Abstract
Background
The development of sensitive myocardial-specific cardiac biomarkers allows for detection of very small amounts of myocardial injury or necrosis. Myocardial injury (MI) as a prelude of the serious perioperative complication myocardial infarction, should be paid more attention, especially in elderly susceptible patients. Myocardial injury after abdominal surgery in elderly patients has not been described yet. The objectives of this study were to identify the incidence, predictors, characteristics and the impact of MI on outcome in elderly patients underwent abdominal surgery.
Methods
Patients aged ≥ 65 who underwent abdominal surgery longer than 2 h between January 2016 and March 2017 were reviewed. Patients with peak troponin I level of 0.04 ng/ml or greater (abnormal laboratory threshold) within once-administration-period and without non-ischemia troponin elevation proof (e.g., sepsis) were assessed for characteristics and prognosis. Risk factors of MI were determined by multivariable regression.
Results
Among 285 patients with whole information, 36 patients (12.6%) suffered MI, only 2 patients (0.7%) fulfilled definition of myocardial infarction. With most of them occurred within first 7 days after surgery. Multivariable analysis showed that coronary artery disease (CAD) history [odds ratio (OR) 2.817, P = 0.015], non-laparoscopic surgery (OR 5.181, P = 0.030), blood loss ≥ 800 ml (OR 3.430, P = 0.008), non-venous maintain (OR 2.105, P = 0.047), and infection (OR 4.887, P = 0.008) as risk factors for MI. MI was associated with longer hospital stay (P = 0.006), more cardiac consultation (P = 0.011), higher infection(P = 0.016) and reoperation(P = 0.026) rate.
Conclusion
MI is common in elderly patients who underwent abdominal surgery, while myocardial infarction is infrequent. They are both associated with risk factors and worse prognosis. MI deserves more attention especially in elderly patients. Troponin I measurement is a useful test after massive surgery, which can help risk-stratifying patients, effective preventing, prompt managing and predicting outcomes. Routine monitoring of cardiac biomarkers especially within 7 days after abdominal surgery in elderly patients is recommended.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Important organs all become vulnerable with aging, therefore, the possibility of cardiac event is increased in elderly patients [1]. Elderly patients with surgical disease have a high prevalence of cardiac risk factors and the stress of abdominal surgery predisposes these patients to major cardiac events [2]. Cardiac events are one of the leading causes of mortality in non-cardiac surgery patients. Among them myocardial infarction is the most common postoperative complication [3].
With the development of more sensitive and myocardial-specific cardiac biomarkers, we can detect small amounts of myocardial injury and necrosis, which improved the definition of myocardial infarction, and highlighted the cardiac biomarker at the same time [4].
Some studies have shown that troponin levels are highly predictive of patient and graft survival following liver transplantation, helping risk stratify patients [5]. Recently, some studies clearified the definition of myocardial injury, extending the range of myocardial infarction to small myocardial injury, and demonstrated that myocardial injury after non-cardiac surgery is common and associated with substantial mortality [6, 7]. To our knowledge, there is no study about myocardial injury after abdominal surgery in elderly patients so far.
We performed this study aiming to identify the incidence, predictors, characteristics and impact on prognosis of MI in elderly patients underwent abdominal surgery.
Materials and methods
After approved by the Beijing Hospital Institutional Review Board(2016BJYYEC-030-01), the retrospective study was carried out at National Center of Gerontology. The medical records of patients ≥ 65 who underwent abdominal surgery longer than 2 h between January 2016 and March 2017 were reviewed.
Cardiac evaluation and treatment were done by cardiac physician preoperatively, cardiac risk factors and cardiac medical history were collected in detail; patients’ nowadays cardiac symptoms and heart function were evaluated by questioning and physical examination; further examinations were performed according to decision of cardiac physician, including echocardiography, stress test even cardiac catheter.
Balanced technique with intravenous and/or inhalation anesthetics combined with opioids and the muscle relaxants was used for anesthetic induction and maintenance. In addition to the standard monitors, the direct arterial blood pressure monitor was used. Intra-operative fluid therapy was fulfilled with crystalloids, colloid, FFP and RBC. Intra-operative vasopressors were used if needed either in bolus or in continuous infusion.
Patients’ preoperative and intra-operative variables were prospectively collected. Postoperatively condition, troponin I, CKMB, myoglobin and BNP level, corresponding situation and resolution were collected until the patients discharged.
MI was defined as prognostic-relevant myocardial injury that occurs within once-administration-period after surgery, manifested by a typical increase in troponin I (≥ 0.04 ng/ml), performed with an electro-chemiluminescent immunoassay (Roche Diagnostics), excluding non-ischemia multi-factorial myocardial injury (e.g., underwent cardiovertion, sepsis or pulmonary embolism). [7] We did not routinely do troponin I measurement for all patients, but only for the patients who had risk factors before, events intra-operative, or symptoms and events after surgery, we hypothetically grouped those patients who had no troponin I measurement to patients without MI.
Myocardial infarction was defined as a typical increase in cardiac biomarker within once-administration-period after surgery and one or more of the following features: symptoms (such as pain of chest, shoulder or arm); ECG ischemia change (ST-segment elevation or depression, T-wave inversion, new left bundle branch block); development of pathologic Q wave; imaging evidence of new loss of visible myocardium or regional wall motion abnormality; Identification of intra-coronary thrombus by angiography or autopsy. [4].
The preoperative, intra-operative and postoperative variables were compared between patients with MI and without MI. The incidence of MI were calculated.
Large dose of vasopressor was defined as using more than two kinds of vasopressor. Infection was defined as fever and WBC ≥ 1.5 times normal upper limit.
All analyses were performed using the Statistical Package for the BMI version 23.0 (SPSS, Inc., Chicago, IL). All reported p values are two sided. The categorical data were analyzed with Pearson’s Chi-square test. Student’s t test or analysis of variance was used to compare the preoperative and intra-operative quantitative variables. The categorical variables were presented as percentages, and the quantitative variables were presented as mean ± standard deviation. The data which were not accord with Gaussian distribution or homoscedasticity were analyzed with nonparametric tests. The cutoff values that were used to divide the quantitative variables were selected by the median, mean, quartiles, or a clinical meaningful value. Variables with a statistically significant relationship to MI in univariate analysis were entered into multivariate logistic regression. Statistical significance was defined as P less than 0.05.
To make the result accurate, we ruled out the patients who had no troponin I measurement within once-administration-period after surgery, comparing the variables between patients with MI and patients with normal troponin I level.
Result
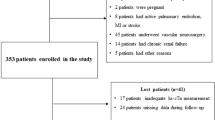
A total of 612 patients (≥ 65)underwent abdominal surgery (longer than 2 h) at Beijing Hospital, National Center of Gerontology between January 2016 and March 2017. After exclusion of 327 without troponin measurement within once-administration-period after surgery, 285 patients were included in the study. The Flow Chart see Fig. 1. The mean patient age was 72 years (range 65–90 years), with troponin I level range from 0.00 to 4.08 ng/ml.
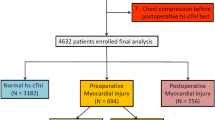
Among 612 patients studied, 285 patients (46.6%) had troponin I measurement within once-administration-period after surgery, 36 patients (12.6%) developed troponin I elevation, no patient had non-ischemia causes, while only two patients (0.7%) fulfilled definition of myocardial infarction. Most of troponin I, CKMB, Myoglobin and BNP peak appeared within the first 7 days after surgery, the profiles of troponin I and other relative biomarkers after surgery are shown in Fig. 2.
Results of the univariate analysis of the studied pre- and intra-operative variables between patients with MI and without MI are shown in Tables 1 and 2. Patients with MI had significantly higher incidence of CAD and infection before surgery compared with patients without MI. Many intra-operative variables were associated with MI in univariate analysis, such as laparoscopic/laparotomy surgery, gastrointestinal/hepatobiliary surgery, blood loss and anesthetic maintenance method, etc.
In multivariable analysis, CAD history, non-laparoscopic surgery, blood loss ≥ 800 ml, non-venous maintain, and infection were confirmed as independent risk factors of MI (Table 3). The risk factors had 2.1–5.2 fold increase odds ratio developing MI.
Results of postoperative outcomes comparing between patients with MI and without MI are shown in Table 4. MI were associated with longer hospital stay, more cardiac consultation, higher infection and reoperation rate, the patients with MI also had lower hemoglobin level and higher BUN, K, glucose level.
Meanwhile, the incidences of mainly outcomes were proportional to the troponin level, the higher of troponin I, more frequency of the outcomes.There was significant difference between troponin ≥ 0.04 ng/ml group and troponin ≥ 0.1 ng/ml group (P < 0.05). See Fig. 3.
Discussion
In our study, we confirmed that MI was common in elderly patients who underwent abdominal surgery (incidence 12.6%), while myocardial infarction was infrequence (incidence 0.7%). They had similar risk factors and both did harm to the prognosis of elderly patients [8]. Therefore, we should pay more attention not only to myocardial infarction patients but also to MI patients. Failure to monitor troponin measurements after surgery will result in missing most of the prognosis-relevant events.
The new universal definition of myocardial infarction highlights cardiac biomarkers [4, 9]. In our study, we found that 12.6% of our investigated population developed troponin I elevation within once-administration-period after surgery. Cardiac troponin I and T are components of the contractile apparatus of myocardial cells and are expressed almost exclusively in the heart [10]. Other biomarkers such as CKMB, myoglobin and BNP also have their clinical significance, we observed corresponding elevation of them in our study, although not that much speciality to MI like troponin [11,12,13]. Cardiac troponin elevation is still multi-factorial, including ischemia causes and non-ischemia causes, resulting from myocardial injury or other important organ injury [14, 15].
Non-ischemia causes include sepsis, pulmonary embolism, stroke, cardioversion, etc. According to the definition of myocardial injury after non-cardiac surgery, perioperative myocardial injuries due to a documented non-ischemic etiology should be excluded [7]. In our study, we found no non-ischemia cases, that is 100% of myocardial injury cases were ischemia related, which maybe because the limited sample size. Although experienced physicians investigated all elevated troponin I measurements to evaluate if there was evidence of a non-ischemic cause, it is still possible some non-ischemic etiologies were missed and that some events were not due to ischemic myocardial injury.
Previous studies, using troponin T as biomarker, showed that the elevation of an isolated cardiac biomarker or enzyme level during the first 3 days was an independent predictor of 30-day mortality [6, 7]. LeManach et al. [16] conducted a consecutive cohort study of 1136 patients undergoing abdominal aortic surgery in which they excluded non-ischemia patients, they demonstrated that an elevated troponin I after surgery was an independent predictor of in-hospital mortality. While our study evaluated all troponin I elevations within once-administration-period after surgery, and excluded troponin I-elevated cases related to non-ischemia, avoiding missing the delay-onset myocardial injury and observing that majority of myocardial injury cases are ischemia related. We demonstrated that whatever the reasons of troponin I elevation are, troponin I elevation is related to bad prognosis after surgery, deserving more attention and management.
In our study, we only did troponin I measurement for part of the patients who had risk factors before, intra-operative event, or symptoms and events after surgery, and we grouped those patients who had no troponin I measurement to patients without troponin I elevation, which might cause bias when calculated the incidence of MI. To make the result more accurate, we excluded the patients who had no troponin I measurement within once-administration-period after surgery, comparing the variables between patients with troponin I elevation and patients with normal troponin I level.
After abundant variable analysis, we identified CAD history, non-laparoscopic surgery, blood loss ≥ 800 ml, non-venous maintain, and infection as independent risk factors for troponin-I elevation. Patients who have history of CAD are more likely suffering cardiac complications under the stress of surgery, which has been established before [17]. There are more and more guidelines helping us to evaluate and manage cardiac diseases before surgery, making CAD a controllable medical history [18]. Preoperative extended evaluation and management should be made to patients with these risk factors, but intra-operative management seems more important than preoperative factors.
Laparoscopic surgery with minimal trauma puts less stress on patients, whereas laparotomy surgery with massive tissue injury gives large burden on patients’ important organs. The laparotomy surgery will five times increase MI incidence, which is similar with previous study [19, 20].
In the present study, we confirmed that blood loss ≥ 800 ml would triple the possibility of MI, pointing out that the more blood loss occurred, the more myocardial injury would happen, suggesting that blood loss should be kept to a minimum during the surgery [21].
Venous maintenance is commonly used during anesthesia, to avoid pollution, nowadays venous anesthetics are applied more frequency than inhalation anesthetics [22]. Although previous study has shown that sevoflurane has myocardial protect effect, [23] in our study, we observed that solely inhalation maintenance doubled MI incidence. The reason maybe combination remifentanil and propofol, effectively depressed the stress from surgical stimuli, decreased HR and cardiac oxygen consumption, therefore, prevented MI onset [24]. Further studies about balancing the advantage and disadvantage of inhalation anesthetics and venous anesthetics are needed.
Infection is the leading cause of mortality after surgery,[3] systemic inflammation reaction will do harm to important organs especially heart and kidney, added with increased HR, heart burdened a lot, almost five times increased MI incidence, controlling infection is of great importance [25].
In our study, we also observed that most of the troponin I elevation happened in the first 7 days after surgery, with other related biomarker accordingly elevated, but only small amount of patients (0.7%) suffering troponin I elevation experienced an ischemic symptom. Therefore, most of the troponin I elevation cases probably would have been missed without systematic biomarker monitoring after surgery. Moreover, the higher the troponin I level was, more frequently happened the bad outcomes. Because MI is common, hidden and leads to bad prognosis, clinical trials to establish strategies to prevent and treat this important complication were urgently needed. We recommend routinely monitoring perioperative troponin I measurements in elderly patients undergoing abdominal surgery, especially on the first 7 days after surgery for the high-risk population.
Our study has some limitations. First, this is a retrospective study, the question remains whether the risk factors identified in this study were surrogate markers of myocardial injury. In addition, the possibility of some other unmeasured confounding factors should be considered. Second, the results of our study were based on data from one center, while there are a variety of perioperative practices during surgery among different centers. Therefore, our results need to be confirmed by other centers. Further prospective studies designed to prevent and treat MI are warranted.
In conclusion, MI is common in elderly patients undergoing abdominal surgery, which has negative impact on prognosis. Perioperative troponin I evaluation in elderly patients, especially within the first 7 days after surgery, may aid in the risk stratification and prognostic assessment. Decreasing intra-operative blood loss, laparoscopic surgery, venousmaintenance anesthesia, control infection, and focus on patients with CAD may help preventing post-operative myocardial injury. Preventative medicine and effective management of MI need further investigation.
References
Priebe HJ (2000) The aged cardiovascular risk patient. Br J Anaesth 85:763–778
Johnston SD et al (2002) Cardiovascular morbidity and mortality after orthotopic liver transplantation. Transplantation 73:901–906
Fouad TR et al (2009) Prediction of cardiac complications after liver transplantation. Transplantation 87:763–770
Thygesen K et al (2012) Third universal definition of myocardial infarction. Circulation 126:2020–2035
Snipelisky D et al (2013) Cardiac troponin elevation predicts mortality in patients undergoing orthotopic liver transplantation. J Transplant 2013:252838
Biccard BM, Devereaux Pj Fau-Rodseth RN, Rodseth RN (2014) Cardiac biomarkers in the prediction of risk in the non-cardiac surgery setting. Anaesthesia 69:484–493
Botto F et al (2014) Myocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30-day outcomes. Anesthesiology 120:564–578
Hedge J, Balajibabu PR, Sivaraman T (2017) The patient with ischaemic heart disease undergoing non cardiac surgery. Indian J Anaesth 61:705–711
Mitka M (2012) New definition of myocardial infarction puts biomarkers front and center. JAMA 308:1511–1512
Arnadottir A, Falk Klein C, Iversen K (2017) Head-to-head comparison of cardiac troponin T and troponin I in patients without acute coronary syndrome: a systematic review. Biomarkers 22:701–708
Athamneh H, Basnawi A Fau-Siler-Fisher A, Siler-Fisher A (2013) CKMB and acute myocardial infarction in the emergency department. J Emerg Med 45:617–678
Hefler-Frischmuth K, Ohoo A et al (2017) Compartment syndrome after gynecologic laparoscopy: systematic review of the literature and establishment of normal values for postoperative serum creatine kinase and myoglobin levels. Arch Gynecol Obstet 296:285–293
Khanam SS et al (2017) Prognostic value of short-term follow-up BNP in hospitalized patients with heart failure. BMC Cardiovasc Disord 17:215.
Jaber S, Paugam-Burtz C (2013) Acute liver failure and elevated troponin-I: controversial results and significance? Crit Care 17:102
Siniscalchi A et al (2012) Postoperative troponin T elevation as a predictor of early acute kidney injury after orthotopic liver transplantation: a preliminary retrospective study. Transplant Proc 44:1999–2001
Le Manach Y et al (2005) Early and delayed myocardial infarction after abdominal aortic surgery. Anesthesiology 102:885–891
Yong CM et al (2010) Multivessel coronary artery disease predicts mortality, length of stay, and pressor requirements after liver transplantation. Liver Transpl 16:1242–1248
Fleisher La Fau-Beckman JA et al (2007) ACC/AHA 2007 guidelines on Perioperative Cardiovascular Evaluation and Care for Noncardiac Surgery: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery) Developed in Collaboration With the American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, and Society for Vascular Surgery. Circulation 116:1971–1996
Lu Z et al (2012) Cost-benefit analysis of laparoscopic surgery versus laparotomy for patients with endometrioid endometrial cancer: experience from an institute in China. J Obstet Gynaecol Res 38:1011–1017
Moehrlen U et al (2012) Immune cell populations and cytokine production in spleen and mesenteric lymph nodes after laparoscopic surgery versus conventional laparotomy in mice. Pediatr Surg Int 28:507–513
Kougias P et al (2017) Effect of postoperative anemia and baseline cardiac risk on serious adverse outcomes after major vascular interventions. J Vasc Surg 66:1836–1843
Herling SF et al (2017) Total intravenous anaesthesia versus inhalational anaesthesia for adults undergoing transabdominal robotic assisted laparoscopic surgery. Cochrane Database Syst Rev 4:CD011387
Heindl B et al (1999) Sevoflurane and isoflurane protect the reperfused guinea pig heart by reducing postischemic adhesion of polymorphonuclear neutrophils. Anesthesiology 91:521–530
Gimenes AM et al (2011) Effect of intravenous propofol and remifentanil on heart rate, blood pressure and nociceptive response in acepromazine premedicated dogs. Vet Anaesth Analg 38:54–62
Kolls JK (2017) Commentary: understanding the impact of infection, inflammation and their persistence in the pathogenesis of bronchopulmonary dysplasia. Front Med (Lausanne) 4:24
Acknowledgements
Support was provided solely from Beijing Hospital, National Center of Gerontology sources. Doctor Research Project. BJ-2015-102. This study was conducted at Beijing Hospital, National Center of Gerontology.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All authors have no conflict of interest to disclose.
Ethical approval
This retrospective study had been approved by the Beijing Hospital Institutional Review Board (2016BJYYEC-030-01).
Informed consent
For this kind of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Huang, S., Peng, W., Yang, N. et al. Myocardial injury in elderly patients after abdominal surgery. Aging Clin Exp Res 30, 1217–1223 (2018). https://doi.org/10.1007/s40520-018-0908-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-018-0908-y