Abstract
Background
Elevated cardiac biomarkers, such as high-sensitivity cardiac Troponin T and N-terminal pro-B-type natriuretic peptide improve the prediction of major adverse cardiac events. However, very few trials have investigated the association between perioperative cardiac injury and non-cardiac complications. The primary aim of this study was to determine the association between peri-operative myocardial injury and non-cardiac complications in patients undergoing vascular surgery. Additionally, the association between elevated pre-operative high-sensitivity cardiac Troponin T or N-terminal pro-B-type natriuretic peptide and non-cardiac complications was explored.
Methods
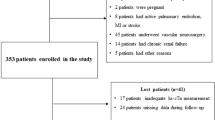
This study is a post hoc analysis of a multicentre randomised controlled trial. Patients were recruited from three centres in Sweden between 2016 and 2019. Cardiac troponin level was measured pre-operatively and at 4, 24, and 48 h after the start of surgery in patients undergoing vascular surgery. N-terminal pro-B-type natriuretic peptide was measured pre-operatively. The primary outcome was a composite of major postoperative non-cardiac complications assessed at 30 days.
Results
A total of 184 patients undergoing peripheral or aortic vascular surgery were included in this study. The primary endpoint occurred in 67 (36%) patients. Perioperative myocardial injury was significantly associated with non-cardiac complications, with an adjusted odds ratio (OR) of 2.71 (95% confidence interval 1.33–5.55, P = 0.01). Sensitivity and specificity were 0.40 and 0.81, respectively. No association was found between pre-operative hs-cTnT or NT-proBNP and non-cardiac complications.
Conclusion
In this pilot study, we found that new peri-operative myocardial injury is associated with an increased risk of non-cardiac complications within 30 days after index surgery in patients undergoing vascular surgery. Pre-operative high-sensitivity cardiac Troponin T or N-terminal pro-B-type natriuretic peptide did not appear to predict non-cardiac complications. Larger studies are needed to confirm our findings.
Trial registration
EudraCT database: 2016-001584-36
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Pre-operative risk assessment tools are recommended to identify patients who are at high risk of peri-operative complications (Wanhainen et al. 2019; Kolh et al. 2016). Pre-operative risk assessment before non-cardiac surgery has recently been evaluated using biomarkers. Elevated pre-operative N-terminal pro-B type natriuretic peptide (NT-proBNP) and high-sensitivity cardiac Troponin T (hs-cTnT) have been associated with increased postoperative mortality (De Hert and Lurati Buse 2020; Puelacher et al. 2018). Peri-operative myocardial injury (PMI) is associated with increased mortality and adverse cardiovascular outcomes (Puelacher et al. 2018; Devereaux et al. 2017; Thygesen et al. 2018; Chew et al. 2023). Several studies have explored the association between PMI and postoperative cardiac complications and their use for perioperative risk assessment is now recommended in the current guidelines (Halvorsen et al. 2022).
Morbidity and mortality associated with postoperative major adverse cardiac events are similar to postoperative major adverse non-cardiac events (Beattie et al. 2018). However, comparatively few have studied the association between PMI and non-cardiac complications (NCC). One large cohort study showed an association between PMI and non-cardiovascular death (Devereaux et al. 2012). Noordzij et al. found an association between a 100 % postoperative increase in troponin and NCC (Noordzij et al. 2015). Patients undergoing vascular surgery have a higher risk of postoperative complications including NCC compared to other surgical cohorts, due to associated comorbidities (Healey et al. 2002). Furthermore, it has been shown that pneumonia and bleeding have the highest impact on clinical outcomes after vascular, abdominal or lower extremity surgery (Bennett et al. 2017). The primary aim of the present study was to determine the association between peri-operative myocardial injury and non-cardiac complications in patients undergoing vascular surgery. We also explored the association between pre-operative elevated cardiac biomarkers, hs-cTnT or NT-proBNP and NCC.
Methods
This study is a post hoc analysis of data from our previously published study (Valadkhani et al. 2022), which was a prospective, multicentre, single-blinded, randomised clinical pilot trial. The study was approved by the Medical Drug Protection Agency in Uppsala, Sweden, (registration number: 5.1-2016-30176). Ethical approval for this study (registration number: 2014/310/1-3) was provided by the Swedish Ethical Review Authority, Uppsala, Sweden (Chairperson Per-Erik Nistér) on 27 August 2014. It was also registered in the EudraCT database: 2016-001584-36.
Patients and study procedure
Patients > 60 years of age undergoing peripheral vascular or aortic surgery and without communication or cognitive difficulties were included in the study. The exclusion criteria were chronic obstructive pulmonary disease (COPD), other lung diseases that result in a patient requiring supplemental oxygen at rest, arterio-venous fistula surgery, carotid surgery or being enrolled in other clinical trials. Written informed consent was obtained from patients deemed eligible from three centres in Sweden: Karolinska University Hospital Stockholm, University Hospital, Linköping and Central Hospital, Karlstad. Recruitment started in November 2016 and was concluded in November 2019.
Randomisation was accomplished by inserting computer-generated random numbers in opaque and sealed envelopes, designated to each site. Patients were randomised in a 1:1 ratio to Group Normoxia (FiO2 = 0.21 and SpO2 target > 90%) and Group Hyperoxia (FiO2 = 0.50 and SpO2 target > 98%). Patients, surgeons assessing complications, and biochemical analysts were blinded to group allocation. Biomarkers including NT-proBNP and hs-cTnT were acquired before surgery (on the day of the index surgery) and 4, 24, and 48 h after the start of surgery. These biomarkers were measured using Cobas Immunoanalyser, Roche Diagnostics, Rotkreutz, Switzerland. Postoperative complications within 30 days were registered in medical records by surgeons and later validated by one of the authors.
Outcome and definitions
The primary outcome was non-cardiac complications (NCC) occurring within 30 days after index surgery. A NCC was defined as one or more complications included in the clusters presented in Table 1.
Non-cardiac complications (NCC)
Peri-operative myocardial injury (PMI)
PMI was defined as either acute PMI or acute chronic PMI, as defined below.
Acute PMI
Normal hs-cTnT values pre-operatively and postoperative increase by > 14 ng l−1 (Thygesen et al. 2018).
Chronic PMI
Pre-operative hs-cTnT > 14 ng l−1 and postoperative hs-cTnT < 14 ng l−1 (Puelacher et al. 2018).
Acute on chronic PMI
Pre-operative hs-cTnT > 14 ng l−1 and an increase in postoperative hs-cTnT by ≥ 14 ng l−1 from the pre-operative value (Puelacher et al. 2018).
Statistics
Patients were grouped by whether they had a non-cardiac complication or not. Categorical values are presented as numbers and percentages. Continuous variables are presented as median and interquartile range (IQR). P values were calculated using Mann-Whitney U test and chi-squared test as appropriate. The association between pre-operative hs-cTnT and NT-proBNP NCC was assessed using generalised linear regression with binomial family. Since the outcome of this post hoc analysis was altered compared to the original study and did not include cardiac complications, we chose to use multiple regression to adjust for oxygen or air. Further adjustments were made using multiple regression to account for the difference in endovascular surgery and duration of operation between the groups with and without NCC. Generalised estimating equation (GEE) regression models were used to account for the statistical correlation of the repeated measurement of hs-cTnT when estimating the association between PMI and NCC, in patients where hs-cTnT was available. The GEE model was further adjusted for air or oxygen therapy, endovascular surgery and duration of operation. Based on the fitted model, sensitivity and specificity were estimated. A GEE model was used to account for which cluster of complications most strongly accounted for the association between PMI and NCC. Multiple regression was used to compare the association between PMI and NCC with the association between body mass index (BMI), duration of operation, American Society of Anaesthesiologists (ASA) score and intra-operative haemorrhage > 500 ml, as independent variables, and NCC. P values < 0.05 were considered statistically significant. All analyses were conducted using R version 4.1.2 (R Core Team (2021). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria)
Results
In total, 184 patients were included in this study. The patient characteristics are presented in Table 2. There was a statistically significant difference between the groups with no NCC and NCC in patients undergoing endovascular surgery vs. non-endovascular surgery (39 % vs. 24 %, P = 0.049) and in the duration of operation (155 min vs. 230 min, p < 0.001), see Table 2.
In two patients, no pre-operative hs-cTnT was obtained while one had no postoperative hs-cTnT. A statistically significant association was found between peri-operative myocardial injury (PMI) and NCC at 30 days after index surgery with an adjusted OR of 2.71 (95 % CI 1.33–5.52, P = 0.01). Sensitivity and specificity were 0.32 and 0.87 respectively. The incidence of complications in each cluster, other than death, is shown in Table 3. One patient in the NCC group died within 30 days after index surgery. When comparing different clusters, PMI was most strongly associated with renal complications (P = 0.03).
Pre-operative hs-cTnT and NT-proBNP were missing in two and three patients respectively. These patients were excluded from the regression models. The association between clinical characteristics and non-cardiac complications are shown in Table 4. No association was found between pre-operative hs-cTnT or NT-proBNP and NCC. A significant association was found between duration of surgery > 120 min and NCC, with an OR of 3.33 (95 % CI 1.17–9.47, P = 0.02).
Discussion
We found an association between peri-operative myocardial injury (PMI) and the subsequent occurrence of a non-cardiac complication (NCC) in patients undergoing vascular surgery. However, we found no association between increased pre-operative hs-cTnT or NT-proBNP and NCC.
The definition of PMI varies depending on the thresholds used (Puelacher et al. 2018; Devereaux et al. 2017). It is important to distinguish between patients with chronic PMI. and those with acute on chronic PMI. This distinction is important since patients with an acute on chronic PMI have a higher mortality compared to those with a chronic PMI (Puelacher et al. 2018). Furthermore, this distinction was important in our patients undergoing vascular surgery since up to 40% had an elevated pre-operative hs-cTnT > 14 ng l−1(Valadkhani et al. 2022).
Compared to trials that have studied the association between PMI and cardiac complications there is a scarcity of trials that have addressed the association between PMI and NCC (Chew et al. 2023). Noordzij et al. studied patients undergoing abdominal surgery and found that an increase in hs-cTnT by 100% between pre-and postoperative values was associated with NCC(11). However, they could not demonstrate an association between elevated pre-operative hs-cTnT and NCC, which was similar to our finding. The sensitivity and specificity were also similar to our results, albeit in patients undergoing abdominal surgery (Noordzij et al. 2015). In a recent study, the authors found an association between PMI and NCC in patients undergoing non-cardiac surgery. However, they did not distinguish between chronic PMI and acute chronic PMI, which is problematic (Ackland et al. 2020). It is important to stress that patients with PMI who have an NCC postoperatively also have higher mortality compared with those who have NCC alone (Beattie et al. 2018; Ackland et al. 2020). Therefore, the detection of PMI may contribute to the prognostication of postoperative mortality.
Our findings also show that PMI was most strongly associated with the cluster of renal complications, which was similar to the findings of Ackland et al. (2020). Previous studies indicate that patients with acute kidney injury can have an acute rise in troponin that may be mistaken for PMI (Banerjee et al. 2019). However, hypotension and sepsis may also cause acute kidney injury so it is possible to have a simultaneous acute kidney injury and PMI (Halvorsen et al. 2022; Banerjee et al. 2019). Despite statistical significance, the absolute number of patients who had renal complications in our study was small and therefore this finding should be interpreted cautiously.
There is no simple physiological explanation for the association between PMI and NCC since PMI is multifactorial (Halvorsen et al. 2022). If PMI occurs following a cardiac event (e.g., arrhythmia, demand-perfusion mismatch), it is possible that perfusion to other organs might be affected, which may in turn lead to NCC. In contrast, non-cardiac causes of PMI such as sepsis or pulmonary embolism might lead to an NCC. Therefore, several distinct pathways may explain how PMI leads to NCC. The temporal relationship between peri-operative PMI and NCC could suggest that PMI increases the risk of NCC. However, it is also possible that both PMI and NCC occur independently as a consequence of an intra-operative event such as hypotension (Sessler et al. 2019).
Recent guidelines have concluded that elevated pre-operative NT-proBNP is associated with significantly increased postoperative mortality (Halvorsen et al. 2022). Furthermore, it is also associated with cardiac complications (Karthikeyan et al. 2009). However, the association between NT-proBNP and NCC remains unexplored, to the best of our knowledge. In addition to the above cardiac markers, other factors such as American Society of Anaesthesiology Physical status, intra-operative blood loss and duration of surgery have been shown to be associated with postoperative complications (Glance et al. 2011; Cheng et al. 2018; Hopkins et al. 2016). In our study, the odds ratio for PMI was greater than all the other factors known to be associated with postoperative complications, except the duration of surgery.
This study has several strengths. It is based on a prospective, multicentre randomised controlled trial with blinded outcomes registered by surgeons. Moreover, we have biomarker data collected both before and after surgery whereby acute, chronic and acute on chronic PMI could be clearly differentiated. This study also focuses on a cohort of patients undergoing vascular surgery who are at high risk of developing postoperative complications (Healey et al. 2002). Finally, the definition of PMI used in this study is the same as recommended in current guidelines and differentiates between acute and acute on chronic PMI. There are some limitations to our conclusions, based on sample size and methodological issues. It is a relatively small study and is based on secondary analysis of data, which could introduce unknown bias. Additionally, we did not attain 48-h hs-cTnT in all patients since some were discharged earlier. A further weakness of this study is the absence of high-resolution intra-operative hemodynamic data that may give a better insight into the aetiology of PMI.
In conclusion, we found an association between PMI and non-cardiac complications within 30 days after index surgery in patients undergoing vascular surgery. This strengthens the importance of troponin measurement in the pre- and postoperative period since it can be used to assess the risk of developing non-cardiac complications after vascular surgery. The physiological causal relationship between PMI and NCC remains unclear and is likely to be multifactorial.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to the risk of compromising patient privacy but are available from the corresponding author on reasonable request.
Abbreviations
- POSSUM:
-
Portsmouth-Physiological and Operative Severity Score for the enUmeration of Mortality and morbidity
- RCRI:
-
Revised Cardiac Risk Index
- MACE:
-
Major adverse cardiac events
- NT-proBNP:
-
N-terminal pro-B type natriuretic peptide
- PMI:
-
Peri-operative myocardial injury
- NCC:
-
Non-cardiac complications
- hs-cTnT:
-
High-sensitivity cardiac Troponin T
- COPD:
-
Chronic obstructive pulmonary disease
- IQR:
-
Interquartile range
- GEE:
-
Generalised estimating equation
- BMI:
-
Body mass index
- ASA:
-
American Society of Anaesthesiologists
References
Ackland GL, Abbott TEF, Jones TF, Leuwer M, Pearse RM, Niebrzegowska E, et al. Early elevation in plasma high-sensitivity troponin T and morbidity after elective noncardiac surgery: prospective multicentre observational cohort study. Br J Anaesth. 2020;124(5):535–43.
Banerjee D, Perrett C, Banerjee A. Troponins, Acute coronary syndrome and renal disease: from acute kidney injury through end-stage kidney disease. European Cardiology Review. 2019;14(3):187.
Beattie WS, Wijeysundera DN, Chan MTV, Peyton PJ, Leslie K, Paech MJ, et al. Implication of major adverse postoperative events and myocardial injury on disability and survival: a planned subanalysis of the ENIGMA-II trial. Anesth Analg. 2018;127(5):1118–26.
Bennett KM, Kent KC, Schumacher J, Greenberg CC, Scarborough JE. Targeting the most important complications in vascular surgery. J Vasc Surg. 2017;65(3):793–803.
Boustani M, Rudolph J, Shaughnessy M, Gruber-Baldini A, Alici Y, Arora RC, et al. The DSM-5 criteria, level of arousal and delirium diagnosis: inclusiveness is safer. BMC Med. 2014;12(1).
Cheng H, Clymer JW, Po-Han Chen B, Sadeghirad PDB, Ferko NC, Cameron CG, et al. Prolonged operative duration is associated with complications: a systematic review and meta-analysis. J Surg Res. 2018;229:134–44.
Chew MS, Saugel B, Lurati-Buse G. Perioperative troponin surveillance in major noncardiac surgery: a narrative review. Br J Anaesth. 2023;130(1):21–8.
De Hert SG, Lurati Buse GA. Cardiac biomarkers for the prediction and detection of adverse cardiac events after noncardiac surgery: a narrative review. Anesth Analg. 2020;131(1):187–95.
Devereaux PJ, Chan MTV, Alonso-Coello P, Walsh M, Berwanger O, Villar JC, et al. Association between postoperative troponin levels and 30-day mortality among patients undergoing noncardiac surgery. JAMA. 2012;307(21):2295–304.
Devereaux PJ, Biccard BM, Sigamani A, Xavier D, Chan MTV, Srinathan SK, et al. Association of postoperative high-sensitivity troponin levels with myocardial injury and 30-day mortality among patients undergoing noncardiac surgery. JAMA - Journal of the American Medical Association. 2017;317(16):1642–51.
Glance LG, Dick AW, Mukamel DB, Fleming FJ, Zollo RA, Wissler R, et al. Association between intraoperative blood transfusion and mortality and morbidity in patients undergoing noncardiac surgery. Anesthesiology. 2011;114(2):283–92.
Halvorsen S, Mehilli J, Cassese S, Hall TS, Abdelhamid M, Barbato E, et al. 2022 ESC Guidelines on cardiovascular assessment and management of patients undergoing non-cardiac surgery developed by the task force for cardiovascular assessment and management of patients undergoing non-cardiac surgery of the European Society of Cardiology (ESC) Endorsed by the European Society of Anaesthesiology and Intensive Care (ESAIC). Eur Heart J. 2022;43(39):3826–924.
Healey MA, Shackford SR, Osler TM, Rogers FB, Burns E. Complications in surgical patients. Arch Surg. 2002;137(5):611–8.
Hopkins TJ, Raghunathan K, Barbeito A, Cooter M, Stafford-Smith M, Schroeder R, et al. Associations between ASA Physical Status and postoperative mortality at 48 h: a contemporary dataset analysis compared to a historical cohort. Perioperative Medicine. 2016;5(1):1–6.
Karthikeyan G, Moncur RA, Levine O, Heels-Ansdell D, Chan MTV, Alonso-Coello P, et al. Is a pre-operative brain natriuretic peptide or N-terminal pro-B-type natriuretic peptide measurement an independent predictor of adverse cardiovascular outcomes within 30 days of noncardiac surgery? A systematic review and meta-analysis of observational studies. J Am Coll Cardiol. 2009;54(17):1599–606.
Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120(4).
Kolh P, de Hert S, de Rango P. The concept of risk assessment and being unfit for surgery. Eur J Vasc Endovasc Surg. 2016;51(6):857–66.
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for Prevention of Surgical Site Infection, 1999. Am J Infect Control. 1999;27(2):97–134.
Noordzij PG, Van Geffen O, Dijkstra IM, Boerma D, Meinders AJ, Rettig TCD, et al. High-sensitive cardiac troponin T measurements in prediction of non-cardiac complications after major abdominal surgery. BJA: British Journal of Anaesthesia. 2015;114(6):909–18.
Puelacher C, Buse GL, Seeberger D, Sazgary L, Marbot S, Lampart A, et al. Perioperative myocardial injury after noncardiac surgery incidence, mortality, and characterization. Circulation. 2018;137(12):1221–32.
Sessler DI, Bloomstone JA, Aronson S, Berry C, Gan TJ, Kellum JA, et al. Perioperative Quality Initiative consensus statement on intraoperative blood pressure, risk and outcomes for elective surgery. Br J Anaesth. 2019;122(5):563–74.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth Universal Definition of Myocardial Infarction (2018). Circulation. 2018;138(20):e618–51.
Valadkhani A, Henningsson R, Nordström JL, Granström A, Hallqvist L, Wahlgren CM, et al. Postoperative complications and myocardial injury in patients receiving air or oxygen. Prospective, randomised and pilot study. Acta Anaesthesiol Scand. 2022;66(10):1185–92.
Wanhainen A, Verzini F, Van Herzeele I, Allaire E, Bown M, Cohnert T, et al. Editor’s Choice e European Society for Vascular Surgery (ESVS) 2019 Clinical Practice Guidelines on the Management of Abdominal Aorto-iliac Artery Aneurysms. Eur J Vasc Endovasc Surg. 2019;57:8–93.
Acknowledgements
We would like to thank Henrike Häbel, biostatistician at Karolinska Institute, Stockholm.
Funding
Open access funding provided by Karolinska Institute. Funding was ascertained from Centrum för klinisk forskning, Region Varmland, Sweden and Nyckel fond, Örebro University Hospital, Sweden. The funders had no specific role in the conceptualization, design, data collection, analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors were involved in the conception, design, acquisition, analysis, interpretation of data and drafted the work or substantively revised it. All authors approve the submitted version. All authors agreed both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Medical Drug Protection Agency in Uppsala, Sweden, (registration number: 5.1-2016-30176). Ethical approval for this study (registration number: 2014/310/1-3) was provided by The Swedish Ethical Review Authority, Uppsala, Sweden (Chairperson Per-Erik Nistér) on 27 August 2014.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Valadkhani, A., Gupta, A. & Bell, M. Perioperative myocardial injury is associated with increased postoperative non-cardiac complications in patients undergoing vascular surgery: a post hoc analysis of a randomised clinical pilot trial. Perioper Med 12, 58 (2023). https://doi.org/10.1186/s13741-023-00350-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13741-023-00350-y