Abstract
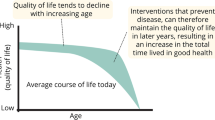
Herpes zoster is a frequent painful infectious disease whose incidence and severity increase with age. In older people, there is a strong bidirectional link between herpes zoster and functional decline, which refers to a decrement in ability to perform activities of daily living due to ageing and disabilities. However, the exact nature of such link remains poorly established. Based on the opinion from a multidisciplinary group of experts, we here propose a new model to account for the interplay between infection, somatic/psychiatric comorbidity, coping skills, polypharmacy, and age, which may account for the functional decline related to herpes zoster in older patients. This model integrates the risk of decompensation of underlying disease; the risk of pain becoming chronic (e.g. postherpetic neuralgia); the risk of herpes zoster non-pain complications; the detrimental impact of herpes zoster on quality of life, functioning, and mood; the therapeutic difficulties due to multimorbidity, polypharmacy, and ageing; and the role of stressful life events in the infection itself and comorbid depression. This model underlines the importance of early treatment, strengthening coping, and vaccine prevention.


Similar content being viewed by others
References
Yawn BP, Saddier P, Wollan PC et al (2007) A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc 82:1341–1349
Clinical Epidemiology and Health Services Evaluation Unit, Melbourne Health. Commissioned on behalf of the Australian Health Ministers’ Advisory Council (AHMAC) by the AHMAC Care of Older Australian Working Group (2004) Best practice approaches to minimise functional decline in the older person across the acute, sub-acute and residential aged care settings. Victorian Government Department of Human Services, Melbourne
Haut Conseil de la Santé Publique (2013) Vaccination des adultes contre le zona—Place du vaccin Zostavax®. Collection Avis et Rapport, Paris
Loeb M, McGeer A, McArthur M et al (1999) Risk factors for pneumonia and other lower respiratory tract infections in elderly residents of long-term care facilities. Arch Intern Med 159:2058–2064
Büla CJ, Ghilardi G, Wietlisbach V et al (2004) Infections and functional impairment in nursing home residents: a reciprocal relationship. J Am Geriatr Soc 52:700–706
Mody L, Sun R, Bradley SF (2006) Assessment of pneumonia in older adults: effect of functional status. J Am Geriatr Soc 54:1062–1067
Chen TY, Anderson DJ, Chopra T et al (2010) Poor functional status is an independent predictor of surgical site infections due to methicillin-resistant Staphylococcus aureus in older adults. J Am Geriatr Soc 58:527–532
Caljouwn MA, Kruijdenberg SJ, de Craen AJ et al (2013) Clinically diagnosed infections predict disability in activities of daily living among the oldest-old in the general population: the Leiden 85-plus Study. Age Ageing 42:482–488
Torres OH, Muñoz J, Ruiz D et al (2004) Outcome predictors of pneumonia in elderly patients: importance of functional assessment. J Am Geriatr Soc 52:1603–1609
Murcia J, Llorens P, Sánchez-Payá J et al (2010) Functional status determined by Barthel index predicts community acquired pneumonia mortality in general population. J Infect 61:458–464
Eurostat—European Commission (2013) European social statistics, 2013th edn. Eurostat Pocketbooks, Luxembourg
World Health Organisation Europe (2002) Active aging: a policy framework. World Health Organization, Geneva
Gil-Prieto R, San-Martín M, Álvaro-Meca A et al (2011) Herpes zoster hospitalizations of patients with chronic illnesses in Spain, 1998–2004. Vacunas 12:95–101
Blein C, Gavazzi G, Paccalin M et al (2013) Evaluation of the Herpes Zoster impact as comorbidity factor in 5 pathologies French hospital care among adults aged 50 and older. Value Health 16:A503
Schmader K (1999) Herpes zoster in the elderly: issues related to geriatrics. Clin Infect Dis 28:736–739
Ho JD, Xirasagar S, Lin HC (2011) Increased risk of a cancer diagnosis after herpes zoster ophthalmicus: a nationwide population-based study. Ophthalmology 118:1076–1081
Iglar K, Kopp A, Glazier RH (2013) Herpes zoster as a marker of underlying malignancy. Open Med 7:e68–e73
Drolet M, Brisson M, Schmader K et al (2010) Predictors of postherpetic neuralgia among patients with herpes zoster: a prospective study. J Pain 11:1211–1221
Drolet M, Brisson M, Schmader KE et al (2010) The impact of herpes zoster and postherpetic neuralgia on health-related quality of life: a prospective study. CMAJ 182:1731–1736
Schmader K, Gnann JW Jr, Watson CP (2008) The epidemiological, clinical, and pathological rationale for the herpes zoster vaccine. J Infect Dis 197:S207–S215
Wood M (2002) Understanding pain in herpes zoster: an essential for optimizing treatment. J Infect Dis 186:S78–S82
Benbernou A, Drolet M, Levin MJ et al (2011) Association between prodromal pain and the severity of acute herpes zoster and utilization of health care resources. Eur J Pain 15:1100–1106
Ghatak NR, Zimmerman HM (1973) Spinal ganglion in herpes zoster. A light and electron microscopic study. Arch Pathol 95:411–415
Zak-Prelich M, McKenzie RC, Sysa-Jedrzejowska A et al (2003) Local immune responses and systemic cytokine responses in zoster: relationship to the development of postherpetic neuralgia. Clin Exp Immunol 131:318–323
Johnson RW, Bouhassira D, Kassianos G et al (2010) The impact of herpes zoster and post-herpetic neuralgia on quality-of-life. BMC Med 8:37
Bouhassira D, Chassany O, Gaillat J et al (2012) Patient perspective on herpes zoster and its complications: an observational prospective study in patients aged over 50 years in general practice. Pain 153:342–349
Katz J, Melzack R (1999) Measurement of pain. Surg Clin North Am 79:231–252
Katz J, Cooper EM, Walther RR et al (2004) Acute pain in herpes zoster and its impact on health-related quality of life. Clin Infect Dis 39:342–348
Coplan PM, Schmader K, Nikas A et al (2004) Development of a measure of the burden of pain due to herpes zoster and postherpetic neuralgia for prevention trials: adaptation of the brief pain inventory. J Pain 5:344–356
Duracinsky M, Paccalin M, Gavazzi G et al (2014) ARIZONA study: is the risk of post-herpetic neuralgia and its burden increased in the most elderly patients? BMC Infect Dis 14:529
Hope-Simpson RE (1975) Postherpetic neuralgia. J R Coll Gen Pract 25:571–575
Higa K, Mori M, Hirata K et al (1997) Severity of skin lesions of herpes zoster at the worst phase rather than age and involved region most influences the duration of acute herpetic pain. Pain 69:245–253
Opstelten W, Zuithoff NP, van Essen GA et al (2007) Predicting postherpetic neuralgia in elderly primary care patients with herpes zoster: prospective prognostic study. Pain 132:S52–S59
Drolet M, Brisson M, Levin MJ et al (2010) A prospective study of herpes zoster severity of illness. Clin J Pain 26:656–666
Quinlivan ML, Ayres K, Ran H et al (2007) Effect of viral load on the outcome of herpes zoster. J Clin Microbiol 45:3909–3914
Scott FT, Leedham-Green ME, Barrett-Muir WY et al (2003) A study of shingles and the development of postherpetic neuralgia in East London. J Med Virol 70:S24–S30
Quinlivan ML, Ayres KL, Kelly PJ et al (2011) Persistence of varicella-zoster virus viraemia in patients with herpes zoster. J Clin Virol 50:130–135
Mahalingam R, Wellish M, Brucklier J et al (1995) Persistence of varicella-zoster virus DNA in elderly patients with postherpetic neuralgia. J Neurovirol 1:130–133
Li Q, Chen N, Yang J et al (2009) Antiviral treatment for preventing postherpetic neuralgia. Cochrane Database Syst Rev 15:CD006866
Rabaud C, Rogeaux O, Launay O et al (2013) Early antiviral treatment fails to completely prevent herpes-related pain. Med Mal 43:461–466
Attal N, Fermanian C, Fermanian J et al (2008) Neuropathic pain: are there distinct subtypes depending on the aetiology or anatomical lesion? Pain 138:343–353
Torrance N, Smith BH, Bennett MI et al (2006) The epidemiology of chronic pain of predominantly neuropathic origin. Results from a general population survey. J Pain 7:281–289
Bouhassira D, Lantéri-Minet M, Attal N et al (2008) Prevalence of chronic pain with neuropathic characteristics in the general population. Pain 136:380–387
Hoffman DL, Sadosky A, Dukes EM et al (2010) How do changes in pain severity levels correspond to changes in health status and function in patients with painful diabetic peripheral neuropathy? Pain 149:194–201
Attal N, Lanteri-Minet M, Laurent B et al (2011) The specific disease burden of neuropathic pain: results of a French nationwide survey. Pain 152:2836–2843
Gormsen L, Rosenberg R, Bach FW et al (2010) Depression, anxiety, health-related quality of life and pain in patients with chronic fibromyalgia and neuropathic pain. Eur J Pain 14:127
Radat F, Margot-Duclot A, Attal N (2013) Psychiatric co-morbidities in patients with chronic peripheral neuropathic pain: a multicentre cohort study. Eur J Pain 17:1547–1557
McCracken LM, Iverson GL (2001) Predicting complaints of impaired cognitive functioning in patients with chronic pain. J Pain Symptom Manage 21:392–396
Baliki MN, Geha PY, Apkarian AV et al (2008) Beyond feeling: chronic pain hurts the brain, disrupting the default-mode network dynamics. J Neurosci 28:1398–1403
Pickering G, Leplege A (2011) Herpes zoster pain, postherpetic neuralgia, and quality of life in the elderly. Pain Pract 11:397–402
Chidiac C, Bruxelle J, Daures JP et al (2001) Characteristics of patients with herpes zoster on presentation to practitioners in France. Clin Infect Dis 33:62–69
Dworkin RH, Johnson RW, Breuer J et al (2007) Recommendations for the management of herpes zoster. Clin Infect Dis 44:S1–S26
Oxman MN, Levin MJ, Johnson GR et al (2005) A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. N Engl J Med 352:2271–2284
Volpi A (2007) Severe complications of herpes zoster. Herpes 14:35–39
Liesegang TJ (2008) Herpes zoster ophthalmicus natural history, risk factors, clinical presentation, and morbidity. Ophthalmology 115:S3–S12
O’Connor KM, Paauw DS (2013) Herpes zoster. Med Clin North Am 97:503–522
Rousseau A, Bourcier T, Colin J, Labetoulle M (2013) Herpes zoster ophthalmicus-diagnosis and management. US Ophthal Rev 6:119–124
Yawn BP, Wollan PC, St Sauver JL et al (2013) Herpes Zoster eye complications: rates and trends. Mayo Clin Proc 88:562–570
Novotný J (2006) Specific issues in pharmacotherapy of the elderly. J Health Sci Manag Public Health 7:81–93
Schuling J, Gebben H, Veehof LJ et al (2012) Deprescribing medication in very elderly patients with multimorbidity: the view of Dutch GPs. A qualitative study. BMC Fam Pract 13:56
Frazier SC (2005) Health outcomes and polypharmacy in elderly individuals: an integrated literature review. J Gerontol Nurs 31:4–11
Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society (2011) Summary of the updated American geriatrics society/British geriatrics society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc 59:148–157
Attal N, Cruccu G, Baron R et al (2010) EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol 17:1113, e88
Johnson RW, Rice AS (2014) Clinical practice. Postherpetic neuralgia. N Engl J Med 371:1526–1533
Laurent B, Vicaut E, Leplege A et al (2014) Prevalence and quality of life impact of postherpetic neuralgia (PHN) in French medical centers specialized in chronic pain management: the ZOCAD study. Med Mal Infect 44:515–524
Bruckenthal P, Barkin RL (2013) Options for treating postherpetic neuralgia in the medically complicated patient. Ther Clin Risk Manag 9:329–340
Pickering G (2014) Antiepileptics for post-herpetic neuralgia in the elderly: current and future prospects. Drugs Aging 31:653–660
Pickering G, Pereira B, Clère F et al (2014) Cognitive function in older patients with postherpetic neuralgia. Pain Pract 14:E1–E7
Graham JE, Christian LM, Kiecolt-Glaser JK (2006) Stress, age, and immune function: toward a lifespan approach. J Behav Med 29:389–400
Schmader K, George LK, Burchett BM et al (1998) Race and stress in the incidence of herpes zoster in older adults. J Am Geriatr Soc 46:973–977
Schmader K, Studenski S, MacMillan J et al (1990) Are stressful life events risk factors for herpes zoster? J Am Geriatr Soc 38:1188–1194
Lasserre A, Blaizeau F, Gorwood P et al (2012) Herpes zoster: family history and psychological stress—case–control study. J Clin Virol 55:153–157
Harpaz R, Leung JW, Brown CJ et al (2015) Psychological stress as a trigger for herpes zoster: might the conventional wisdom be wrong? Clin Infect Dis 60:781–785
Irwin MR, Levin MJ, Carrillo C et al (2011) Major depressive disorder and immunity to varicella-zoster virus in the elderly. Brain Behav Immun 25:759–766
Irwin M, Costlow C, Williams H et al (1998) Cellular immunity to varicella-zoster virus in patients with major depression. J Infect Dis 178:S104–S108
Volpi A, Gatti A, Serafini G et al (2007) Clinical and psychosocial correlates of acute pain in herpes zoster. J Clin Virol 38:275–279
Gorwood P (2004) The generalized anxiety disorder and major depressive disorder comorbidity: an example of genetic pleiotropy? Eur Psychiatry 19:27–33
Kendler KS, Gardner CO, Prescott CA (2002) Toward a comprehensive developmental model for major depression in women. Am J Psychiatry 159:1133–1145
Vlaeyen JW, Linton SJ (2000) Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain 85:317–332
Sutor B, Rummans TA, Jowsey SG et al (1998) Major depression in medically ill patients. Mayo Clin Proc 73:329–337
Jiang W, Krishnan RR, O’Connor CM (2002) Depression and heart disease: evidence of a link, and its therapeutic implications. CNS Drugs 16:111–127
Millan MJ, Agid Y, Brüne M et al (2012) Cognitive dysfunction in psychiatric disorders: characteristics, causes and the quest for improved therapy. Nat Rev Drug Discov 11:141–168
Moussavi S, Chatterji S, Verdes E et al (2007) Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 370:851–858
Clarke DM, Currie KC (2009) Depression, anxiety and their relationship with chronic diseases: a review of the epidemiology, risk and treatment evidence. Med J Aust 190:S54–S60
Lin EH, Katon W, Von Korff M et al (2004) Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care 27:2154–2160
Hébert R (1997) Functional decline in old age. CMAJ 157:1037–1045
Acknowledgments
The authors are extremely grateful to Karine Bloch, Charles Baptiste, and Isabelle Bertrand (Sanofi Pasteur MSD) for their assistance in preparing the meeting. They also thank Fabienne Péretz (Abelia Science) for her assistance (supported by Sanofi Pasteur MSD) in preparing the manuscript.
Author information
Authors and Affiliations
Consortia
Ethics declarations
Conflict of interest
The authors declared that they have received within the past 5 years the following: NA: Reimbursement and fees for advisory boards or speakers from Pfizer, Lilly, Sanofi Pasteur, Sanofi Pasteur MSD, Grunenthal, Adir, Astra Zeneca, Astellas. CD: Reimbursement and fees for advisory board from Sanofi Pasteur MSD. GG: Reimbursement and fees for advisory board from bioMérieux, ECDC, OMS, Pfizer, ViforPharma; lecture, training courses: Pfizer, Sanofi Pasteur, Sanofi Pasteur MSD, ViforPharma; invitations to attend national and international conferences: Sanofi Pasteur MSD, bioMérieux, Pfizer, Janssens, Novartis; Grant support from Sanofi Pasteur MSD, bioMérieux, Pfizer studies. PG: Reimbursement and fees for advisory board from AstraZeneca, Bristol-Myers-Squibb, Janssen, Lilly, Lundbeck, Naurex, Otsuka, Roche, Sanofi Pasteur MSD, Servier and Shire. ML: Reimbursement and fees for advisory boards or speakers bureau from Alcon, Allergan, Bausch & Lomb, Sanofi Pasteur MSD, Santen, Thea. FL: Reimbursement and fees for advisory board from Sanofi Pasteur MSD. GP: Sanofi Pasteur MSD, Grünenthal. KS: Grant support from Merck for zoster vaccine study.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Informed consent
For this type of study informed consent is not required.
Additional information
The Herpes Zoster and Functional Decline Consortium list of authors is shown in the Appendix.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
The Herpes Zoster and Functional Decline Consortium list of authors is as follows:
Nadine ATTAL (INSERM U 987 and CETD, Hôpital Ambroise Paré, APHP, 9 Avenue Charles de Gaulle, Boulogne Billancourt, 92100, France; Université Versailles- Saint Quentin en Yvelines, Versailles, France); Claire DEBACK (Service de Virologie, Hôpital Paul Brousse, APHP, Université Paris Sud, Villejuif, 94804, France; INSERM U996, Clamart, 92140, France); Gaétan Gavazzi (Université Grenoble-Alpes, GREPI AGIM, and Clinique Universitaire de Médecine Gériatrique, CHU de Grenoble, Nord Michallon, Boulevard De La Chantourne, La Tronche, 38700, France); Philip Gorwood (CMME, Centre Hospitalier Sainte-Anne, Université Paris Descartes, Paris, France; INSERM U894, 100 Rue de la Santé, Paris Cedex 14, 75158, France), Marc Labetoulle (Service d’Ophtalmologie, CHU Bicêtre, APHP, Université Paris Sud, Kremlin-Bicêtre, 94275, France; Laboratoire de virologie moléculaire et structurale, UPR 3296, CNRS, Gif-Sur-Yvette, 91198, France); François Liard (72 Grand Rue, Saint-Epain, 37800, France); Gisèle Pickering (CHU Clermont-Ferrand, Centre de Pharmacologie Clinique, Clermont-Ferrand, 63003, France; INSERM, CIC 1405, INSERM Neurodol 1107, Clermont-Ferrand, 63003, France; Pharmacologie, Faculté de médecine, Clermont Université, Clermont- Ferrand, 63001, France); Kenneth E Schmader (Durham VA medical Center GRECC and Duke University Medical Centers, Durham, NC, USA).
Rights and permissions
About this article
Cite this article
Herpes Zoster and Functional Decline Consortium. Functional decline and herpes zoster in older people: an interplay of multiple factors. Aging Clin Exp Res 27, 757–765 (2015). https://doi.org/10.1007/s40520-015-0450-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-015-0450-0