Abstract
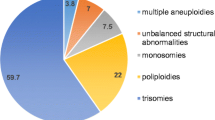
Spontaneous miscarriages are strongly associated with fetal chromosomal abnormalities. We sought to validate the occurrence of chromosomal abnormalities in Japanese patients with early spontaneous miscarriages using a conventional long-term culture method. One hundred and thirty-two patients were studied after excluding 7 cases with culture failure. Chromosomal analysis of 132 cases was performed using a long-term culture method of the villous placental tissue. Patients’ age, number of previous spontaneous abortions, fetal data from ultrasonography, and the method of conception (ART or spontaneous pregnancy) were obtained from the electronic medical records. The association between the patient’s background and the cytogenetic data was analyzed using a Chi squared test. The average maternal age of the 132 cases of early spontaneous abortion was 34.2 ± 4.7 year (range: 24–43). Chromosomal abnormalities were detected in 89 cases (67.4%), among which 52.8% represented trisomy, 1.1% represented double trisomy, 10.1% represented polyploidy, 7.9% represented monosomy, 12.4% represented structural chromosomal abnormality, and 15.7% represented mosaic chromosome abnormalities. Women older than 35 year had a higher rate of chromosomal abnormalities than younger women (76.6% vs. 58.8%; P = 0.015). Twenty-five of the 132 pregnancies were achieved with ART and were associated with a higher rate of trisomy (64.0% vs. 37.4%; P = 0.008). G-banding identified a rare form of polyploidy 94,XXYYYY. Our results confirmed previous findings that older Japanese women with spontaneous miscarriages have a higher rate of chromosomal abnormalities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Early spontaneous miscarriage occurs in 10–15% of all pregnancies, and may be caused by maternal disorders, such as diabetes and antiphospholipid syndrome, [1] antibiotic consumption, [2] body mass index, [3] etc. Chromosomal abnormalities are observed in 50–70% of spontaneous miscarriages and are reported to be the most common cause of spontaneous miscarriage [4,5,6]. These studies indicate that cytogenetic analysis of chorionic villi is crucial in understanding the cause of fetal loss and assess the risk of recurrence [6].
The incidence of fetal chromosomal abnormalities is known to increase with increasing maternal age [7,8,9]. The influence of other factors, such as assisted reproduction techniques (ART) and the number of previous miscarriages, has also been investigated, but the results are inconsistent [10,11,12,13]. While Bonduelle and colleagues [10] reported a higher incidence of chromosomal abnormalities in women undergoing ART, a recent study by Wu and colleagues [11] found no such association.
Similarly, contradictory reports exist on the influence of previous miscarriages on miscarriage recurrence. Ogasawara et al. showed that the incidence of miscarriages increased with the number of previous spontaneous abortions; [12] however, a recent study by Goldstein et al. contradicted the existence of such a correlation [13].
Studies by Jenderny et al. and Menasha et al. examined chromosomal aberrations in large scale cohorts of spontaneous miscarriages [14, 15]. In this study, we corroborated these previous findings in a small-scale Japanese cohort. We also examined the relationship between the patient’s background and the occurrence and type of chromosomal abnormality.
Materials and Methods
Patient Information
Pregnant women who experienced a spontaneous abortion within the first 12 gestational weeks (as confirmed by clinical ultrasonography) were enrolled in the study. One hundred and six cases from January 2001 to December 2009 at the Hyogo College of Medicine and 33 cases from July 2012 to March 2018 at the Jichi Medical University Saitama Medical Center who underwent chorionic villous chromosome examination were included in this study. The study was performed prior to elective dilation and curettage procedures. The protocol was approved by the Ethics Committee and all participants provided written informed consent in opt-out documents prior to the study.
Patients were included as per the following criteria: (1) gestational sac empty diameter ≥ 25 mm, (2) crown-rump lengths ≥ 7 mm for embryos with no cardiac activity, or (3) no cardiac activity upon the initial scan and post 7 days scan for embryos with a crown-rump length < 7 mm.
A miscarriage was diagnosed following international guidelines [16]. Cases were limited to a single fetus with no evidence of progressing abortion or villus contamination to avoid culture failure. Information regarding patients’ age, number of previous spontaneous abortions, fetal data from ultrasonography, and method of conception (ART or spontaneous pregnancy) were obtained from the electronic medical records. Information about the fetal sex ratio was also collected.
Chromosomal Examination
Chromosomal examination was performed on the collected villous placental tissue using a long-term culture method [5]. Briefly, 50–100 mg of villous tissue was harvested and immediately cleaned to remove maternal blood. Subsequently, the tissue was rinsed 5 times with a solution containing alfa-MEM (Sigma-Aldrich), penicillin, and streptomycin. The specimen was then transferred to a 35-mm petri dish in 5 mL of Chang’s medium (Irvine Scientific) and incubated at 37 °C, 5% CO2 for 1–2 weeks. The medium was changed 2–3 times per week. Following confirmation of adequate cell growth of the tissue explants, colcemid (1 µg/mL; Adipo Gen) was added to the medium for 2–3 h. The medium was subsequently removed, and the dishes were washed for 3–4 min in phosphate buffered saline and 0.5% trypsin–EDTA solution (Sigma-Aldrich). Finally, the cells were aspirated, centrifuged, treated with 0.075 M hypotonic KCl for 15 min, and fixed in 3 changes of Carnoy’s fixative. Chromosome preparations were made by transferring the cell suspensions onto clean slides and allowing them to air-dry at room temperature (25–27 °C) Coverslips were G-banded following standard laboratory techniques [17].
Ultrasonography
Transvaginal ultrasonography was performed by experienced sonographers using a 5–9 MHz vaginal probe (GE Voluson E8/730, GE Tech Co., Ltd., New York, America). All patients received at least two ultrasonography examinations at our hospital between the 6th and 12th weeks of gestation to diagnose spontaneous miscarriage.
Statistical Analysis
Data were analyzed for potential associations between patients’ background and the presence of fetal chromosomal abnormalities using a Chi squared test. P < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS (version 19.0, SPSS Inc, Chicago, IL, USA) software.
Results
Among the 139 cases of spontaneous abortion, chromosome analysis was successfully performed for 132 cases (culture success rate = 95.0%). Seven cases were excluded due to contamination of the culture.
The mean age of the patients was 34.2 ± 4.7 y (range: 24–43), the mean number of gestational weeks was 8.8 ± 1.2 weeks (range: 6–11), and the mean number of previous spontaneous abortions was 1.1 ± 1.4 (range: 0–6).
Chromosomal analysis revealed a normal karyotype in 43 cases (32.6%) and abnormalities in 89 (67.4%) cases. The results of the cytogenetic analyses are summarized in Table 1 and Supplementary Table 1. The most commonly found abnormality was trisomies (52.8%). Other abnormalities included double trisomy (1.1%), polyploidy (triploidy: 5.6%; tetraploidy: 4.5%), monosomy (45,X) (7.9%), structural abnormality (12.4%), and mosaicism (15.7%) (Table 1). The types of mosaic and structural abnormalities found are described in Supplementary Table 1.
Chromosomal abnormalities were significantly associated with maternal age. Women with abnormal karyotypes tended to be older than women with a normal karyotype (abnormal karyotype: 89 (67.4%), age: 34.8 ± 4.8 year vs. normal karyotype: 43 (32.6%), age: 33.1 ± 4.5 year; P = 0.034) (Supplementary Table 2). To further explore the effect of maternal age, patients were grouped according to age (< 35 or ≥ 35 year of age) and the incidence of chromosomal abnormalities was analyzed (Supplementary Table 3). Women older than 35 year were found to have a significantly higher rate of chromosomal abnormalities (58.8% for women < 35 year old vs. 76.6% for women ≥ 35 year old; P = 0.015). These women also had a significantly higher rate of trisomy (35.3% for women < 35 year old vs. 50.0% for women ≥ 35 year old; P = 0.044).
Trisomy cases included mosaic cases (normal karyotype/trisomy and normal karyotype/double trisomy) and double trisomy cases. Only one case (normal karyotype/trisomy/tetraploidy) was not counted as a trisomy as the number of trisomy cells was small.
The association between the number of previous spontaneous abortions and the frequency of chromosomal abnormalities is presented in Table 2. The number of previous spontaneous abortions did not significantly affect the frequency of chromosomal abnormalities (68.1% for 0–2 vs. 63.2% for ≥ 3; P = 0.334).
Of the 132 patients included in the study, ART treatment resulted in 25 pregnancies, which include conventional IVF (n = 14) and intracytoplasmic sperm injection (n = 11). Women who underwent ART treatment were older than those who conceived spontaneously (37.4 ± 4.1 year for ART vs. 33.5 ± 4.6 year for non-ART; P < 0.01) (Table 3). Although, the overall occurrence of chromosomal abnormalities did not differ significantly between ART and non-ART treated women (P = 0.154), the number of trisomies was significantly higher in ART treated women (64.0% for ART vs. 37.4% for non-ART; P = 0.008).
Regarding the sex ratio of fetuses in all 132 cases, the Y chromosome was detected in 49 cases (37.1%) and not detected in 83 cases (62.9%). In the 89 cases with an abnormal karyotype, the Y chromosome was detected in 37 cases (41.6%) and absent in 52 cases (58.4%). In the 43 cases with a normal karyotype, 12 cases were 46,XY (27.9%) and 31 cases were 46,XX (72.1%).
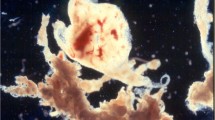
G-banding identified a rare form of polyploidy 94,XXYYYY as shown in Fig. 1.
Discussion
Here, we investigated chromosomal abnormalities in 132 cases of spontaneous miscarriage diagnosed at our clinic. Our study found that 67.4% of all cases had chromosomal abnormalities that included trisomies, polyploidy, monosomy, structural abnormalities, and mosaicism. The percentage of chromosomal abnormalities increased with increasing maternal age (women ≥ 35 year old) but was not affected by previous spontaneous abortions. Women who conceived using ART had a higher percentage of trisomies. Our study is a confirmatory investigation and adds to the literature on this topic in the Japanese population [14, 15, 18].
In our study, chromosomal abnormalities were detected in 67.4% of the analyzed samples, which falls within the previously reported range of 50–70% [6, 19, 20]. It has been suggested that chorionic villous cells with chromosomal abnormalities may have impaired proliferative capacity in long-term in vitro cultures, leading to the underestimation of the abnormality rate [21]. In fact, several studies have reported higher rates of fetal chromosomal abnormalities [22,23,24]. It is possible that the lower abnormality rate in our study resulted from reduced proliferative capacity of villous cells with abnormal chromosomes.
Nevertheless, our results indicated that women over 35 year of age present a higher occurrence of chromosomal abnormalities than those younger than 35 year. This result is consistent with findings that report an increase in the chromosomal abnormality rate with increasing maternal age [19, 25, 26].
In terms of abnormality types, we found that the highest proportion corresponded to trisomy (52.8%), followed by structural abnormalities (12.4%), polyploidy (10.1%) and monosomy (7.9%). Mosaics of the normal karyotype and chromosomal aberrations were observed in 15.7% of the cases, and double trisomy was observed in 1.1% of the cases. Comparable proportions have been reported in previous studies [27, 28].
The most frequent trisomy detected in our study was trisomy 16, which is similar to a past report by Soler et al. [6] We only found one case of trisomy 17, which is known to be rare [29]. Several important genes are present on chromosome 17 and its abnormality may be lethal at a very early stage in embryonic development, leading to a lower incidence of this trisomy in our study [30]. Similar to past reports, polyploidies were not uncommon in this study, but one rare case of 94,XXYYYY was detected. This karyotype is known to be associated with sperm chromosome abnormality [31]. In our study, this karyotype was found in a recurrent miscarriage case with no paternal chromosomal abnormalities. Therefore, it is possible that this karyotype resulted from meiosis errors during spermatogenesis.
Most cases of trisomy derive from errors in maternal meiosis (meiotic non-disjunction), in which advanced maternal age is a risk factor [19]. In line with this, the trisomy rate was found to be significantly higher in women older than 35 year compared to younger women in our study.
Although a study has reported an increased likelihood of a future pregnancy loss in cases with a history of spontaneous miscarriages, [32] the relationship between previous miscarriages and the occurrence of fetal chromosomal abnormalities remains controversial [12, 13]. We found no significant difference in the occurrence of chromosomal abnormalities between women with 3 or more previous miscarriages and those with less than 2 miscarriages.
Similarly, reports about the influence of ART on the occurrence of fetal chromosomal abnormalities are contradictory [10, 11]. In this study, the overall occurrence of fetal chromosomal abnormalities was not significantly different between ART and non-ART patients. However, the proportion of trisomy was higher in ART patients. In addition, the age of ART women was significantly higher than that of non-ART mothers. This may imply that the higher rate of trisomy may be an indirect consequence of higher age, rather than a direct consequence of the ART technique. It has been reported that the age of Japanese women seeking ART is increasing [33].
The Y chromosome was less frequently detected in patients with a normal karyotype than those with an abnormal karyotype. This could result from maternal cell contamination [34]. It is possible to identify this using quantitative fluorescent polymerase chain reaction (QF-PCR); [35] however, this was not performed as the patient did not agree to incur the additional cost. Although there was only a slight increase in the percentage of the Y chromosome in patients with an abnormal karyotype, more studies are required to rule out maternal cell contamination.
Karyotyping has been used as a conventional method for genetic analysis of products of conception [36]. However, the need to culture the cells and the possibility of maternal cell contamination lead to a high percentage of sample loss (approx. 20–40%). In a genetic analysis by Sahoo et al. [36] 91% of samples were successfully analyzed using chromosomal microarray analysis. Although we did not compare the results of our method with more sensitive methods like microarray analysis, we successfully analyzed 95% (132/139) of the samples using a long-term culturing method. Future studies comparing the success rate of both methods in large sample cohorts will be useful.
This study is limited by the small sample size and the use of only one method for genetic analysis. The effect of maternal cell contamination on the sex ratio was not determined using additional techniques like QF-PCR. Future studies addressing these issues are warranted.
In conclusion, our study confirmed previous reports of chromosomal abnormalities in patients with spontaneous miscarriages in a Japanese cohort. Future large-scale prospective studies comparing the different analytical methods are required.
References
Massalska D, Zimowski JG, Bijok J, Pawelec M, Czubak-Barlik M, Jakiel G, et al. First trimester pregnancy loss: clinical implications of genetic testing. J Obstet Gynaecol Res. 2017;43:23–9.
Muanda FT, Sheehy O, Bérard A. Use of antibiotics during pregnancy and the risk of major congenital malformations: a population based cohort study. Br J Clin Pharmacol. 2017;2017(83):2557–71.
Jung SJ, Park SK, Shin A, Lee SA, Choi JY, Hong YC, et al. Body mass index at age 18–20 and later risk of spontaneous abortion in the health examinees study (HEXA). BMC Pregnancy Childbirth. 2015;2015(15):228.
Yuan SM, Liao C, Li DZ, Huang JZ, Hu SY, Ke M, et al. Chorionic villus cell culture and karyotype analysis in 1 983 cases of spontaneous miscarriage. Zhonghua Fu Chan Ke Za Zhi. 2017;52:461–6 In Chinese.
Kajii T, Ferrier A, Niikawa N, Takahara H, Ohama K, Avirachan S. Anatomic and chromosomal anomalies in 639 spontaneous abortuses. Hum Genet. 1980;55:87–98.
Soler A, Morales C, Mademont-Soler I, Margarit E, Borrell A, Borobio V, et al. Overview of chromosome abnormalities in first trimester miscarriages: a series of 1,011 consecutive chorionic villi sample karyotypes. Cytogenet Genome Res. 2017;152:81–9.
Ohno M, Maeda T, Matsunobu A. A cytogenetic study of spontaneous abortions with direct analysis of chorionic villi. Obstet Gynecol. 1991;77:394–8.
Teles TM, Paula CM, Ramos MG, Costa HB, Andrade CR, Coxir SA, et al. Frequency of chromosomal abnormalities in products of conception. Rev Bras Ginecol Obstet. 2017;39:110–4.
Dai R, Li L, Zhu H, Geng D, Deng S, Liu R. Effect of maternal age on spontaneous abortion during the first trimester in Northeast China. J Matern Fetal Neonatal Med. 2018;31:1824–9.
Bonduelle M, Aytoz A, Van Assche E, Devroey P, Liebaers I, Van Steirteghem A. Incidence of chromosomal aberrations in children born after assisted reproduction through intracytoplasmic sperm injection. Hum Reprod. 1998;13:781–2.
Wu T, Yin B, Zhu Y, Li G, Ye L, Chen C, et al. Molecular cytogenetic analysis of early spontaneous abortions conceived from varying assisted reproductive technology procedures. Mol Cytogenet. 2016;9:79.
Ogasawara M, Aoki K, Okada S, Suzumori K. Embryonic karyotype of abortuses in relation to the number of previous miscarriages. Fertil Steril. 2000;73:300–4.
Goldstein M, Svirsky R, Reches A, Yaron Y. Does the number of previous miscarriages influence the incidence of chromosomal aberrations in spontaneous pregnancy loss? J Matern Fetal Neonatal Med. 2017;30:2956–60.
Jenderny J. Chromosome aberrations in a large series of spontaneous miscarriages in the German population and review of the literature. Mol Cytogenet. 2014;7:38.
Menasha J, Levy B, Hirschhorn K, Kardon NB. Incidence and spectrum of chromosome abnormalities in spontaneous abortions: new insights from a 12-year study. Genet Med. 2005;7(4):251–63.
Preisler J, Kopeika J, Ismail L, Vathanan V, Farren J, Abdallah Y, et al. Defining safe criteria to diagnose miscarriage: prospective observational multicenter study. BMJ. 2015;351:h4579.
Cheung SW, Crane JP, Beaver HA, Burgess AC. Chromosome mosaicism and maternal cell contamination in chorionic villi. Prenat Diagn. 1987;7:535–42.
Nagaishi M, Yamamoto T, Iinuma K, Shimomura K, Berend SA, Knops J. Chromosome abnormalities identified in 347 spontaneous abortions collected in Japan. J Obstet Gynaecol Res. 2004;30(3):237–41.
Geisler M, Kleinebrecht J. Cytogenetic and histologic analyses of spontaneous abortions. Hum Genet. 1978;45:239–51.
Hassold T, Chen N, Funkhouser J, Jooss T, Manuel B, Matsuura J, et al. A cytogenetic study of 1000 spontaneous abortions. Ann Hum Genet. 1980;1980(44):151–78.
Qumsiyeh MB, Kim KR, Ahmed MN, Bradford W. Cytogenetics and mechanisms of spontaneous abortions: increased apoptosis and decreased cell proliferation in chromosomally abnormal villi. Cytogenet Genome Res. 2000;88(3–4):230–5.
Shah MS, Cinnioglu C, Maisenbacher M, Comstock I, Kort J, Lathi RB. Comparison of cytogenetics and molecular karyotyping for chromosome testing of miscarriage specimens. Fertil Steril. 2017;107:1028–33.
Thorne J, Craffey A, Nulsen JC 3rd. Detection of an inherited deletion in products of conception in a patient with recurrent losses and normal karyotype. Obstet Gynecol. 2017;130:126–9.
Lee YX, Chen CW, Lin YH, Tzeng CR, Chen CH. Prediction of a rare chromosomal aberration simultaneously with next generation sequencing-based comprehensive chromosome screening in human preimplantation embryos for recurrent pregnancy loss. J Assist Reprod Genet. 2018;35:171–6.
Choi TY, Lee HM, Park WK, Jeong SY, Moon HS. Spontaneous abortion and recurrent miscarriage: a comparison of cytogenetic diagnosis in 250 cases. Obstet Gynecol Sci. 2014;57:518–25.
Jia CW, Wang L, Lan YL, et al. Aneuploidy in early miscarriage and its related factors. Chin Med J (Engl). 2015;128:2772–6.
Russo R, Sessa AM, Fumo R, Gaeta S. Chromosomal anomalies in early spontaneous abortions: interphase FISH analysis on 855 FFPE first trimester abortions. Prenat Diagn. 2016;36:186–91.
Segawa T, Kuroda T, Kato K, Kuroda M, Omi K, Miyauchi O, et al. Cytogenetic analysis of the retained products of conception after missed abortion following blastocyst transfer: a retrospective, large-scale, single-centre study. Reprod Biomed Online. 2017;34:203–10.
Horiuchi I, Hashimoto T, Tsuji Y, Shimada H, Furuyama J, Koyama K. Direct assessment of triploid cells in mosaic human fetuses by fluorescence in situ hybridization. Mol Hum Reprod. 1997;3(5):445–50.
Baranov VS. Role of various portions of chromosome 17 in the early embryogenesis of the laboratory mouse. Genetika. 1983;19(2):246–54.
Milazzo JP, Rives N, Mousset-Siméon N, Macé B. Chromosome constitution and apoptosis of immature germ cells present in sperm of two 47. XYY infertile males. Hum Reprod. 2006;21(7):1749–58.
Poorolajal J, Cheraghi P, Cheraghi Z, Ghahramani M, Doosti Irani A. Predictors of miscarriage: a matched case-control study. Epidemiol Health. 2014;36:e2014031.
Irahara M, Kuwahara A, Iwasa T, Ishikawa T, Ishihara O, Kugu K, et al. Assisted reproductive technology in Japan: a summary report of 1992–2014 by the Ethics Committee, Japan Society of Obstetrics and Gynecology. Reprod Med Biol. 2017;16:126–32.
Lathi RB, Gustin SL, Keller J, Maisenbacher MK, Sigurjonsson S, Tao R, et al. Reliability of 46, XX results on miscarriage specimens: a review of 1,222 first-trimester miscarriage specimens. Fertil Steril. 2014;101(1):178–82.
Guzel AI, Demirhan O, Pazarbasi A, Ozgunen FT, Kocaturk-Sel S, Tastemir D. Detection of parental origin and cell stage errors of a double nondisjunction in a fetus by QF-PCR. Genet Test Mol Biomark. 2009;13(1):73–7.
Sahoo T, Dzidic N, Strecker MN, Commander S, Travis MK, Doherty C, et al. Comprehensive genetic analysis of pregnancy loss by chromosomal microarrays: outcomes, benefits, and challenges. Genet Med. 2017;19(1):83–9.
Acknowledgements
We acknowledge the editorial support, including manuscript writing based on detailed directions provided by the authors, collating author comments, copyediting, cross-referencing, and referencing provided by Editage.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical Approval Statements
The protocol was approved by the Ethics Committee of Jichi Medical University, Japan (Ethics Committee Approval Number Rin-S17-100), and all participants provided written informed consent in opt-out documents prior to the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Horiuchi, I., Wakimoto, Y., Kuwata, T. et al. Cytogenetic Analysis of Spontaneous Miscarriages Using Long-Term Culturing of Chorionic Villi. J. Fetal Med. 6, 1–6 (2019). https://doi.org/10.1007/s40556-018-0190-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40556-018-0190-2