Abstract
Background
Although risperidone is increasingly used for behavioral indications in children, the associated adverse events (AEs) are not well defined in this population.
Objective
We determined the incidence of and risk factors for AEs among children treated with risperidone at our institution, an academic medical center with inpatient, outpatient, generalist, and specialist pediatric care.
Methods
The study included children aged ≤ 18 years with ≥ 4 weeks of risperidone exposure. Data were obtained using de-identified electronic health records. AEs were defined as any untoward event attributed to risperidone reported by the patient, parent/guardian, or physician or detected following a laboratory investigation. Associations between AEs and clinical variables were determined using univariate and multivariate analyses.
Results
The study cohort included 371 individuals (median age 7.8 years [interquartile range 5.9–10.2]; 271 [73.0%] male). The two most common primary diagnoses were attention-deficit/hyperactivity disorder (160 [43.1%]) and autism (102 [27.5%]). The most frequent indications for risperidone were aggression (166 [44.7%]) and behavioral problems (114 [30.7%]). Altogether, 110 (29.6%) individuals had 156 AEs. Weight gain (32 [20.5%]) and extrapyramidal symptoms (23 [14.7%]) were the most common AEs. Aggression, irritability, and self-injurious behavior were positively associated with AEs, and concomitant analgesics and antibiotics were negatively associated. In multivariate analysis, associations remained significant for self-injurious behavior (adjusted odds ratio [aOR] 3.1; 95% confidence interval [CI] 1.7–5.4) and concomitant antibiotics (aOR 0.2; 95% CI 0.1–0.9).
Conclusions
Nearly one in three children treated with risperidone for ≥ 1 month experienced one or more AEs. Particular vigilance is warranted for children with self-injurious behavior.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Use of risperidone in children is common, especially among children with developmental and behavioral problems such as autism and attention-deficit/hyperactivity disorder. |
Nearly one in three pediatric patients treated with risperidone experienced one or more adverse event. Weight gain and extrapyramidal symptoms were the most common adverse events. |
The pre-exposure presence of self-injurious behavior was associated with higher odds of adverse events, whereas concomitant use of antibiotics was associated with lower odds of adverse events. |
1 Introduction
Despite relatively narrow US FDA-approved indications in children and adolescents, antipsychotic drugs are important in the treatment of several pediatric conditions, and prescription rates for young people are on the rise [1,2,3,4]. Risperidone, a serotonin-dopamine antagonist, is FDA approved for use in children aged 5–16 years to treat irritability associated with autism, in children aged 10–17 years to treat mania and mixed state due to bipolar disorder, and in children aged 13–17 years to treat schizophrenia [3]. Risperidone is also increasingly used “off-label” for conditions including developmental and disruptive disorders, depression, obsessive-compulsive disorder (OCD), post-traumatic stress disorder, personality disorder, attention-deficit/hyperactivity disorder (ADHD), and Tourette syndrome [4, 5].
Clinically important adverse events (AEs) attributed to risperidone include weight gain, prolonged QTc, tardive and withdrawal dyskinesia, diabetes mellitus, and hyperlipidemia, all of which have been well-documented in adults [6,7,8]. The reported incidence of AEs with risperidone, based on limited studies in adults, ranges from 1 in 16 patients to 68 in 100 patients, depending on the population studied and the definition of AEs [9, 10]. According to the American Academy of Child and Adolescent Psychiatry, AEs with atypical antipsychotics in children are similar to those seen in adults [4], but there are concerns that the consequences of risperidone-related AEs may be more serious in children than in adults [6].
There are very limited data documenting the AE profile of risperidone in young patients. Studies published to date have been of small patient cohorts representing specific subgroups of pediatric patients and have focused on the most common AEs such as weight gain and enuresis [7, 10,11,12,13,14,15,16]. Further, the studies were limited to ≤ 8 weeks and were unable to capture the AEs associated with prolonged use of risperidone. There are reports of additional AEs with prolonged use of risperidone, including iron deficiency anemia, pituitary tumors, hyperprolactinemia, low bone mineral density, arterial hypertension, and posterior reversible cerebral edema syndrome [17,18,19,20].
Due to developmental changes in the expression of drug targets, transporters, ion channels, receptors, and downstream signal transduction pathways, AE profiles may differ across age groups [21]. Further, children and adolescents may also be at a greater risk for rare AEs than adults. Because fewer children than adults are treated with most atypical antipsychotic medicines, the data available from passive reporting databases such as the FDA Adverse Event Reporting System (FAERS) are limited, and available information on rare AEs of risperidone may be insufficient to guide rational prescribing for children and adolescents.
In this study, we sought to determine the incidence of and risk factors for AEs among children treated with risperidone at our institution. We used a de-identified electronic health record (EHR)-based data repository to study AEs among 371 children and adolescents exposed to risperidone for at least 4 weeks and, in doing so, also enabled an analysis of risperidone use patterns at this tertiary care children’s hospital.
2 Methods
2.1 Study Design
The study was performed using the Synthetic Derivative (SD), a de-identified EHR data repository from > 2.8 million individuals from Vanderbilt University Medical Center (VUMC) [22, 23]. VUMC is an academic medical center that provides both primary and subspecialty care for pediatric patients in inpatient and outpatient settings. The study was reviewed by the Vanderbilt Institutional Review Board and determined to be non-human subjects research. Inclusion criteria included inpatient or outpatient treatment with risperidone for ≥ 4 weeks and age ≤ 18 years at first dose of risperidone. Exclusion criteria were treatment with risperidone outside of the VUMC system (e.g., patients seen by a pediatric subspecialist but not the risperidone prescriber), insufficient follow-up, or missing data.
2.2 Case Definition and Identification
The primary outcome of interest (AEs) was defined as any untoward event reported by the patient or their parent/guardian, observed by a physician, or detected following a laboratory investigation that was documented in the EHR and attributed to risperidone. As a retrospective study, no causality assessment was performed to establish the relationship between the AEs and risperidone. The EHR of each individual in the cohort was manually reviewed to ensure no AEs were omitted, including all records from the time of risperidone initiation through risperidone discontinuation, loss to follow-up, or the current date.
2.3 Data Extraction
Study data were collected and managed using REDCap electronic data capture tools hosted at Vanderbilt University [24]. Data were extracted on the demographic and clinical details of the patient (including sex, race/ethnicity per administrative data in the EHR, psychiatric/behavioral diagnoses, and comorbidities), medications (including dose amount, route, frequency, duration, and indications), and AEs through manual extraction and use of MedEx data [25]. The first mention of risperidone in the case note or medication administration record was defined as the time risperidone was first commenced. In addition, we noted whether the starting dose of risperidone was modified (increased, decreased, or discontinued) during the course of treatment. In cases with AEs, the type, time of onset, total daily dose of risperidone at the time of the AE, action taken by the physician, and any new antipsychotic orders or prescriptions were documented.
2.4 Statistical Analysis
Demographic, clinical, and dosing data were described as frequencies and percentages for categorical variables or median and interquartile range (IQR) for continuous variables, unless otherwise specified. Comparisons of individuals with and without AE were made using Pearson’s Chi-squared, Fisher’s exact test, or the Mann–Whitney U test, as appropriate. Multivariate logistic regression was performed with AEs as the primary outcome and the following covariates: presence of comorbid conditions, age at which risperidone was commenced, risperidone starting dose and frequency of dosing, dose increase of risperidone, three major indications (aggression, irritability, and self-injurious behavior), and concomitant use of analgesics, antibiotics, and orexigenic (appetite stimulating) medicines. Post hoc analyses of risperidone dosing at the time of the AEs of daytime hypersomnia and extrapyramidal symptoms were performed. Data were analyzed using SPSS statistics software, version 21.0 (IBM Corp; Armonk, NY, USA). All p values < 0.05 were considered statistically significant, and all statistical tests were two-tailed.
3 Results
3.1 Study Cohort
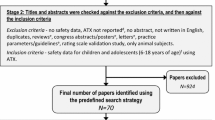
Of 520 individuals initially identified in a search for risperidone-exposed young people, 371 (71.3%) met the inclusion criteria (Fig. 1). The subjects were predominantly males (271 [73.0%]), White (308 [83.0%]), and non-Hispanic (356 [96.0%]) (Table 1). The median age when risperidone was commenced was 7.8 (IQR 5.9–10.2) years (Table 1). Figure 2a shows the primary psychiatric or medical diagnoses for the patients; the two most common were ADHD (160 [43.1%]) and autism (102 [27.5%]). The most common indications for risperidone were aggression (166 [44.7%]) and behavioral problems (114 [30.7%]) (Fig. 2b). In all, 137 (36.9%) patients had at least one of the 81 identified comorbidities; seizure disorder (58 [42.3%]) and asthma (34 [24.8%]) were the most common (Fig. 2c). Most of the prescriptions for risperidone were off-label (277 [74.7%]).
Clinical conditions and concomitant medications in individuals treated with risperidone. a Psychiatric and non-psychiatric diagnoses in the cohort. The total number of diagnoses (458) was higher than the total number of patients (371), as some patients had multiple diagnoses. b Indications for risperidone. The total number of indications (586) was higher than the total number of patients (371), as some patients had multiple indications for risperidone use. c Comorbid conditions in individuals treated with risperidone; 137 individuals had one or more comorbid conditions. d Classes of medicines used concomitantly with risperidone. The total number of concomitant medications (1251) was higher than the total number of patients with concomitant medications (360), as some patients had multiple concomitant medications. *Chromosomal abnormalities included Angelman syndrome, Prader–Willi syndrome, Russell–Silver syndrome, Klinefelter syndrome, trisomy 12p, trisomy 21, 4q deletion, and 7q22.1 deletion; **other diagnoses with only a single count included borderline personality disorder, mixed bipolar affective disorder (depression, anxiety, and panic attack), psychosis, Apert syndrome, asthma, bacteremia and peritonitis, cardiofaciocutaneous syndrome, cerebral palsy only, cerebral palsy with periventricular leukomalacia, chorea/movement disorder, cystic fibrosis with pancreatic insufficiency, ectrodactyly-ectodermal dysplasia-clefting syndrome, end-stage cardiac disease, focal segmental glomerulosclerosis, glomerulonephritis, Henoch–Schönlein purpura, hypoplastic cerebellum, spastic cerebral palsy, hepatic disease, ischemic stroke, meningitis, nephrotic syndrome, neurodegeneration and seizure disorder, non-ketotic hyperglycemia, non-accidental trauma with subdural hemorrhage, pica, post-viral encephalitis seizure disorder, septic shock and encephalopathy, and viral infection; ***other comorbidities with a single count included abdominal pain, acute respiratory failure, anemia, anxiety, bulimia nervosa, Burkitt’s lymphoma, celiac sprue, cerebral palsy, cholesteatoma, chronic adeno-tonsillitis, chronic bronchiolitis, chronic kidney disease, clostridium difficile disease, Crohn’s disease, diabetes insipidus, elevated liver enzymes, endocrine dysfunction, fatty liver disease, failure to thrive, familial hypercholesterolemia, fructose intolerance, gastritis, glomerulonephritis, Grave’s disease, hemophilia A, Henoch Schonlein purpura, hepatitis, Hunter’s disease, hypoalbuminemia, intestinal lymphoid nodular hyperplasia, immunosuppression, latent tuberculosis, liver cirrhosis, malnutrition, meningitis, neuromyotonia, nocturnal enuresis, pancreatitis, perianal candidiasis, periorbital cellulitis, pulmonary hypertension, recurrent hypoglycemia, ruptured appendicitis, scurvy, sickle cell disease, suicidal ideation, transient hypogammaglobinemia of infancy, and VACTERL syndrome. ^Other drugs included antidiabetics, antidiuretics, antifailure medicine, antifungals, antilipidemic medicine. antisecretory medicine, antispasmodic medicine, antiretroviral medicine, anti-tuberculous medicine, antiviral medicine, clotting promoter, diuretics, dopamine promoter, fish oil, iron supplement, laxatives, synthetic growth hormone, thyroxine, urinary bladder relaxant, vasodilator, and vitamins. NOS not otherwise specified, WAGRO Wilms’ tumor/aniridia/genitourinary anomalies/mental retardation syndrome/obesity
3.2 Risperidone and Concomitant Medications
The median starting dose of risperidone was 0.50 mg/day (IQR 0.37–1.00), given as a single dose (n = 160 [43.1%]) or two to six divided doses (n = 211 [56.9%]) (Table 2). Risperidone starting dose was later increased, decreased, or discontinued for 178 (48.0%) patients over the period of treatment. Poor response was the reason for dose increase (n = 94), whereas AEs (n = 4) and good response (n = 8) were the reasons for dose decrease. The drug was discontinued due to treatment completion for postoperative delirium (n = 1), AEs (n = 34), or failure to respond to treatment (n = 37).
Most individuals (n = 360 [97.0%]) used one or more concomitant medicines with risperidone (Fig. 2d). Antidepressants (n = 145 [40.3%]), α2- agonists (n = 144 [40.0%]), psychostimulants (n = 141 [39.2%]), and anticonvulsants (n = 121 [33.6%]) were the leading classes of concomitant medicines.
3.3 Adverse Events to Risperidone
Altogether, 110 (29.6%) patients had a total of 156 AEs (Fig. 3). Weight gain (n = 32 [20.5%]) and extrapyramidal symptoms (n = 23 [14.7%]) were the most common AEs. The specific AEs experienced by each patient and the actions taken by providers are presented in the table in the Electronic Supplementary Material (ESM).
Adverse events during risperidone therapy in the study cohort. *Extrapyramidal symptoms included akathisia, dystonic movement, tremor, and spastic rigidity; **other adverse events included anxiety, droopy eyes, early menstrual flow, fainting spell, headache, heavy tongue, hot flashes, hyperthermia, multiple bruises, musculoskeletal pain, nervousness, oculogyric crisis, premature adrenarche, restlessness, tachycardia, thirst, worsened behavioral problem, and worsened muscle cramp. DM diabetes mellitus
The demographics, clinical variables, and dosing regimen of risperidone for subjects with and without AEs were compared in a univariate analysis (Table 2). There were significant associations between the AE status of the subjects and their race (p = 0.030), risperidone use to treat aggression (p = 0.030), irritability (p = 0.042) or self-injurious behavior (p < 0.001), dose modification of risperidone (p < 0.001), type of dose modification (p < 0.001), and concomitant use of analgesics (p = 0.003) or antibiotics (p = 0.001). On-label versus off-label use was not associated with incidence of AE.
Covariates for multivariate analysis were selected based on adequate group size (≥ 30), significance in the univariate analysis (dose increase of risperidone, aggression, irritability, self-injurious behavior, concomitant analgesics, concomitant antibiotics), prior studies of risperidone AEs (age, starting dose, frequency of dosing, presence of comorbid conditions), and potential direct influence on AEs (concomitant orexigenic drugs). In the multivariable analysis including these 11 covariates, self-injurious behaviors and antibiotic therapy were significantly associated with increased AEs (Table 3). The odds of AEs were higher in the presence of self-injurious behavior (adjusted odds ratio [aOR] 3.1; 95% confidence interval [CI] 1.7–5.4) compared with children without this indication for risperidone use, whereas the odds of AEs were lower among those using concomitant antibiotics (aOR 0.20; 95% CI 0.05–0.94) than among children not using antibiotics concomitantly with risperidone.
Extrapyramidal symptoms and daytime hypersomnia may be related to risperidone dose. Of 20 children with daytime hypersomnia, the starting dose of risperidone had been increased in four (20.0%), resulting in a risperidone dose of 0.75–5 mg/day at the time of the AE (ESM table). The remaining 16 (80.0%) children had daytime hypersomnia while on low starting doses (0.25–1 mg/day) of risperidone (ESM table). The frequency of increased dose among children with daytime hypersomnia did not differ from children with no risperidone AEs (p = 1.0). In children with extrapyramidal symptoms (n = 23), seven (30.4%) occurred on an increased risperidone dose of 2–6 mg/day, and 16 (69.6%) occurred at a low starting dose (0.25–1.5 mg/day) (ESM table). The frequency of increased risperidone dose did not differ among those with extrapyramidal symptoms and those without AEs (p = 0.45).
4 Discussion
Risperidone use in our cohort resulted in substantial number of common and rare AEs. On-label versus off-label use was not significantly associated with AE and, after controlling for the significant clinical variables, only self-injurious behavior and concomitant antibiotics were associated with AEs. The odds of AEs were higher in the presence of self-injurious behavior than in children without this indication for risperidone use, and lower with concomitant antibiotics.
Nearly one-third of this study cohort had experienced at least one AE, warranting close monitoring of children and adolescents treated with risperidone. Previous smaller studies involving children and adolescents with prolonged exposure to risperidone have reported higher rates (48–65%) [12, 13, 26], whereas a single study reported a lower rate (28.2%) [27]. Differences in the population studied, the methodology used, the duration of use of risperidone, and sample sizes may underlie the disparate AE rates. Our cohort included children and adolescents with a wide range of psychiatric and non-psychiatric disorders. By contrast, most prior studies of risperidone AEs involved children and adolescents with autism/autism spectrum disorder or disruptive behavior disorders [12, 13, 26, 27]. Our study was retrospective, with AEs detected from EHR documentation, whereas others were prospective, randomized, and double blind or open label, with active monitoring for AEs [12, 13, 26]. While the retrospective nature of our study leads to some limitations, merits of this design are less selection bias than prospective clinical trials and a focus on AEs that were documented by clinicians. Thus, our data may be more representative of “real-world” populations and clinically relevant findings. We also evaluated a larger cohort of 371 individuals, whereas the largest cohort published to date includes ≤172 individuals [13, 26,27,28,29].
Our cohort had a wide range of AEs, including common AEs (e.g., weight gain, extrapyramidal symptoms, and daytime hypersomnia) and rare AEs (e.g., premature adrenarche, precocious puberty, and early menstrual flow). Nearly one-quarter of our patients experienced multiple AEs. Consistent with other studies, common and rare AEs have been reported with risperidone among children and adolescents with autism and disruptive behavioral disorders, and weight gain is one of the most common AEs [12, 13, 26,27,28,29]. Some prior studies had reported respiratory system disorders as common AEs with risperidone (e.g., upper respiratory tract infection, rhinitis, pharyngitis) [12, 13], which we did not identify in our cohort. Respiratory AEs had previously been assessed as unrelated or of doubtful relationship to risperidone treatment [13] and thus may not have been documented as risperidone AEs in the EHR.
Extrapyramidal symptoms and daytime hypersomnia are common AEs with risperidone therapy and potentially related to risperidone dose. In our cohort, the majority of children with daytime hypersomnia experienced this effect while on a low starting dose of risperidone. An earlier study evaluating the efficacy and safety of low-dose (0.125 mg/day for children weighing 20 to < 45 kg; 0.175 mg/day for children weighing > 45 kg) and high-dose (1.25 mg/day for children weighing 20 to < 45 kg; 1.75 mg/day for children weighing > 45 kg) risperidone or placebo in 96 children and adolescents (aged 5–17 years) with autism reported hypersomnia (somnolence and sedation) following low- and high-dose exposures; however, the AE was more frequent in high-dose than low-dose groups [30]. Similarly, the majority of children in our cohort with extrapyramidal symptoms were on low starting doses of risperidone. Data from multiple fixed-dose (1–16 mg/day and placebo) trials of risperidone in adults with schizophrenia suggested extrapyramidal symptoms are risperidone dose related [31, 32]. Those on placebo or low-dose risperidone (1 mg/day) experienced more extrapyramidal symptoms than those on high doses (2–16 mg/day). Another study had shown that dystonia might occur in susceptible individuals during the first few days of risperidone use, even at low doses [32, 33].
One patient each experienced rare AEs, including droopy eyes, hyperthermia, early menstrual flow, fainting spell, precocious puberty, heavy tongue, hot flashes, multiple bruises, musculoskeletal pain, nervousness, oculogyric crisis, premature adrenarche, and restlessness. While there are reports of risperidone-induced AEs involving the ocular muscles (blepharospasm and oculogyric crisis) [26, 34], and potentially thermoregulatory disorder (febrile seizure) [29], the other rare AEs are not previously reported, and the mechanism is unknown. Some of these rare AEs may be attributed to comorbid conditions or concomitant medications and may not be truly risperidone-related. Nonetheless, it is important to make note of these rare AEs in the future monitoring of risperidone in children and adolescents.
Poor response was the major reason for increasing the dose of risperidone in our patients; of the 94 patients with dose increase to > 1 mg/day, 42.4% had AEs (Table 2 and ESM table). However, this is not surprising as previous studies had shown that higher doses of risperidone are associated with high rates of extrapyramidal symptoms and hypersomnia in children with various behavioral problems [35]. Further, the starting dose of risperidone was decreased in four patients and discontinued in 37 patients due to AEs (Table 2 and ESM table). Four other atypical antipsychotic agents (aripiprazole, olanzapine, paliperidone, and quetiapine) currently have FDA-approved indications for use in children and adolescents [36]. These other agents were used as alternatives to risperidone in our patients after discontinuation due to AEs. Aripiprazole was the most frequently used substitute for risperidone, and this may be attributed to its relatively lower AEs and good tolerability compared with other newer atypical antipsychotic agents [37]. Aripiprazole has been successfully used to address risperidone-induced mild hypothermia in an 11-year-old with schizophrenia [38].
Although the univariate analyses showed that dosing frequency and dose-modification pattern of risperidone were significantly associated with AEs (Table 2), these two factors did not remain significant in the multivariate analysis (Table 3). There is a lack of studies identifying risk factors for risperidone-induced AEs. However, younger age and higher medication dose have been reported as predictors of adverse weight gain in children exposed to risperidone for 8 weeks [39]. Despite weight gain being the most reported AE among our cohort, age at commencement of risperidone and increased dose did not significantly impact the risk for AEs in our cohort. By contrast, use of risperidone to treat self-injurious behavior was associated with a higher risk of AEs compared with children without this behavioral problem. This is a new finding that will be strengthened by validation in an independent dataset. It is noteworthy that children with autism spectrum disorder (ASD) and various forms of chromosomal abnormalities, which constitutes a significant proportion of our patients, are known to have a high prevalence of self-injurious behaviors [40], which might have influenced our observation that self-injurious behaviors are associated with AE risk. It is possible that AEs are reported with higher frequency in this subset, due to more frequent follow-up, higher vigilance for AEs, or more difficulty in discerning drug effects. These individuals may also be receiving additional drugs, contributing to AEs and drug–drug interactions. In addition, risperidone is primarily metabolized by the polymorphic cytochrome P450 2D6 enzyme (CYP2D6) [41]. A study comparing the distribution of CYP2D6*4 and CYP2D6*41 alleles (implicated in the efficacy and adverse effects of risperidone) in patients with ASD and healthy control groups showed higher frequencies of both alleles in patients with ASD [42]. This is a potential confounder that might have contributed to the high odds ratio of AEs among individuals with self-injurious behavior. Our ongoing study of the roles of CYP2D6 polymorphisms in risperidone AEs in children will test this hypothesis. Further, concomitant use of antibiotics was associated with a lower risk of AEs compared with children who did not use antibiotics. One potential mechanism for this observation is increased metabolism of risperidone due to enzymatic induction. An in vitro study demonstrated risperidone metabolism by CYP3A4 and CYP3A5 enzymes [43], which can be induced by antibiotics. Although we did not ascertain whether the antibiotics enhanced the metabolism of risperidone to produce this protective effect and cannot determine causation in this retrospective study, the impact of this minor metabolic pathway and this potential drug–drug interaction merit further investigation.
We acknowledge several limitations. This was a single-center study, and these findings may not be generalizable to the entire pediatric population. However, we believe our findings are robust based on the larger sample size analyzed compared with previous smaller studies [12, 13, 26,27,28,29]. Weight gain and sedation are common adverse effects of some concomitant drugs, such as valproic acid, used by our patients, which could potentially increase the prevalence of risperidone-induced weight gain and hypersomnia reported in this study [44]. Another limitation is that risperidone exposure and the associated AEs were audited retrospectively in the EHR, which may have missing and inaccurate data [45, 46]. For example, an AE ascertained at another hospital may not be captured [47, 48], we may not have complete ascertainment of mild AEs [49], the primary diagnoses and indications for risperidone exposure may not be complete, there may be errors in the documented dosing regimen, and weight and height were not serially assessed at every visit for every individual. Further, patients with early AEs may have been excluded from the study due to the inclusion criteria of ≥ 4 weeks of risperidone therapy. We did not perform causality assessment between the AEs and risperidone to exclude concomitant medications as the likely cause. Generally, AE refers to any problem occurring at the time a medicine is used, whether or not it is identified as a cause of the problem [50]. For this cohort with a high incidence of polypharmacy, other medications or a drug–drug interaction may have been truly responsible for some AEs. Our cohort size was not large enough to explore all possible risk factors (or combinations of risk factors) contributing to risperidone-related AEs. Meta-analysis across many cohorts may enable more granular detail and more precisely guide future prescribing advice.
5 Conclusions
Risperidone was associated with a significant proportion of one or more AEs among children and adolescents after using the medicine for ≥ 4 weeks. The age at commencement of risperidone, presence of comorbidities, dosing regimen of risperidone, and concomitant use of analgesics or orexigenic medicines did not predict AEs in this study, but there was an increased risk for AEs among patients with self-injurious behavior. Clinicians should be cautious in prescribing risperidone to patients with self-injurious behavior. Further research is needed to identify clinical factors or biomarkers to accurately predict risperidone AEs.
References
Cabaleiro T, Ochoa D, López-Rodríguez R, Román M, Novalbos J, Ayuso C, et al. Effect of polymorphisms on the pharmacokinetics, pharmacodynamics, and safety of risperidone in healthy volunteers. Hum Psychopharmacol. 2014;29:459–69.
Stahl S. Stahl’s essential psychopharmacology: neuroscientific basis and practical applications. 3rd ed. New York: Cambridge University Press; 2008.
Essick CJ. Examining the effect of FDA approval of risperdal for pediatric use on prescribing trends from 2005–2008. Public Health Theses, 2012. 1082. https://elischolar.library.yale.edu/cgi/viewcontent.cgi?article=1081&context=ysphtdl. Accessed 23 Feb 2019.
American Academy of Child and Adolescent Psychiatry (AACAP) Committee on quality issues. Practice parameter for the use of atypical antipsychotic medications in children and adolescents. https://www.aacap.org/App_Themes/AACAP/docs/practice_parameters/Atypical_Antipsychotic_Medications_Web.pdf. Accessed 5 June 2016.
Correll CU, Penzner JB, Parikh UH, Mughal T, Javed T, Carbon M, et al. Recognizing and monitoring adverse events of second-generation antipsychotics in children and adolescents. Child Adolesc Psychiatr Clin N Am. 2006;15:177–206.
Correll CU, Carlson HE. Endocrine and metabolic adverse effects of psychotropic medications in children and adolescents. J Am Acad Child Adolesc Psychiatry. 2006;45:771–91.
Safer DJ. A comparison of risperidone-induced weight gain across the age span. J Clin Psychopharmacol. 2004;24:429–35.
Findling RL, Kusumakar V, Daneman D, Moshang T, Desmedt G, Binder C. Prolactin levels during long-term risperidone treatment in children and adolescents. J Clin Psychiatry. 2003;64:1362–9.
Miyaji S, Yamamoto K, Hoshino S, Yamamoto H, Sakai Y, Miyaoka H. Comparison of the risk of adverse events between risperidone and haloperidol in delirium patients. Psychiatry Clin Neurosci. 2007;61:275–82.
Aman MG, Arnold LE, McDougle CJ, Vitiello B, Scahill L, Davies M, et al. Acute and long-term safety and tolerability of risperidone in children with autism. J Child Adolesc Psychopharmacol. 2005;15:869–84.
Gencer O, Emiroglu FN, Miral S, Baykara B, Baykara A, Dirik E. Comparison of long-term efficacy and safety of risperidone and haloperidol in children and adolescents with autistic disorder. An open label maintenance study. Eur Child Adolesc Psychiatry. 2008;17:217–225.
Haas M, Karcher K, Pandina GJ. Treating disruptive behavior disorders with risperidone: a 1-year, open-label safety study in children and adolescents. J Child Adolesc Psychopharmacol. 2008;18:337–45.
Reyes M, Buitelaar J, Toren P, Augustyns I, Eerdekens M. A randomized, double-blind, placebo-controlled study of risperidone maintenance treatment in children and adolescents with disruptive behavior disorders. Am J Psychiatry. 2006;163:402–10.
Malone RP, Maislin G, Choudhury MS, Gifford C, Delaney MA. Risperidone treatment in children and adolescents with autism: short- and long-term safety and effectiveness. J Am Acad Child Adolesc Psychiatry. 2002;41:140–7.
McDougle CJ, Holmes JP, Bronson MR, Anderson GM, Volkmar FR, Price LH, et al. Risperidone treatment of children and adolescents with pervasive developmental disorders: a prospective open-label study. J Am Acad Child Adolesc Psychiatry. 1997;36:685–93.
Findling RL, McNamara NK, Branicky LA, Schluchter MD, Lemon E, Blumer JL. A double-blind pilot study of risperidone in the treatment of conduct disorder. J Am Acad Child Adolesc Psychiatry. 2000;39:509–16.
Calarge CA, Ziegler EE. Iron deficiency in pediatric patients in long-term risperidone treatment. J Child Adolesc Psychopharmacol. 2013;23:101–9.
Szarfman A, Tonning JM, Levine JG, Doraiswamy PM. Atypical antipsychotics and pituitary tumors: a pharmacovigilance study. Pharmacotherapy. 2006;26:748–58.
Calarge CA, Zimmerman B, Xie D, Kuperman S, Schlechte JA. A cross-sectional evaluation of the effect of risperidone and selective serotonin reuptake inhibitors on bone mineral density in boys. J Clin Psychiatry. 2010;71:338–47.
Milani GP, Bianchetti MG, Mazzoni MB, Triulzi F, Mauri MC, Agostoni C, Fossali EF. Arterial hypertension and posterior reversible cerebral edema syndrome induced by risperidone. Pediatrics. 2014;133:e771–4.
Mulla H. Understanding developmental pharmacodynamics: importance for drug development and clinical practice. Paediatr Drugs. 2010;12:223–33.
Roden DM, Pulley JM, Basford MA, Bernard GR, Clayton ER, Balser JR, et al. Development of a large-scale de-identified DNA biobank to enable personalized medicine. Clin Pharmacol Ther. 2008;84:362–9.
McGregor TL, Van Driest SL, Brothers KB, Bowton EA, Muglia LJ, Roden DM. Inclusion of pediatric samples in an opt-out biorepository linking DNA to de-identified medical records: pediatric BioVU. Clin Pharmacol Ther. 2013;93:204–11.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
Xu H, Stenner SP, Doan S, Johnson KB, Waitman LR, Denny JC. MedEx: a medication information extraction system for clinical narratives. J Am Med Informatics Assoc. 2010;17:19–24.
Kent JM, Hough D, Singh J, Karcher K, Padina G. An open-label extension study of the safety and efficacy of risperidone in children and adolescents with autistic disorder. J Child Adolesc Psychosopharmacol. 2013;23:676–86.
Youngster I, Zachor DA, Gabis LV, Bar-Chaim A, Benveniste-Levkovitz P, Britzi M, et al. CYP2D6 genotyping in paediatric patients with autism treated with risperidone: a preliminary cohort study. Dev Med Child Neurol. 2014;56:990–4.
Aman MG, Arnold LE, McDougle CJ, Vitiello B, Scahill L, Davies M, et al. Acute and long-term safety and tolerability of risperidone in children with autism. J Child Adolesc Psychopharmacol. 2005;15:869–84.
Malone RP, Maislin G, Choudhury MS, Gifford C, Delaney MA. Risperidone treatment in children and adolescents with autism: short- and long-term safety and effectiveness. J Am Acad Child Adolesc Psychiatry. 2002;41:140–7.
Kent JM, Kushner S, Ning X, Karcher K, Ness S, Aman M, Singh J, Hough D. Risperidone dosing in children and adolescents with autistic disorder: a double-blind, placebo-controlled study. J Autism Dev Disord. 2013;43(8):1773–83.
Thomson SR, Chogtu B, Bhattacharjee D, Agarwal S. Extrapyramidal symptoms probably related to risperidone treatment: a case series. Ann Neurosci. 2017;24(3):155–63.
Risperdal® (risperidone). Highlights of prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/020272s056,020588s044,021346s033,021444s03lbl.pdf. Accessed 30 Nov 2018.
Chandra NC, Sheth SA, Mehta RY, Dave KR. Severe tardive dystonia on low dose short duration exposure to atypical antipsychotics: factors explored. Indian J Psychol Med. 2017;39(1):96–8.
Masliyah T, Ad-Dab’bagh Y. Low-dose risperidone-induced oculogyric crises in an adolescent male with autism, Tourette’s and developmental delay. J Can Acad Child Adolesc Psychiatry. 2011;20:214–6.
Vanwong N, Srisawasdi P, Ngamsamut N, Nuntamool N, Puangpetch A, Chamkrachangpada B, Hongkaew Y, Limsila P, Kittitharaphan W, Sukasem C. Hyperuricemia in children and adolescents with autism spectrum disorder treated with risperidone: the risk factors for metabolic adverse effects. Front Pharmacol. 2017;7:527. https://doi.org/10.3389/fphar.2016.00527 (eCollection 2016).
Saljoughian M. Atypical antipsychotics: safety and use in pediatric patients. US Pharm. 2015;40(5):52–5.
Harrison JN, Cluxton-Keller F, Gross D. Antipsychotic medication prescribing trends in children and adolescents. J Pediatr Health Care. 2012;26(2):139–45.
Grau K, Plener PL, Gahr M, Denzer C, Freudenmann RW. Mild hypothermia in a child with low-dose risperidone: a case report. Zeitschrift für Kinder- und Jugendpsychiatrie und Psychotherapie. 2017;45:335–7.
Hoekstra PJ, Troost PW, Lahuis BE, Mulder H, Mulder EJ, Franke B, et al. Risperidone-induced weight gain in referred children with autism spectrum disorders is associated with a common polymorphism in the 5-hydroxytryptamine 2C receptor gene. J Child Adolesc Psychopharmacol. 2010;20:473–7.
Oliver C, Richards C. Practitioner review: self-injurious behaviour in children with developmental delay. J Child Psychol Psychiatry. 2015;56(10):1042–54.
Mannens G, Huang ML, Meuldermans W, Hendrickx J, Woestenborghs R, Heykants J. Absorption, metabolism, and excretion of risperidone in humans. Drug Metab Disp. 1993;21(6):1134–41.
Bauze D. Genetic aspects of autism spectrum disorders. Summary of the Doctoral Thesis for obtaining the degree of a Doctor of Medicine, Speciality—Medical Genetics. Rīga, 2014. https://pdfs.semanticscholar.org/eae0/d6ba0dc08fe731f3b652810a69699739aff2.pdf. Accessed 30 Nov 2018.
Fang J, Bourin M, Baker GB. Metabolism of risperidone to 9-hydroxyrisperidone by human cytochromes P450 2D6 and 3A4. Naunyn Schmiedebergs Arch Pharmacol. 1999;359:147–51.
Rocha GP, Batista BH, Nunes ML. Use of psychoactive and antiepileptic drugs: guidelines for pediatricians. J Pediatr (Rio J). 2004;80(2 Suppl):S45–55.
Madden JM, Lakoma MD, Rusinak D, Lu CY, Soumerai SB. Missing clinical and behavioral health data in a large electronic health record (EHR) system. J Am Med Informatics Assoc. 2016;23:1143–9.
Stiglic G, Kocbek P, Fijacko N, Sheikh A, Pajnkihar M. Challenges associated with missing data in electronic health records: a case study of a risk prediction model for diabetes using data from Slovenian primary care. Health Informatics J. 2017;1460458217733288. https://doi.org/10.1177/1460458217733288 (Epub ahead of print)
Wilson RM, Runciman WB, Gibberd RW, Harrison BT, Newby L, Hamilton JD. The quality in Australian health care study. Med J Aust. 1995;163:458–71.
Leape LL, Brennan TA, Laird N, Lawthers AG, Localio AR, Barnes BA, et al. The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II. N Engl J Med. 1991;324:377–84.
Zegers M, de Bruijne MC, Wagner C, Groenewegen PP, Waaijman R, van der Wal G. Design of a retrospective patient record study on the occurrence of adverse events among patients in Dutch hospitals. BMC Health Serv Res. 2007;7:27. https://doi.org/10.1186/1472-6963-7-27.
Bates DW, Cullen DJ, Laird N, Petersen LA, Small SD, Servi D, et al. Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE Prevention Study Group. JAMA. 1995;274:29–34.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
The study was reviewed by the Vanderbilt Institutional Review Board and determined to be non-human subjects research.
Conflict of Interest
Dr. Van Driest has been an invited speaker to Merck. Dr. Oshikoya, Dr. Carroll, Ms. Aka, and Dr. Roden have no conflicts of interest that are directly relevant to the content of this article.
Funding
This work used a dataset from Vanderbilt University Medical Center’s BioVU, which is supported by the Vanderbilt Institute for Clinical and Translational Research (VICTR) and the National Institutes of Health (NIH) National Center for Advancing Translational Sciences grants UL1 TR000445. This work was also supported by KL2 TR000446 (SLV), Burroughs Wellcome Fund Innovation in Regulatory Science Award 1015006 (SLV), Doris Duke Clinical Scientist Development Award 2017075 (SLV), and NIH/National Institute of General Medical Sciences Clinical Pharmacology Training Program 5T32 GM007569 (KAO).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Oshikoya, K.A., Carroll, R., Aka, I. et al. Adverse Events Associated with Risperidone Use in Pediatric Patients: A Retrospective Biobank Study. Drugs - Real World Outcomes 6, 59–71 (2019). https://doi.org/10.1007/s40801-019-0151-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-019-0151-7