young age, IFs can have profound lifelong implications. However, for some of these IFs the natural course, and hence their clinical significance, are (partially) unknown. Consequently, it is imperative that the prevalence of any IFs, and the management thereof, is well established.
The aim of this study was to determine the prevalence of IFs on MRI scans with coverage of the hip joints, pelvic skeleton, lower and mid-abdomen and lumbar, and lower thoracic spine in the general pediatric population.
Methods
Study population and design
The source population originates from the Generation R Study, a prospective population-based cohort study in Rotterdam, the Netherlands, following children from fetal life until early adulthood. Nine-thousand seven-hundred seventy-eight mothers with expected delivery dates between April 2002 and January 2006 were included initially. The objectives of the Generation R study are to identify relationships between environmental and genetic factors and their contribution to normal and abnormal growth and development.15,16,17
At approximately 9 years of age 5862 children without contraindications to MRI were invited to undergo MRI. Between March 2013 and November 2016, a subgroup consisting of 3231 children participated in MR imaging to study the development of the hip joints and lower spine and the associations between bone shape, physical activity and bone health. These MRI scans covered the hip joints, pelvic skeleton, lower and mid-abdomen and lumbar and lower thoracic spine. Prior studies did not include analysis of these MRI scans. The Erasmus University Medical Center review board approved of the study and parents or legal guardians of the children provided written informed consent. In accordance with Dutch Law, children aged 12 years and older provided written informed consent themselves as well.15
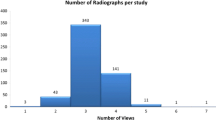
MRI acquisition
All MR images were obtained on the same 3.0 Tesla MRI scanner (Discovery MR750, GE Healthcare, Milwaukee, WI). Children were scanned in supine position with a Geometry Embracing Method (GEM) posterior array embedded in the table and a small 16 channel body anterior array. The scan protocol consisted of two high-resolution three-dimensional (3D) sequences acquired in the coronal plane; a 3D T2–weighted fat-suppressed sequence (FS Cube); and a 3D T1–weighted 2-point DIXON gradient echo scan sequence (LAVA-Flex), producing four volumetric imaging datasets: water only, fat only, in-phase, and out-of-phase. The T2 FS Cube images were acquired with a 40 cm field of view (FOV) and a reconstructed voxel size of 0.8 × 0.8 × 1.2 mm3. The LAVA-Flex images were acquired with a 46 cm FOV and a reconstructed voxel size of 0.9 × 0.9 × 1.2 mm3. All slices were contiguous and a 3D gradient inhomogeneity (gradwarp) correction was applied to account for geometrical distortions. Multiplanar reconstructions were available to accurately study the shape and dimensions of IFs. The total scan time of these two sequences was 4:46 min. Examinations were obtained in a standardized way by trained research technologists.
Protocol assessment of incidental findings
IFs were evaluated using AquariusNET software (TeraRecon Gmb, Frankfurt am Main, Germany). All scans were evaluated for IFs in the hip joints, pelvic skeleton, lower and mid-abdomen and lumbar, and lower thoracic spine along with the surrounding soft tissues, including the abdominal organs in this region by trained medical staff consisting of seven radiology residents, two radiology doctorate students and a medical student. The medical staff evaluating these scans did not have any clinical information on the children. All detected findings were confirmed by a radiologist. Management of IFs was predefined in a protocol developed in consensus between specialist radiologists (musculoskeletal and pediatric) and a pediatric orthopedic surgeon. Table 1 shows the list of expected IFs that were defined in our protocol. This list was used to categorize IFs into those that required further clinical evaluation and those that were considered unlikely to be clinically relevant. We considered intra-abdominal IFs other than those listed as relatively uncommon and potentially diverse, such that extending the protocol to cover all possible findings would make it unclear and unnecessarily complicated. All findings that were not covered by the predefined list were discussed individually by a panel consisting of a musculoskeletal radiologist, a pediatric radiologist and a pediatric orthopedic surgeon; furthermore when needed a pediatric (sub)specialist was consulted. Accurate diagnosis of undescended testes based on MRI is unreliable without a proper physical exam,18 therefore this potential finding was not included in the results.
Each detected IF that was considered clinically relevant (Table 1), was discussed with a pediatric orthopedic surgeon or other clinical pediatric specialist, as applicable, in order to confirm clinical relevance and to initiate further clinical evaluation. Parents were contacted and/or medical information submitted by children was checked to verify that the detected findings were indeed previously unknown and therefore incidental.
Children with IFs requiring follow-up evaluation or treatment were informed and referred to their family physician with recommendations. The family physician directly referred these patients to a specialist, (with the exception of undescended testes, which were evaluated by the family physician who first performed physical examination) who decided whether further radiological or specialized work-up was required.
Analysis
The prevalence of each IF in the study population was determined on a per-subject basis. Therefore, multiple identical diagnoses of IFs in the same participant (e.g. more than one simple bone cyst) were counted once to determine prevalence.
Results
This study consisted of 3231 children (1632 female, 50.5%) with a mean age of 10 years and 2 months (range 8.6 to 12.9 years). Owing to time restrictions not all children underwent both MRI sequences; a total of 3147 LAVA-Flex scans and 3224 T2 FS Cube scans were collected.
Prevalence of incidental findings
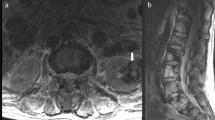
The predefined protocol for the assessment of IFs covered most musculoskeletal IFs that were encountered, allowing for an efficient categorization of clinical relevance of the IF. A total of 271 different types of abnormalities were found in 8.3% (n = 267) of children. 1.0% (n = 32) of children had two or more IFs, including four children with two different types of abnormalities. Table 2 shows the prevalence of each recorded IF. The majority of these findings were categorized as musculoskeletal, found in 7.9% (n = 254) of children. The most common musculoskeletal finding was simple bone cysts found in 6.0% (n = 195, Fig. 1a, b) of children. A total of 225 bone cysts were found, including 18 children with two bone cysts and 6 children with three bone cysts. The bone cysts were located in the iliac bone 54.2% (n = 122), sacrum 32.0% (n = 72), acetabulum 7.6% (n = 17), coccyx 2.7% (n = 6), femur 2.2% (n = 5), ischium 0.4% (n = 1), pubic bone 0.4% (n = 1) and spine 0.4% (n = 1), with sizes varying from ≤ 5 mm in 156 subjects (69.3%), 6–10 mm in 61 subjects (27.1%), 11–15 mm in 4 subjects (1.8%), 16–20 mm in 3 subjects (1.3%), and > 20 mm in 1 subject (0.4%). The second and third most common musculoskeletal findings were chondroid lesions 0.6% (n = 20, Fig. 1c) and perineural (Tarlov) cysts 0.5% (n = 15). There was a relatively equal distribution between sexes for the three most common musculoskeletal diagnoses; 52.3% (n = 102) of children with simple bone cysts, 60.0% (n = 12) of children with chondroid lesions and 53.3% (n = 8) of subjects with perineural (Tarlov) cysts were girls. The three most common intra-abdominal IFs were a duplex collecting system 0.09% (n = 3), a significant amount of ascites 0.06% (n = 2), and hydroureteronephrosis 0.06% (n = 2).
Clinical evaluation and follow up treatment
Further clinical evaluation was only required in 0.8% (n = 2) of musculoskeletal IFs. In contrast, intra-abdominal IFs were detected in only 0.5% (n = 17) of children (Table 2), over half of which required clinical evaluation (Table 3). Overall, 0.3% (n = 11) children had findings that required referral for further clinical evaluation. Table 3 shows the prevalence of IFs requiring further clinical evaluation or radiological follow up. A child with a large simple bone cyst (> 20 mm, Fig. 1b) in the femur was referred to a pediatric orthopedic surgeon. The bone cyst was re-evaluated with MRI after 3 years, which showed that the lesion had not changed. The child was advised to return to an orthopedic surgeon only if the child developed complaints of the hip. A child with a large soft-tissue lesion (> 20 mm) in the vastus lateralis muscle was referred to a pediatric orthopedic surgeon and re-evaluated by ultrasound 3 years later, in which the lesion had decreased in size and become more inhomogeneous. The soft-tissue lesion was assumed to be post traumatic, as the child regularly practiced sports, and an expectative management approach was implemented. One male subject with significant amount of ascites was referred to his family physician with the recommendation for evaluation by ultrasound to exclude underlying pathology. A child with a congenital solitary kidney was referred to a pediatric nephrologist. After further examination the final diagnosis was uncomplicated solitary kidney and the patient was referred back to the family physician and advised to have blood pressure evaluations every other year. Three children with a duplex collecting system (Fig. 2a) and two children with hydroureteronephrosis (Fig. 2b) were referred to the family physician with the recommendation for evaluation by ultrasound. A boy with hydrocele testis was referred to the family physician for physical evaluation. One child was diagnosed with a teratoma likely originating from their left ovary (Fig. 3), and was referred to a gynecologist for monitoring. The child developed lower abdominal pain after 4 years and re-evaluation with MRI showed small growth of the teratoma, leading to its removal via laparoscopic surgery.
Discussion
Based on this large pediatric population imaging study, we found that the prevalence of IFs on MRI covering the hips, pelvic skeleton, lower and mid-abdomen and lumbar and lower spine is common in 8-13 year-old children, though only few warrant further clinical evaluation. Musculoskeletal IFs are usually innocuous, whereas over half of soft tissue/abdominal findings demand further clinical work-up. We believe that this study greatly contributes to knowledge on the prevalence of IFs in children.
The prevalence of musculoskeletal IFs was 7.9%, which is higher than the reported 6.0% based on whole-body MRI research conducted on the general population.11 This higher prevalence could be explained by the large number of simple bone cysts found in children, which could indicate that these bone cysts resolve over time. This has also been suggested by previous research, in which simple bone cysts were found in only 2.0% of adults.10
Intra-abdominal IFs were detected in 0.5% of children. In the general adult population IFs in the abdominal organs (6.8%) and urinary tract (6.8%) have been reported to be more prevalent.11 This study was, however, based on whole-body imaging which explains, along with greater age, the higher number of intra-abdominal findings, a substantial number of which consisted of (presumed) malignancies and degenerative disorders, including prostatic hyperplasia.11 Our young population explains the absence of incidentally discovered degenerative diseases and malignancies, which occur more frequently with increasing age.19 In a clinical population of children who underwent whole-body MRI, IFs in the abdominal organs and the genitourinary tract were present in 1.7% and 6.8% of children, respectively.12 This is a relatively high number compared to our findings but could be explained by the fact that this study was conducted in a clinical setting with pediatric patients who were evaluated for unrelated pathologies, and who could have a higher predisposition for IFs compared to the community dwelling children included in our analysis. Moreover this whole-body MRI study also covered all upper abdominal organs, contrary to our study that only covered the mid and lower abdomen.
Given the low frequency of clinically relevant IFs, it could be questioned from both a medical and financial perspective, whether the effort of systematic screening of research MR images for IFs is warranted. However, from a psychological viewpoint, participants (children and their parents) have a strong opinion about the need to evaluate their MR images and research shows that they expect this to be performed regardless of whether this is mentioned in informed consent documents.20,21 Consequently, a decision not to screen for IFs could have a potential negative impact on participants willingness to participate in research studies. Furthermore, given the young age of the children in a pediatric population study like ours, clinically relevant findings could have potential lifelong consequences if they are not detected in their early stages. Conversely, one also needs to consider the emotional impact of disclosing IFs and the subsequent follow-up.20 For many IFs it is currently not possible to state that earlier diagnosis precipitated by research would result in a better long-term clinical outcome. However, from a research ethical perspective, we considered it prudent to disclose the IFs in this study.
The large sample size is a major strength of this population study. All subjects were scanned according to the same MRI protocol and reviewers were unaware of children’s medical history, making detection bias unlikely.
There are several limitations to this study. Firstly, scans were initially evaluated by trained medical staff instead of a radiologist. However, all IFs were verified by a radiologist. The radiologist reviewing scans did not detect any additional abnormalities compared to those detected initially, indicating that our initial screening procedure had high accuracy. Secondly, due to the short acquisition time of these research MR images, available pulse sequences were limited, without contrast administration, and image quality was relatively low compared to clinical MRI protocols, potentially leading to underreporting of abnormalities. Thirdly, available literature on the prevalence and natural course of musculoskeletal abnormalities, such as bone cysts in children, is scarce. Consequently, our protocol to manage IFs was based on expert opinions. A major benefit of this study being embedded in a longitudinal population cohort is the possibility of studying the natural course of IFs, due to the repetition of MRI at later ages.
Lastly, the inclusion criteria of the Generation R study, in which selection bias towards a more healthy and Western population might have occurred,15 might have potentially influenced the prevalence of IFs.
In conclusion, IFs in the hip joints, pelvic skeleton, lower and mid-abdomen, and lower spine on research MRI are relatively common in children aged 8–13 years. However, most IFs are clinically irrelevant, not meriting additional clinical or radiological follow up. While musculoskeletal IFs requiring further evaluation are very uncommon, intra-abdominal IFs are also very rare, but require clinical evaluation in the majority of cases.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Sullivan, J. W. O., Muntinga, T., Grigg, S. & Ioannidis, J. P. A. Prevalence and outcomes of incidental imaging findings: umbrella review. BMJ 361, k2387 (2018).
Hitzeman, N. & Cotton, E. Incidentalomas: Initial Management. Am. Fam. Physician 90, 784–789 (2014).
Bunnik, E. M. & Vernooij, M. W. Incidental findings in population imaging revisited. Eur. J. Epidemiol. 31, 1–4 (2016).
Illes, J. et al. Incidental findings in brain imaging research. Science (80-) 311, 783–784 (2006).
Ikram, M. A. et al. The Rotterdam Scan Study: design update 2016 and main findings. Eur. J. Epidemiol. 30, 1299–1315 (2015).
Jaddoe, V. W. V. et al. The generation R study: Design and cohort update 2012. Eur. J. Epidemiol. 27, 739–756 (2012).
Jansen, P. et al. Incidental findings on brain imaging in the general pediatric population. N. Engl. J. Med. 377, 1593–1595 (2017).
Kim, B. S., Illes, J., Kaplan, R. T., Reiss, A. & Atlas, S. W. Incidental findings on pediatric MR images of the brain. Am. J. Neuroradiol. 23, 1674–1677 (2002).
Morris, Z. et al. Incidental findings on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ 339, b3016 (2009).
Morin, S. H. X. et al. Incidental findings in healthy control research subjects using whole-body MRI. Eur. J. Radio. 72, 529–533 (2009).
Hegenscheid, K. et al. Potentially relevant incidental findings on research whole-body MRI in the general adult population: frequencies and management. Eur. Radio. 23, 816–826 (2013).
du Preez, H., Lasker, I., Rajakulasingam, R. & Saifuddin, A. Whole-body magnetic resonance imaging: Incidental findings in paediatric and adult populations. Eur. J. Radio. 130, 109156 (2020).
Ramadorai, U., Devine, J. G., Brodt, E. D. & Dettori, J. R. Incidental findings on magnetic resonance imaging of the spine in the asymptomatic pediatric population: a systematic review. Evid. Based Spine Care J. 5, 95–100 (2014).
Urrutia, J., Zamora, T. & Prada, C. The prevalence of degenerative or incidental findings in the lumbar spine of pediatric patients: a study using magnetic resonance imaging as a screening tool. Eur. Spine J. 25, 596–601 (2016).
Kooijman, M. N. et al. The generation R study: design and cohort update 2017. Eur. J. Epidemiol. 31, 1234–1264. (2016).
Jaddoe, V. W. V. et al. The generation R study: design and cohort update until the age of 4 years. Eur. J. Epidemiol. 23, 801–811 (2008).
Hofman, A. et al. Growth, development and health from early fetal life until young adulthood: the generation R study. Paediatr. Perinat. Epidemiol. 18, 61–72 (2004).
Jenkins, J. T. & O’Dwyer, P. J. Inguinal hernias. BMJ 336, 269–272 (2008).
Cieszanowski, A., Maj, E., Kulisiewicz, P., Grudzinski, I. P. & Jakoniuk-Glodala, K. Non-contrast-enhanced whole-body magnetic resonance imaging in the general population: the incidence of abnormal findings in patients 50 years old and younger compared to older subjects. PLoS ONE 9, e107840 (2014).
Boer AW, D. E. et al. Incidental findings in research: a focus group study about the perspective of the research participant. J. Magn. Reson. Imaging 47, 230–237 (2018).
Kirschen, M., Jaworska, A. & Illes, J. Subjects’ expectations in neuroimaging research. J. Magn. Reson. imaging 23, 205–209 (2006).
Funding
No financial assistance was received in support of the study.
Author information
Authors and Affiliations
Contributions
D.K.d.V., J.H.J.M.B., M.H.G.D., A.v.d.L., E.H.G.O.: substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; drafting the article or revising it critically for important intellectual content; and final approval of the version to be published. M.W.V.: drafting the article or revising it critically for important intellectual content; and final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The Erasmus University Medical Center review board approved of the study and parents or legal guardians of the children provided written informed consent. In accordance with Dutch Law, children aged 12 years and older provided written informed consent themselves as well.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
de Vreede, D.K., Bessems, J.H.J.M., Dremmen, M.H.G. et al. The prevalence of incidental findings on pelvis MRI of 8–13-year-old children. Pediatr Res 93, 2045–2050 (2023). https://doi.org/10.1038/s41390-022-02259-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02259-6
- Springer Nature America, Inc.